Michelle Dimza, DO, Diego Moguillansky, MD, MS, Mohammad Al-Ani, MD
University of Florida College of Medicine, Gainesville, Florida, USA
Clinical History:
A 52-year-old woman with myelofibrosis secondary to essential thrombocytopenia underwent allogenic peripheral blood stem cell transplant (PBSCT) with fludarabine-melphalan and anti-thymocyte globulin conditioning two years prior to presentation. Transplant course was complicated by gastrointestinal, skin, and eye graft-versus-host disease (GVHD), fungal pneumonia, essential hypertension, adrenal insufficiency, and stage III chronic kidney disease. She described NYHA Class III symptoms and moderate pleuritic chest pain. Electrocardiogram showed normal sinus rhythm and narrow QRS complex without injury. Transthoracic echocardiogram revealed newly reduced ejection fraction (EF) 30-35% (compared with EF 60-65%, 5 months prior), mild right ventricular (RV) systolic dysfunction, minimal pericardial effusion, and moderately impaired diastolic function. The inferior vena cava was normal in size (1.9 cm) with poor collapsibility. There was no prominent respiratory variation in septal motion or tricuspid or mitral inflow patterns. Brain natriuretic peptide was elevated at 919 pg/mL with baseline renal function and no neprilysin inhibition.
CMR findings:
Cardiac magnetic resonance (CMR) was performed with use of a Siemens Aera 1.5T scanner. CMR showed mild biatrial dilation and biventricular systolic dysfunction (left ventricular EF [LVEF] 32%, RVEF 39%) with normal ventricular size and global hypokinesis. There was LV late gadolinium enhancement (LGE) in the pericardium (Figure 1A). The T1 and T2 bullseye plots demonstrate the distribution of myocardial injury and edema, associated with myocardial dysfunction as assessed by the reduced longitudinal systolic strain (Figure 2). As such, the patient meets modified lake Louise criteria for myocardial inflammation.
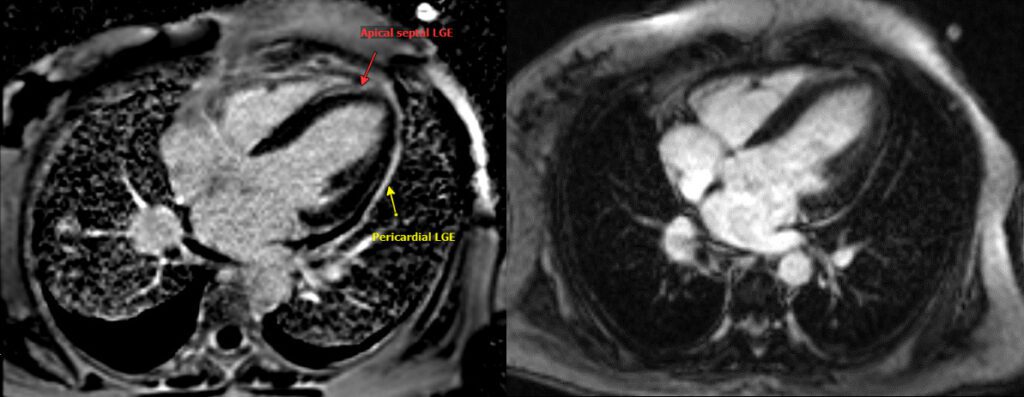
Figure 1: T1 weighted phase sensitive inversion recovery showing late gadolinium enhancement (LGE) 1A: LGE in the apical septum (red arrow) and pericardium (yellow arrow) 1B: follow up scan 8 months later showing resolution of pericardial and myocardial LGE, and regression of the pericardial and pleural effusions. Note that 1A scan was performed on Siemens Aera 1.5 T scanner and 1B was performed on Siemens Prisma 3T scanner. Contrast agent was Gadovist in both scans and 4-chamber LGE sequences were obtained ~ 12 min post gadolinium (0.1 mmol/kg).

