Runyawan Chotenimitkhun, MD MSc
Heart Center, Internal Medicine, Police General Hospital, Bangkok, Thailand
Clinical history:
A 60-year-old, obese woman with diabetes and hypertension presented with dyspnea on exertion and atypical chest pain for weeks. The physical examination was unremarkable. No ischemic changes were observed on the electrocardiogram (figure 1). The sensitive Troponin-T level was less than 50.0 ng/L (0.0-100.0).
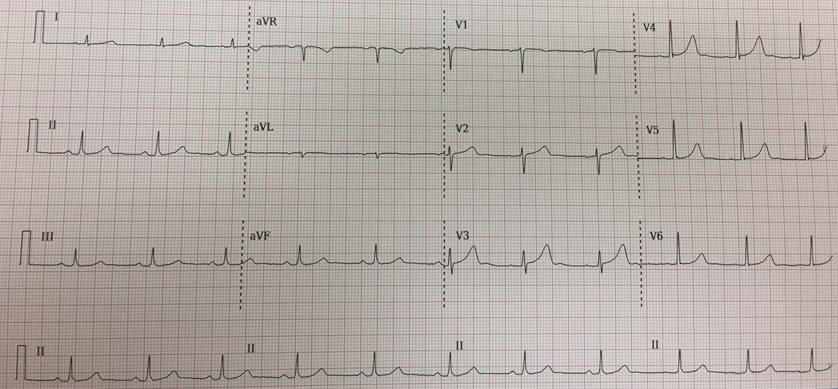
Figure 1. 12-lead ECG depicting normal sinus rhythm without ST-segment changes.
The result of transthoracic echocardiography was limited due to body habitus, however, it revealed normal left ventricular systolic function. The patient was referred to stress cardiovascular magnetic resonance (CMR) to exclude obstructive coronary artery disease (CAD).
CMR findings:
A resting CMR showed normal biventricular systolic function with no regional wall motion abnormalities. An aneurysm and dissection (intimal flap) of the ascending thoracic aorta, consistent with Stanford type A, Debakey type 2 (figure 2), were noted. The entry site of the dissection was above the ostium of the right coronary artery and the dissection terminated prior to the right innominate artery. Because of this finding, adenosine stress CMR was not performed. Moderate aortic regurgitation (regurgitant fraction of 30%) was noted and was believed to be the result of a dilated aortic annulus caused by the ascending thoracic aortic aneurysm. A large 50 x 48 x 49 mm right atrial mass with heterogeneous signal intensity was appreciated.
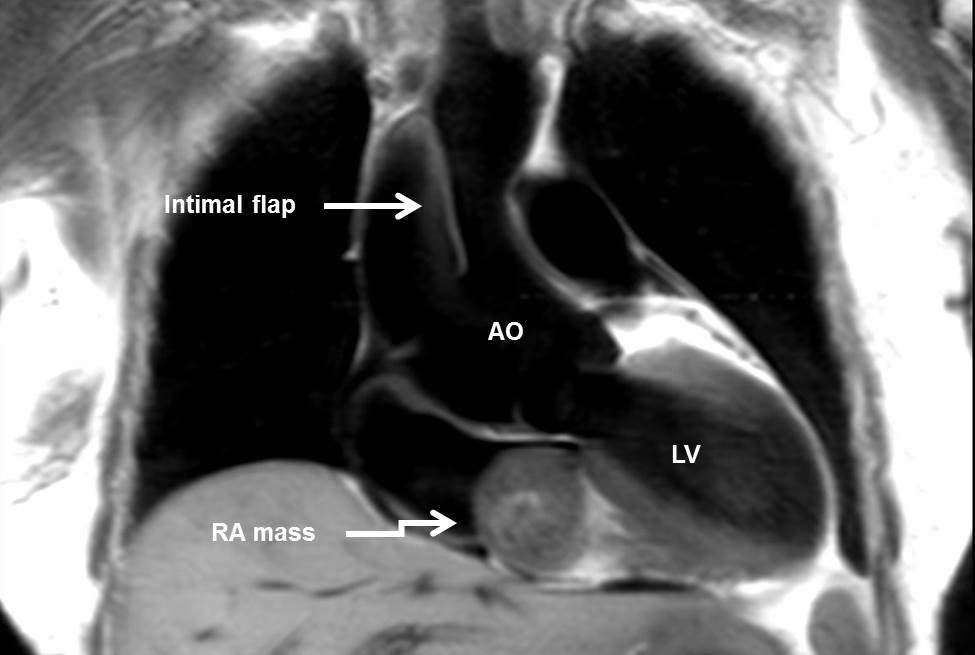
Figure 2. T1-weighted dark blood image depicting an aneurysmal change and dissection (intimal flap) of the ascending thoracic aorta. In addition, a mass is observed in the right atrium with heterogeneous signal intensity relative to myocardium.

