Case from: Cruz C, MD1 , Sousa AR, MD2, Madureira AJ, MD3, Pinho T, MD1, Ramos I, PhD3, Pinho P, MD2, Silva Cardoso J, PhD1, Maciel MJ, PhD1
Institute: 1Serviço de Cardiologia, Centro Hospitalar São João; 2Serviço de Cirurgia Cardiotorácica, Centro Hospitalar São João; 3Serviço de Radiologia, Centro Hospitalar São João, Alameda Professor Hernâni Monteiro 4200-319 Porto, Portugal
We report a patient presenting with a massive aortic aneurysm two decades after TOF repair in whom the preoperative CMR assessed the risk of a conventional sternotomy for the planned Bentall operation. The two-step surgical approach, first with a right anterolateral thoracotomy and then a repeat-sternotomy, for the aortic root replacement contributed to the surgical success, minimizing the risk of a potentially fatal iatrogenic aortic rupture.
Clinical history:
A 35-year-old male was followed at our Adult Congenital Heart Disease (ACHD) Clinic with the diagnosis of TOF.
In 1978, by the age of two, he had the diagnosis of TOF with a right aortic arch and underwent a palliative left Blalock-Taussig aortopulmonary shunt (1980). In 1984 a “TOF repair” was performed.
The patient had an uneventful development until adulthood except for a muscular weakness in the legs with abnormal gait which prompted a neurologic evaluation. The electromyography was normal and the screening of the repeat expansions on the DMPK gene excluded Steinert’s disease. The patient was discharged from the neurology department without any further evaluation.
The EKG (Figure 1) showed regular sinus rhythm with a first degree atrioventricular block and an incomplete right bundle branch block (maximal QRS duration 105 msec).
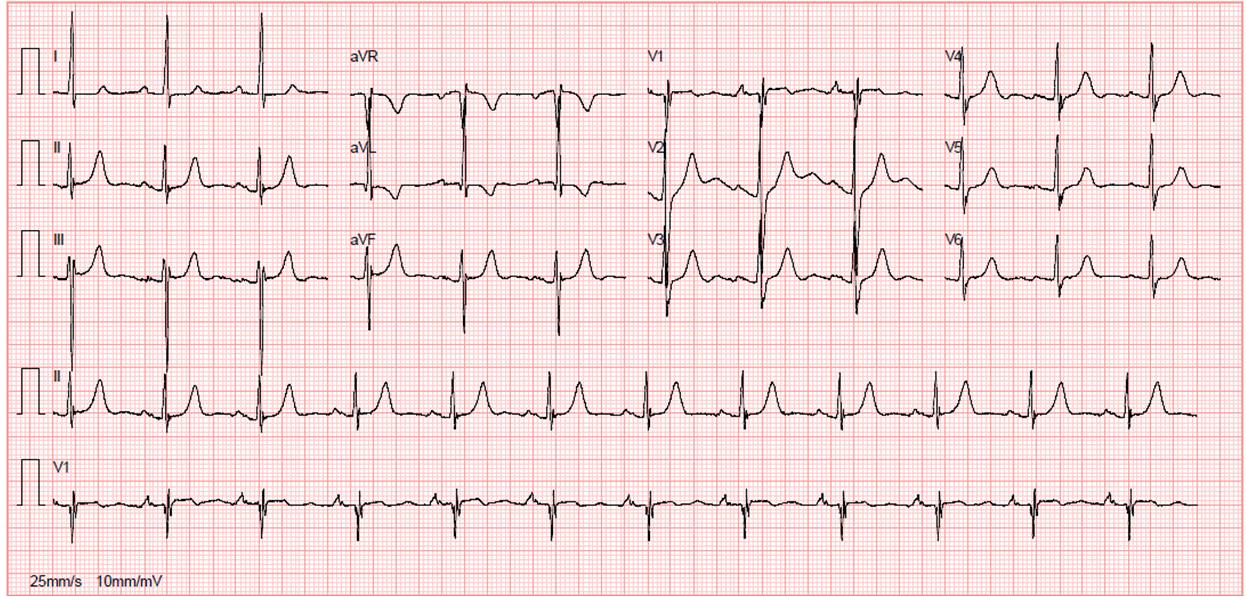
Figure 1: Patient’s EKG showing sinus rhythm with a first degree atrioventricular block and an incomplete right bundle branch block.
The transthoracic echocardiogram (TTE) showed a right aortic arch; right sided cardiac chambers were moderately enlarged; dilated main pulmonary artery (pulmonary annulus 31 mm); pulmonary maximal instantaneous gradient 45 mmHg and a grade III-IV/IV pulmonary regurgitation. There was no residual intracardiac shunt. Normal bi-ventricular systolic function was present.
