Child N1, Hadi A1, Shambrook J2, Lewis S3, Flett A1, Vassilius T2, Roberts P1
Institutions
1 – Department of Cardiology and Cardiothoracic Surgery, University Hospital Southampton, Southampton, UK
2 – Department of Cardiovascular Imaging, University Hospital Southampton, Southampton, UK
3 – Department of Cardiology, Salisbury District Hospital, Salisbury, UK
Clinical History
A 22-year old Caucasian gentleman was transferred as an emergency to our cardiac surgical center with a large unexplained right ventricular mass, with evidence of a large pulmonary embolus. He had a 6-week history of fevers and rigors following a dental infection and had been admitted to another hospital 10 days previously for investigation. He was otherwise fit and well, with no previous medical history or medications. He had been treated with a course of penicillin V at the time of initial dental infection, and had presented a number of times to his local emergency department in the preceding weeks with fevers, mouth ulcers, pleuritic chest pain and had raised inflammatory markers (white cell count of 18 cells per cubic millimeter of blood with neutrophilia, C-reactive protein (standard assay) of 120 mg/mL, erythrocyte sedimentation rate of 80 mm/hr) with negative blood cultures and no localizing signs of infection.
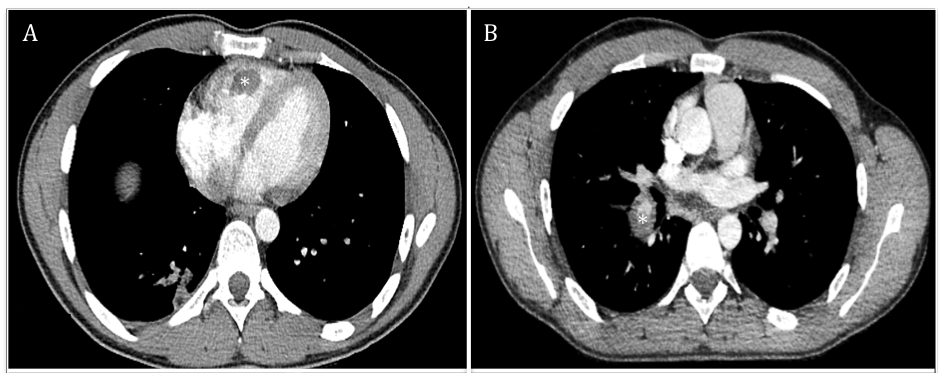
A CT with contrast of his chest, abdomen and pelvis was performed to look for a source of infection which showed a large right ventricular mass and a large filling defect of the right lower lobe pulmonary artery. The right ventricular mass was treated as a large thrombus with low molecular weight heparin, and was thought to be the cause of the pulmonary artery findings. The D-dimer was only mildly elevated at 350 ug/L (normal <250 ug/L).
Below are CT images. On the left is an axial slice of a contrast enhanced CT chest of the at the mid chest level showing a large filling defect in keeping with thrombus (*). On the right is an axial slice at the level of the right lower pulmonary artery showing an occlusive filling defect (*).
Because of continued fevers and raised inflammatory markers, he was also treated for endocarditis with intravenous antibiotics and 10 days later underwent transthoracic and transesophageal echocardiography. This showed the right ventricular mass remained very large despite anticoagulation and had a very unusual appearance, which necessitated transfer for consideration of surgical resection. The heart otherwise appeared entirely normal.
Below is 2D TTE image demonstrating the attachment of the mass to the free wall near the RV apex, with a large more homogenous component clearly shown to be non-adherent to the wall.
A large intracardiac mass or a thrombus in an otherwise normal heart is a very rare finding, which prompted a complete multispecialty review. There was no personal or family history of any bleeding or clotting abnormalities and thrombophilia and clotting screens were unremarkable. There were no systemic features to suggest a malignant process, although this remained a differential diagnosis for the RV mass. The mouth ulcers that were part of the initial presentation remained and an additional scrotal ulcer was found on examination. In addition, a papulopostular lesion appeared at the site of a recent cannula.
CMR findings
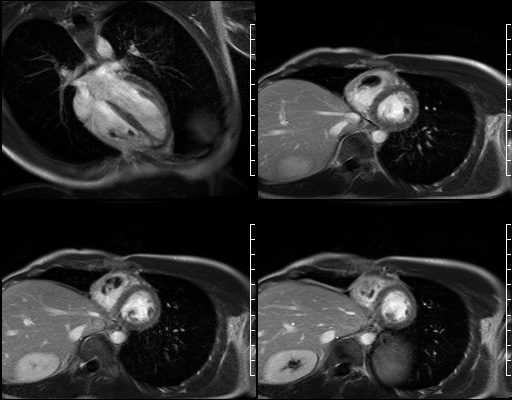
A cardiac MRI was performed on arrival in an attempt to further characterize the RV mass and to identify whether it was a thrombus or a tumor.
Cine CMR (shown below) confirmed the presence of the right ventricular mass and an otherwise structurally normal heart. The RV mass measurements were 39 x 37 x 17 mm and it was tethered to the free wall.
On first pass perfusion (shown below) the mass appeared to be avascular with no enhancement.
On late gadolinium enhancement CMR (shown below), the lesion was predominantly non-enhancing but at the point where the mass was attached to the free wall, there was an area of hyperenhancement.
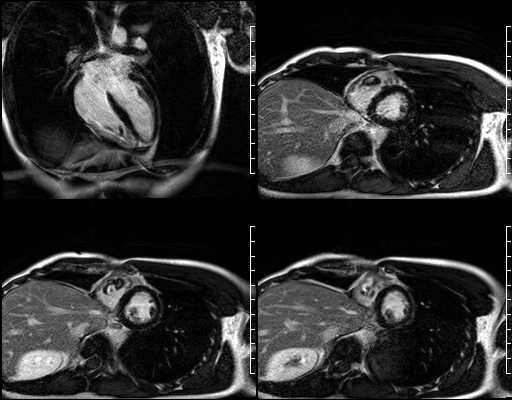
Long TI imaging (see below) was performed at a TI of 440 ms and showed similar findings.
