Berge Sievers* and Berk Sievers*, Burkhard Sievers, MD, FACC, FESC, FSCMR
Department of Internal Medicine
Divisions of Cardiology, Pulmonology, Vascular Medicine, Nephrology and Intensive Care Medicine
Sana Klinikum Remscheid, Germany
*co-first authors contributed equally
Clinical History:
Our 89-year-old grandma has suffered from hypertension, diabetes, dyslipidemia, and severe polyneuropathy for many years. She has been very unsteady with her gait and frequently falls. One day, she fell on her way to answering the front door and sustained a severe laceration to her face above the eyebrow. It took a while until after great effort and under tremendous stress, she was finally able to call our dad. Our dad, a physician, immediately responded and treated the head laceration. Since our grandma did not want to go to the hospital, our dad treated her at home and stayed with her overnight. The next day, she complained of weakness and shortness of breath.
A few days prior to the fall, she also had a fast and irregular heartbeat. She was diagnosed with rapid atrial fibrillation and treated with a beta-blocker. Her pulse decreased and, ultimately, she spontaneously converted into sinus rhythm. However, because our grandma had recurrent rapid atrial fibrillation a few days later, she was started on blood-thinning therapy with apixaban, followed by rhythm-stabilizing therapy with amiodarone.
Four days after her fall, our grandma reported a feeling of pressure on her chest. Her ECG showed R-wave loss and ST-segment elevations over the anterior wall (Figure 1), and the laboratory hs-troponin (0.519 ng/ml, normal range >0.014 ng/ml), as well as NTpro-BNP levels, were markedly elevated (6233 ng/l, normal range <100 ng/ml). An urgent cardiac catheterization revealed a severe narrowing of the left anterior descending coronary artery (Figure 2), treated with two drug eluting stents. 1
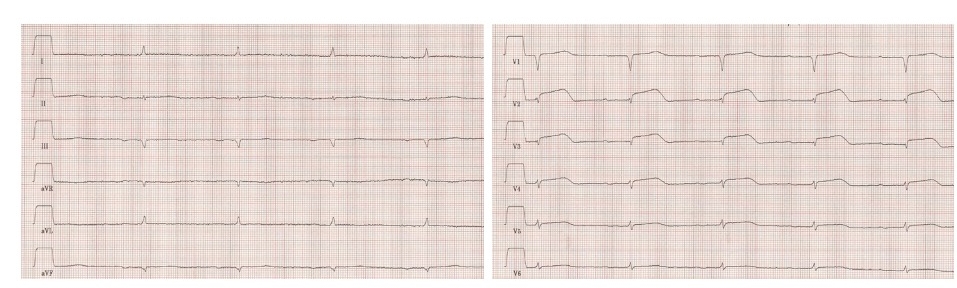
Figure 1. 12-lead electrocardiogram (ECG) on admission. The ECG shows low voltage, R-wave reduction and ST-segment elevation in leads V2-V5 indicating acute myocardial injury.

Figure 2. Coronary angiogram indicating subtotal occlusion of the left anterior descending artery (arrows).
Transthoracic echocardiography showed impaired left ventricular systolic function with severe hypokinesis/akinesis of all mid/distal and apical LV segments. The contractility of the basal segments was preserved. These findings were suggestive of Takotsubo cardiomyopathy (“broken heart syndrome”). To evaluate the likelihood of improvement of left ventricular function and recovery of the wall motion abnormalities, a contrast-enhanced CMR was performed.
CMR Findings
CMR the second day of admission showed highly impaired function of the left ventricle with myocardial thinning and akinesis/dyskinesis of all mid/distal and apical LV segments (Movie 1). T2-TSE imaging revealed global edema of the mid/distal segments (Figure 3). Late contrast enhanced CMR revealed a small myocardial infarction limited to the distal septal and distal anterior segments (Figure 4). Right ventricular systolic function was preserved despite distal free wall hypokinesis. There were no significant valvular abnormalities. There were bilateral pleural effusions indicating cardiac decompensation.
Movie 1. CMR cine imaging in two-chamber, three-chamber, four-chamber, and mid short-axis orientations. There is akinesis/dyskinesis of all mid and distal LV segments. Basal segments are hyperkinetic. Bilateral pleural effusions are present.