On serial echocardiographic evaluation, a progressive aortic root and ascending aorta dilatation along with aortic regurgitation was noted from 2002 to 2007 when a routine TTE reported an aortic root diameter of 69 mm and aortic regurgitation grade III/IV.
A magnetic resonance angiography (MRA) was performed that confirmed a massive aneurysm of the aortic root and ascending aorta (maximal diameter 67 mm) with effacement of the sinotubular ridge, extending for 7 cm longitudinally, with preserved dimensions of the aortic arch and descending aorta (Figure 2).

Figure 2: Preoperative 3D reconstruction MRA of the aorta showing the massive aortic root and ascending aorta aneurysm, in a patient with a previous tetralogy of Fallot repair.
No signs of dissection were found. Also, there was impressive adhesion of the anterior aortic wall just beneath the sternum, increasing the risk of a catastrophic bleeding at the time of the sternotomy for the aortic root replacement (Figures 3 and 4).
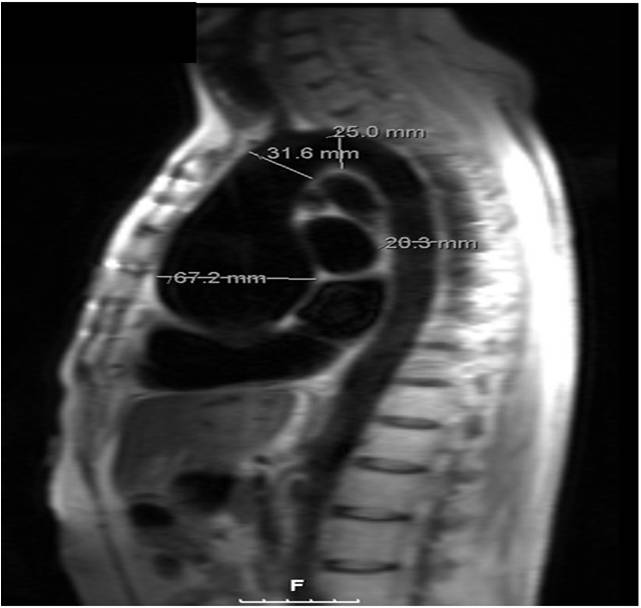
Figure 3: A turbo spin echo sequence of a preoperative magnetic resonance oblique sagittal aorta plane, showing the adhesion of the anterior aortic wall just beneath the sternum.
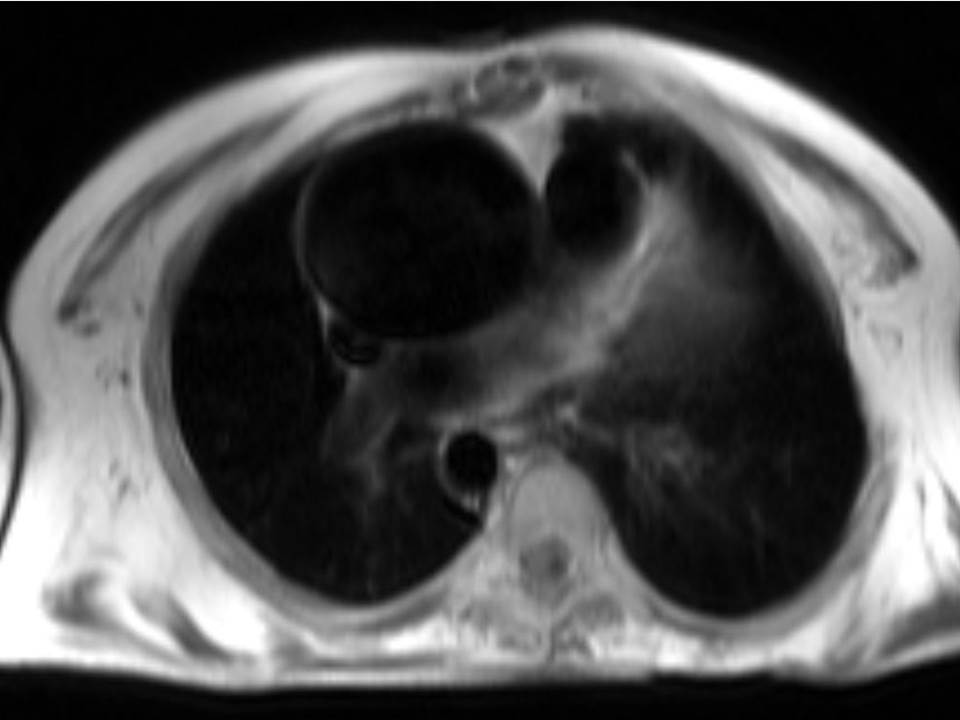
Figure 4: A transverse aorta plane showing the impressive adhesion of the anterior aortic wall to the sternum.
No history of thoracic trauma or chest pain were found. The patient’s blood pressure was always in the normal range.