Movie 1. Coronal SSFP depicting the aortic valve regurgitation as well as the immobility of the dissection flap.
The mass was attached to the interatrial septum and was without a definite stalk. The mass moved across the tricuspid valve without hemodynamic obstruction as no signal void or abnormal flow was observed (movie 2).
Movie 2. 4-chamber SSFP depicting the large right atrial mass attached to the interatrial septum, moving across tricuspid valve without hemodynamic obstruction.
The mass was isointense relative to the myocardium on T1 weighted spin echo (figure 2) and hyperintense on T2 weighted imaging (figure 3) with the brightness persisting on fat saturation images (figure 4) excluding a fat-originating tumor.
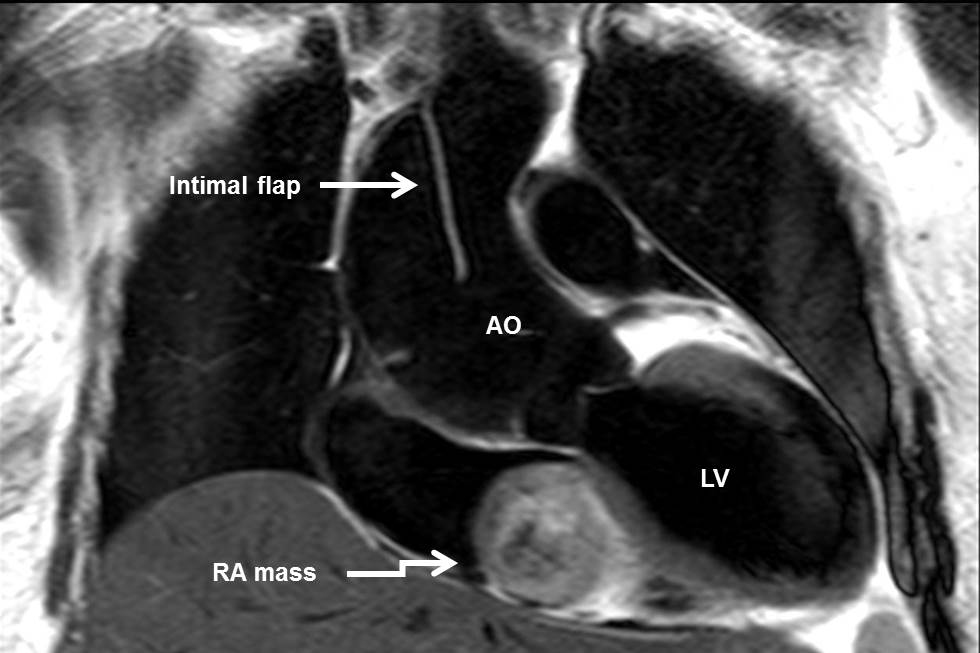
Figure 3. T2-weighted dark blood image showing the RA mass with hyperintense signal intensity.