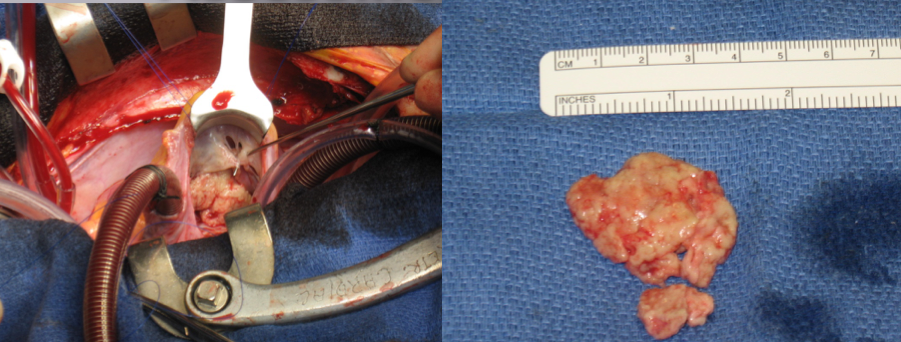
These CMR features were largely characteristic of an inflammatory mass. Because the patient had already suffered from a significant pulmonary embolus and the mass was unchanged despite a period of anticoagulation, the patient underwent surgical removal of the inflammatory mass to prevent further embolic complications. In order to prevent long-term complications from a large incision in the right ventricle, this was performed with collaboration from our congenital surgeons via a right atriotomy following a midline sternotomy. The inflammatory mass had an unusual appearance (shown below); it was white and endothelialized and removed entirely and sent for histology and culture.
Conclusion
The combination of mouth ulcers and a genital ulcer was felt to be suspicious of Behçet’s disease in which a very rare complication is cardiac involvement with inflammatory mass formation due to a local endothelial vasculitic process, and pulmonary artery involvement due to vasculitis leading to pulmonary artery aneurysms and subsequent pulmonary hemorrhage. On further review the initial CT showing the filling defect was felt to be notable because the vessel itself is abnormally thickened, consistent with vasculitis. Initially though there was significant caution in diagnosing this as Behçet’s disease as this would represent such an atypical presentation of a new diagnosis, which is typically a chronic relapsing condition characterized by classical oral, genital and cutaneous signs and symptoms. In addition, Behçet’s disease has a very strong racial predisposition for people from southern Europe and Asia, which our patient was not.
Histopathology from the mass was diagnostic of an inflammatory thrombotic mass and included a large number of degenerating neutrophils. Culture from the mass was negative. All blood cultures were also negative. Further clinical examination of the patient demonstrated that the pustular lesions occurring at the site of intravenous cannulation were a manifestation of pathergy, which is a reactive feature of Behçet’s disease, and subsequent tests showed he was positive for HLA B51, which again is more common in Behçet’s disease.
Based on the overall clinical picture, he was given a unifying diagnosis of cardiac inflammatory mass and pulmonary involvement secondary to Behçet’s disease. He completed a 6-week course of antibiotics and then started treatment for Behçet’s disease, initially with steroids and then cyclophosphamide. He was continued on anticoagulation and made a good recovery.
Perspective
This case illustrates the essential role of CMR in the characterization of abnormal masses. Although the clinical presentation meant an expedited surgical resection was likely regardless, without the CMR mass characterization it is unlikely that the surgeons would have attempted this without a right ventricular incision, which is likely to lead to long term right ventricular impairment. The characterization of the inflammatory mass is based upon the combination of perfusion, long TI and LGE characteristics.
This is a very unusual first presentation of Behçet’s disease. Whilst Behçet’s disease is usually a chronic relapsing oral, genital and cutaneous condition, this case demonstrates the importance of considering the varied systemic manifestations of the disease. Unravelling the underlying etiology proved even more complex in this case where the more characteristic features were only very subtle, and the disease was unusual for our patient’s ethnicity.
Whilst the skin, oral and genital lesions are the most common features of Behçet’s disease, it is important to remember this disease is associated with an increased mortality rate secondary to the more systemic features, mainly because of pulmonary as well as large vessel involvement, neurological involvement and bowel perforation [1]. There are more than 200 published case reports on Behçet’s disease with pulmonary involvement in the literature, and is estimated to occur in 1-8% of Behçet’s disease [2]. The pulmonary arteries are commonly involved, in which pulmonary aneurysms are the most frequently encountered manifestation, in addition to arterial and venous thrombosis, pulmonary infarction and recurrent pneumonia. Aneurysms most commonly occur in the right lower lobe arteries as a result of vasculitis, and there is a tendency of secondary thrombus formation at the site of inflammation. As such, it is likely that the pulmonary artery thrombus in our patient formed secondary to local inflammation rather than because of embolization from the RV inflammatory mass. Aneurysms are associated with a very poor prognosis in Behçet’s disease, with 30% mortality at two years, necessitating further imaging to check on sub-clinical disease progression [1]. Intracardiac manifestations in Behçet’s disease are much rarer, although a few cases of much smaller inflammatory masses have been described previously [3, 4, 5], presumably as a result of a vasculitic process of the endocardium.
Click here to view the entire case on CloudCMR.
Case prepared by Associate Editor: Chetan Shenoy, University of Minnesota
References:
2. Erkan F, Gul A, Tasali E. Pulmonary manifestations of Behçet’s disease. Thorax 2001;56:572-8.