The patient was sent for cardiac surgery and a Bentall operation was planned. Due to the preoperative CMR findings the surgical approach changed to a two-step procedure, first an anterolateral thoracotomy was performed in order to dissect the scar tissue from the previous sternotomy and carefully separate the anterior wall of the ascending aorta from the sternum adhesions, than a conventional repeat-sternotomy was performed without any aortic wall damage. The aortic root was replaced and a mechanical prosthesis was implanted in the aortic position. Also, the pulmonary valve was replaced by a St Jude 27 mechanical prosthesis and a De Vega tricuspid annuloplasty was done on aorto-bicaval cardiopulmonary bypass. The postoperative recovery was uneventful and the patient was discharged on warfarin with an INR 3-3.5 and aspirin 100mg qd.
The postoperative CMR, performed 3 months after surgery, showed normal aortic dimensions, the ascending prosthetic conduit of 35 mm (Bentall operation), main pulmonary diameter 34 mm (Figure 4).
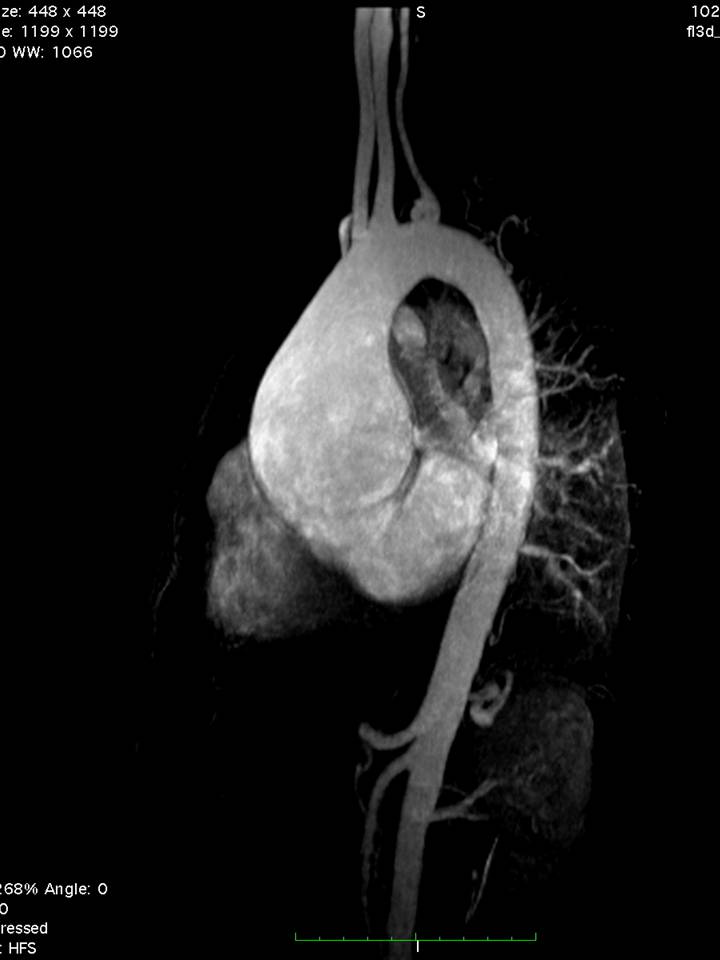

Figure 5: MRA, 3 months after a Bentall operation, preoperative MRA on the left for comparison.
The TTE evaluation, performed 4 months postoperatively, revealed normal diameters of the ascending aorta, aortic arch and descending aorta, mild dilation of the right atrium with normal dimensions of the right ventricle and left cardiac chambers; normal opening of mechanical aortic and pulmonary prosthesis with a maximal instantaneous gradient of 15 and 10 mmHg, respectively. No tricuspid regurgitation was found and a normal bi-ventricular systolic function was present.
The patient is asymptomatic, working full time in a factory and is able to live an almost normal life nevertheless he needs a meticulous follow-up at an expert ACHD centre and a lifelong chronic oral anticoagulation.
Discussion and conclusion
Cardiac surgery improvements and the long-term good results of tetralogy of Fallot (TOF) repair allow adult survival [1] but residual lesions exist and evolve, demanding a meticulous clinical and imaging follow-up. Progressive dilatation of the aortic root after repaired TOF is a recognized complication first described by Capelli et al [2]. It has been postulated that the long-standing left-sided volume overload during fetal life and before complete repair, due to the association of right-outflow obstruction and right-to-left shunt, can be responsible for the progressive dilatation of the aorta. Niwa et al [3] reported that male sex, pulmonary atresia, right aortic arch, and longer time interval from palliative aortopulmonary shunts to repair are possible predisposing factors for aortic dilatation. Possibly intrinsic histological abnormalities in the aortic root and ascending aortic wall, present since infancy in TOF patients, can contribute to this progressive dilatation [4].