Figure 2A: T1 map obtained via Shortened Modified Look-Locker Inversion recovery (ShMOLLI) (T1 lab reference 950-1050 ms). 2B: T2 map (T2 lab reference 42-52 ms.) 2C: Longitudinal strain measured via feature tracking showing globally reduced values (Normal < -18%), with dysfunction more pronounced in the septal areas likely due to ventricular interdependence.
Conclusion:
The CMR findings overall are consistent with myopericarditis. Guideline-directed heart failure therapy using carvedilol, spironolactone, and lisinopril was initiated with close follow-up and titration. Bumetanide was titrated to maintain euvolemia. After multidisciplinary discussion, escalating immunosuppressive therapy was felt to be prohibitively high risk for reactivating fungal infection; accordingly, the patient was maintained on low-dose systemic steroids and topical immunosuppression for treatment of skin and ocular chronic GVHD.
The patient tolerated heart failure therapy and had improvement in heart failure symptoms to NYHA Class II. Repeat cardiac MRI eight months after initial MRI showed improvement in LVEF to low normal with regression of LGE (Figure 1B). There was also normalization of the T2 map. Steroid therapy was weaned off, pneumonia has resolved, and the patient continues to do well one year later.
Perspective:
Chronic GVHD is a known complication of PBSCT, with the most common organs involved being skin, mouth, eyes, and gastrointestinal systems. Cardiac involvement is extremely rare and includes only case reports of myocarditis, acute coronary syndrome, and arrhythmias responsive to immunosuppression.[1] We present a rare case of myopericarditis in a patient with chronic GVHD following PBSCT after discontinuation of immunosuppressive therapy. The cardiac MRI demonstrates myocarditis, pericarditis, and pleurisy as evident by dysfunction, effusions, and edema. The disease affection to serous membranes predisposes to constrictive pericarditis, for which CMR is able to diagnose both acute and chronic cases of.[2] The resolution of pericardial LGE on follow-up is reassuring for absence of chronic pericarditis. In our patient, we found correlation between resolution of heart failure and pleurisy symptoms and the findings of follow up CMR.
GVHD affects up to 80% of stem cell transplant patients depending on risk factors and diagnostic criteria.[3] Keeping a high index of suspicion of cardiac GVHD is important, as it can mimic symptoms of cardiotoxicity from chemotherapy, misleading clinicians to withdraw rather than escalate immunosuppression.[4] Lastly, this case also highlights the value of CMR in follow-up, allowing individualized modification of immunosuppression in a patient cohort at high risk of infectious complications. CMR can be used for post PBSCT patients with cardiac complaints to evaluate for autoimmune, infectious, or medication induced etiologies of cardiomyopathy.
In conclusion, cardiac GVHD can be seen on CMR as myopericarditis with affinity to the septal wall and the pericardium. Follow-up CMR can help follow response to immunosuppression and rule-out chronic pericarditis.
Click here to view initial CMR study on CloudCMR
Click here to view follow up CMR study on CloudCMR
References
- Rackley C, Schultz KR, Goldman FD, et al. Cardiac manifestations of graft-versus-host disease. Biol Blood Marrow Transplant. Oct 2005;11(10):773-80. doi:10.1016/j.bbmt.2005.07.002
- Morley-Smith AC, Cowie MR, Vazir A. Pericardial constriction attributable to graft-versus-host disease: importance of early immunosuppression. Circ Heart Fail. Sep 1 2013;6(5):e59-61. doi:10.1161/circheartfailure.113.000462
- Flowers ME, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. Mar 17 2011;117(11):3214-9. doi:10.1182/blood-2010-08-302109
- Ohmoto A, Fuji S. Cardiac complications associated with hematopoietic stem-cell transplantation. Bone Marrow Transplant. Nov 2021;56(11):2637-2643. doi:10.1038/s41409-021-01427-2
Case prepared by
Jeffrey M. Dendy, MD, FACC
Associate Editor, Cases of SCMR
Vanderbilt University Medical Center