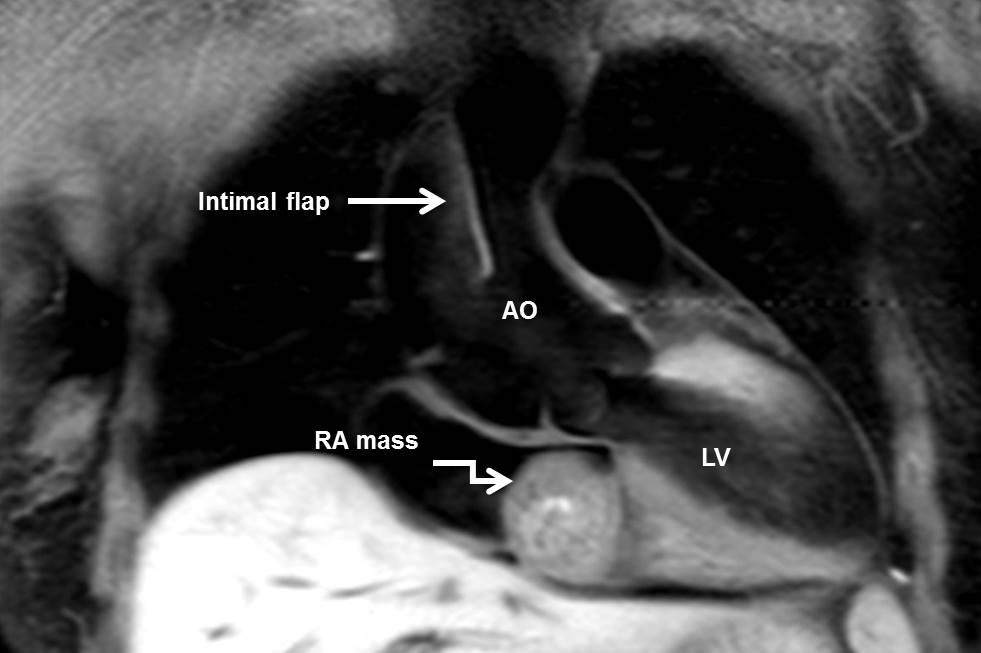
Figure 4. T1-weighted dark blood image with fat suppression showed the brightness persisting and excluded a fat-originating tumor.
The central part of the tumor showed heterogeneous signal intensity on T2 weighted imaging which was consistent with a hemorrhagic and necrotic tumor. There was a peripheral or ring enhancement on late gadolinium images (figure 5). These findings are suggestive of central hemorrhage and necrosis.

Figure 5. Late gadolinium enhanced image showing peripheral enhancement with minimal contrast uptake within central core of tumor, representing central hemorrhage and necrosis. This appearance excluded a thrombus.
Conclusion:
Using comprehensive CMR imaging and clinical correlation, the patient was diagnosed with chronic aortic dissection and a cardiac mass of the right atrium. The individual CMR characteristics such as non-enhancing central tumor following gadolinium administration raises fibroma (central calcification), sarcoma (central necrosis) or organized chronic thrombus (peripheral fibrous content) into the differential diagnosis. The specific location (endocardial/intracavitary, myocardial, or epicardial/pericardial) of the lesion and the main chamber or structure involved were used to narrow down the differential diagnosis.
The patient underwent urgent aortic surgery and the right atrial tumor was removed. The surgery was without complication and she was discharged 2 weeks later. The pathology report of the right atrial mass revealed cardiac schwannoma (figure 6 and 7), which is the most rare cardiac tumor-only 17 cases of this disease have been reported in the literature.

Figure 6. Gross images depicting the tumor as a round encapsulated light brown rubbery mass. The cut surfaces of mass depicted a well-circumscribed area of hemorrhage and necrosis with calcific nodule in the mass. The remaining area of mass was a homogeneous myxoid white and light yellow surface.
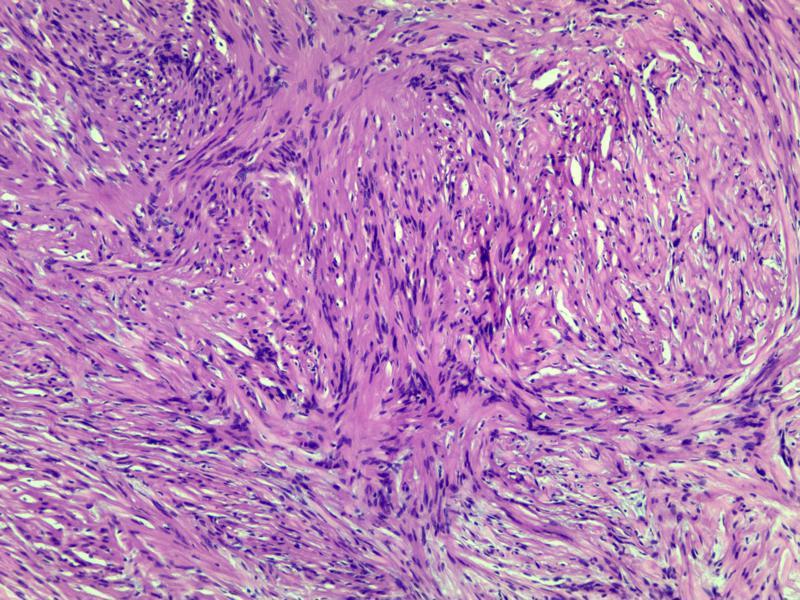
Figure 7. Microscopic sections depicting circumscribed, thick fibrous encapsulated by pseudo-capsule, alternating hypercellular (Antoni A) and hypocellular (Antoni B) areas of low grade spindle cells neoplasm. Occasional nuclear palisading around fibrillary process (Verocay bodies) were found in Antoni A area (H&E stain, 600×800).