Imaging follow-up of TOF patients include chest X-ray, Doppler echocardiography, computerized tomography (CT) scan and cardiovascular magnetic resonance imaging (CMR). However, in patients with associated thoracic deformities and previous cardiac surgeries the ability to obtain an optimal acoustic window for Doppler echocardiography screening is far from perfect and the contribution of the CT scan and CMR in the setting of congenital heart disease imaging has increased rapidly in the past decade. CMR has been shown to be very accurate in the diagnosis of thoracic aortic disease [5], including in TOF patients [6], assessing the entire aorta without exposing the patient to either radiation or iodinated contrast despite the relatively long scan duration. Three dimensional reconstruction of the aorta by contrast enhanced magnetic resonance used as part of the examination of the aorta may however, be a problem in patients with renal insufficiency or during pregnancy. Other potential difficulties in CMR are patients with claustrophobia or non-MRI compatible pacemaker or cardiac defibrillator.
Although patients with repaired TOF commonly have problems with residual pulmonary valve lesions and right ventricular dilatation and systolic dysfunction, the evaluation of the aorta in this subgroup of patients should not be neglected. This case report emphasizes the importance of the aortic root imaging in the follow-up of TOF patients and clearly shows the importance of CMR in the preoperative evaluation of repaired TOF. We report a patient presenting with a massive aortic aneurysm long-term after tetralogy of Fallot repair in whom the preoperative CMR showed impressive adhesion of the anterior aortic wall just beneath the sternum.
The preoperative CMR findings helped the cardiac surgeon in order to plan a different surgical approach, preventing a potential fatal iatrogenic aortic rupture while performing a conventional sternotomy, contributing to the surgical success and the patient survival.
Some case reports of aortic aneurysm and dissection late after repair of TOF [7-9] reinforce this concept and advise regular screening of the aorta in order to promptly diagnose and ultimately to prevent a potential cause of sudden death in this subset of TOF patients.
Perspective
CMR is an important tool for the assessment of congenital heart disease, including the imaging of the aorta in this subset of patients. Moreover, the preoperative evaluation of patients with previous cardiac surgeries requires a meticulous imaging follow-up. CMR provides important imaging findings that can help the cardiac surgeon while facing a reoperation scenario, in order to plan the best surgical approach, minimizing potential perioperative complications. This case report illustrates the role of CMR in this setting.
List of abbreviations
ACHD = adult congenital heart disease; CMR = cardiovascular magnetic resonance; CT = computerized tomography; MRA = magnetic resonance angiography; TOF = tetralogy of Fallot; TTE = transthoracic echocardiogram
Competing interests
None regarding the contents of this manuscript.
Acknowledgements
We thank Dr. Carole Warnes who kindly provided language and writing revision of this manuscript.
References:
- Lillehei CW, Varco RL, Cohen M, Warden HE, Gott VL, DeWall RA, Patton C, Moller JH: The first open heart corrections of tetralogy of Fallot: a 26-31 year follow-up of 106 patients. Ann Surg 1986, 204:490-502.
- Capelli H, Ross D, Somerville J. Aortic regurgitation in tetrad of Fallot and pulmonary atresia. Am J Cardiol 1982, 49:1979-1983.
- Niwa K, Siu SC, Webb GD, Gatzoulis MA. Progressive aortic root dilatation in adults late after repair of tetralogy of Fallot. Circulation 2002, 106:1374-1378.
- Tan JL, Davlouros PA, McCarthy KP, Gatzoulis MA, Ho SY. Intrinsic histological abnormalities of aortic root and ascending aorta in tetralogy of Fallot. Circulation 2005, 112:961-968.
- Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey Jr DE, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM.2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine (developed in collaboration with the American College of Emergency Physicians). J Am Coll Cardiol 2010, 55:e27-129.
- Oosterhof T, Mulder BJM, Vliegen HW, de Roos A. Cardiovascular magnetic resonance in the follow-up of patients with corrected tetralogy of Fallot: a review. Am Heart J 2006, 151:265-272.
- Rathi VK, Doyle M, Williams RB, Yamrozik J, Shannon RP, Biederman RWW. Massive aortic aneurysm and dissection in repaired tetralogy of Fallot ; diagnosis by cardiovascular magnetic resonance imaging. Int J Cardiol 2005, 101:169-170.
- Kim W-H, Seo J-W, Kim S-J, Song J, Lee J, Na C-Y. Aortic dissection late after repair of tetralogy of Fallot. Int J Cardiol 2005, 101:515-516.
- Dimitrakakis G, Oppell UV, Bosanquet D, Wilson D, Luckraz H. Aortic aneurysm formation five decades after tetralogy of Fallot repair. Ann Thorac Surg 2009, 88:1000-1001.
COTW handling editor: Sylvia Chen
Have your say: What do you think? Latest posts on this topic from the forum







