On October 30, 2015, the Centers for Medicare and Medicaid Services (CMS) issued the Final Rules for the 2016 Medicare Physician Fee Schedule (MPFS) and the 2016 Hospital Outpatient Prospective Payment System (OPPS). The SCMR has completed an initial analysis of these rules to determine the impact on the provision of cardiac magnetic resonance (CMR) services.
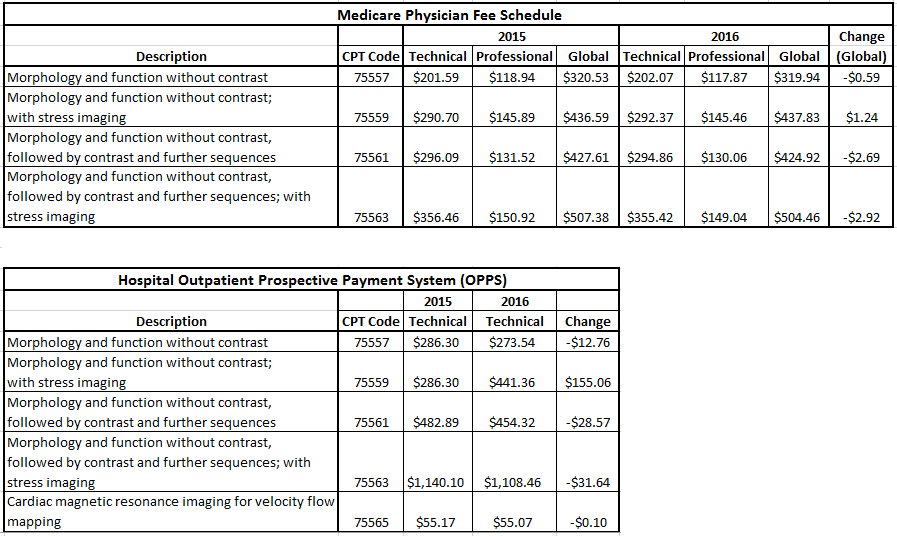
The tables below provide information on reimbursement for the CMR-related CPT codes effective January 1, 2016, for both the Medicare Physician Fee Schedule and the Hospital Outpatient Prospective Payment System. We are pleased to report that the rates are relatively unchanged from 2015, which is a positive outcome in today’s environment of ever decreasing reimbursement. This outcome did not occur without significant effort. Over the past several months, SCMR’s executive leadership, the U.S. Working Group, and SCMR’s advocacy consultants led a concerted effort to oppose a proposed significant cut in the technical component (TC) payment for CPT 75563 – cardiac MRI w/stress imaging and contrast, included in the 2016 OPPS rule. Specifically, CMS had proposed to move CPT 75563 to a proposed new Ambulatory Payment Classification (APC) group – APC 5592, which would have resulted in a reduction in reimbursement of 58 percent, from a 2015 level of $1140.10 down to $474.00.
SCMR’s U.S. Working Group Chair, Dr. Ted Martin, supported by SCMR advocacy consultants, The Korris Group, investigated the reasoning behind the proposed change with the help of data analysis provided by The Moran Company. The group met with CMS representatives and also filed formal comments explaining why the proposed APC placement and associated reimbursement cut was not warranted for CPT 75563. SCMR explained that for reasons of clinical homogeneity and resource use, CPT 75563 should be placed in APC 5593, and thereby retain a reimbursement rate similar to 2015. This opinion was shared by the American College of Cardiology and the American College of Radiology, and both organizations supported the SCMR’s efforts to change the proposed APC designation.
We are pleased to report that CMS recognized the validity of our arguments and in the Final OPPS Rule for 2016 re-assigned CPT 75563 to APC 5593, thereby preserving a more appropriate technical component reimbursement. Under the final rule, the average national reimbursement for the TC of CPT 75563 will be $1108.46, effective January 1, 2016; this represents only a 2.7% decrease from 2015, versus the originally proposed 58% cut.
Additionally, under the MPFS final rule, CMS delayed the proposed January 1, 2017, implementation of the requirement that ordering physicians consult appropriate use criteria (AUC) when ordering advanced diagnostic imaging services such as MR, CT and SPECT. SCMR remains concerned about the lack of regulatory guidance and an unknown implementation date of the AUC requirement. CMS has stated that additional details will be forthcoming in the rulemaking cycles for 2017 and 2018.
We encourage all U.S. SCMR members to work with their institutions to ensure the accurate accounting of all costs involved in the provision of cardiac magnetic resonance services. This is especially important as hospital data inform the hospital outpatient prospective payment system. The OPPS is a prospective payment system, meaning that data reported affect the reimbursement level two years in the future.
Please contact us with questions or concerns. SCMR values each and every member, and we want you to add your voice to advocacy. We thank you for your support.