Perspective:
Echocardiography usually offers a limited field of view in diagnosing aortic diseases and intracardiac masses. CMR imaging overcomes such issues and has a unique ability of tissue characterization (1-2). However, a definite diagnosis of cardiac tumors can only be completed after histological examination.
Primary cardiac schwannoma is an extremely rare disease (3). It frequently arises from the nervous system of the heart, which resides in epicardial fat and contains both myelinated and unmyelinated axons located on the right side of the heart, particularly in the right atrium and close to the cardiac plexus; however, it can also be found in other sites of the heart (4). Most patients with schwannomas are asymptomatic. If symptoms are present they are related to extrinsic compression, pericardial effusion, valvular obstruction, thromboembolism, heart failure, sudden death, etc (3-5). Some previous cases reported schwannomas as a malignant tumor with an aggressive presentation. They can also have a benign, asymptomatic, non-specific presentation such as in the patient reported here (months to year) as well as in other previously reported cases (5). In this case early detection, smaller tumor size and favorable location likely favored the absence of symptoms. The distinct characteristics of a cardiac schwannoma on CMR is the ring enhancement with minimal contrast uptake within a central core during perfusion study or post-gadolinium enhancement images. This finding corresponded to the gross pathology of encapsulated light brown rubbery mass.
Most patients diagnosed with chronic aortic dissection (onset >90 days) (6) have asymptomatic or non-specific symptoms, similar to this case. The typical findings in CMR of chronic aortic dissection include thickened, immobile, intimal flap, demonstrated in this case but not thrombus in the false lumen. However, the aortic or intimal flap calcification which represent chronicity may not visible by CMR (7). CMR in aortic dissection provides good diagnostic accuracy as to the extent of the disease, localization of entry and re-entry, identification of the intimal flap, and the presence of pericardial effusion, aortic regurgitation, carotid artery dissection and coronary involvement. CMR also does not require ionizing radiation or iodinated contrast (6, 8). However, despite the above mentioned excellent performance of CMR, several methodological and practical limitations preclude the use of this modality in the majority of cases and also in unstable patients (6-8).
Click here to view the CMR images.
References
1. Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S. MR Imaging of Cardiac Tumors and Masses: A Review of Methods and Clinical Applications. Radiology. 2013;268:26-43.
2. O’Donnell DH, Abbara S, Chaithiraphan V, Yared K, Killeen RP, Cury RC, Dodd JD. Cardiac Tumors: Optimal Cardiac MR Sequences and Spectrum of Imaging Appearances. American Journal of Roentgenology. 2009;193:377-387.
3. Serge Koujanian, Bernard Pawlowicz, David Landry. Benign cardiac schwannoma: A case report. Human Pathology: Case Reports.2017;8:24–26.
4. Hwang SK, Jung SH. Schwannoma of the Heart. Korean J Thorac Cardiovasc Surg 2014;47:141-144.
5. Early SA, McGuinness J, Galvin J, Kennedy M, Hurley J. Asymptomatic schwannoma of the heart. Journal of Cardiothoracic Surgery 2007:2:1-3.
6. Erbel R. et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014 Nov 1;35(41):2873-926.
7. Litmanovich D, Bankier AA, Cantin L, Raptopoulos V, Boiselle PM. CT and MRI in Diseases of the Aorta. AJR 2009;193:928–940.
8. Liu Q, Lu JP, Wang F, Wang L, Tian JM. Three-dimensional Contrast-enhanced MR Angiography of Aortic Dissection. RadioGraphics. 2007;27:1311–132.
Case prepared by SCMR Case of the Week Associate Editor: Pranav Bhagirath, Sint Lucas Andreas Ziekenhuis.