Figure 3. Pre-contrast T2-weighted turbo spin echo (TSE) images in short-axis orientation (apical, mid, and basal LV cavity). Increased signal intensity of the myocardium in the apical and mid segments indicates myocardial edema. Basal segments are unaffected.
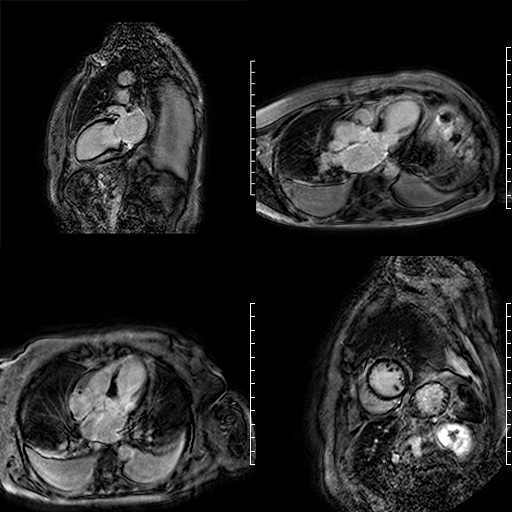
Figure 4. Post-contrast phase sensitive inversion recovery (PSIR) images in two-chamber, three-chamber, four-chamber, and mid short-axis orientations. There is a limited infarction of the distal septal and apical segments.
An ECG performed two days later showed resolution of ST-segment elevation (Figure 5).
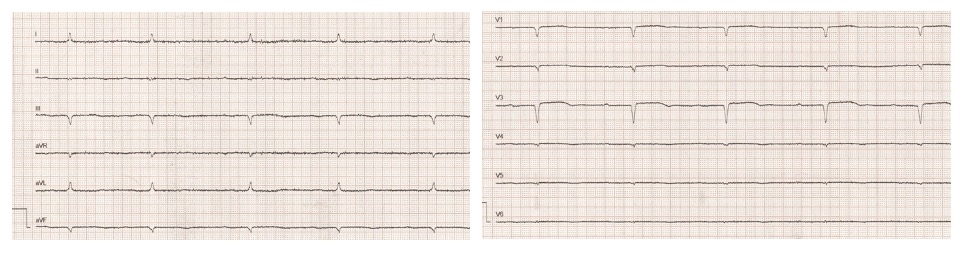
Figure 5. 12-lead ECG. Two days after presentation. Q-waves have developed in the anterior leads and ST-segment elevation has largely resolved.
Three months later, a follow-up CMR revealed normalized left ventricular systolic function (LVEF 59%) and recovered wall thickness (Movie 2, Figure 6). There was only mild residual hypokinesis of the distal septum and apex. The distal RV free wall contracted normally. The limited distal septal and apical infarction was better visualized. An ECG demonstrated R-wave recovery of the anterior wall (Figure 7).
Movie 2. Cine CMR images in two-chamber, mid short axis, three-chamber, and four-chamber orientations. LV systolic function has normalized.

Figure 6. Post-contrast phase sensitive inversion recovery (PSIR) images in four-chamber orientation. Limited late gadolinium enhancement of the distal septal and apical segments persists.
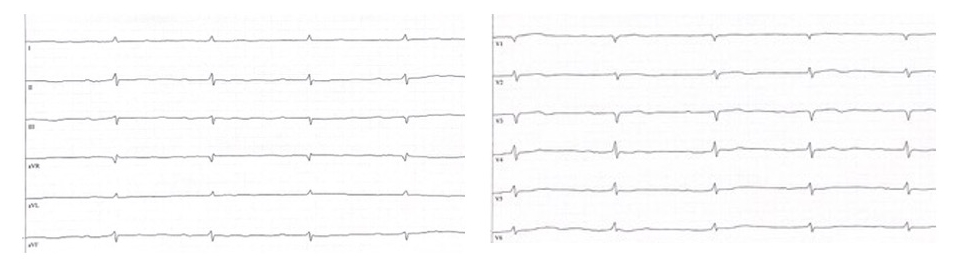
Figure 7. 12-lead ECG three months after presentation. There is recovery of R-wave amplitude in the anterior leads.
Conclusion and Perspective
This case highlights the importance of CMR in the diagnosis and prognosis of heart failure in a rare case of simultaneous occurrence of myocardial infarction and Takotsubo cardiomyopathy. 2 Whether the initial ST-segment elevations were due to a ST-segment elevation myocardial infarction or Takotsubo cardiomyopathy remains unclear. Echocardiography revealed severe LV dysfunction but could not clearly discriminate between these two diagnoses. Tachycardia-induced cardiomyopathy could also have been a contributing factor to the initially severely reduced left ventricular ejection fraction.
CMR showed typical wall motion abnormalities in accordance with stress-induced Takotsubo cardiomyopathy despite the discovery of a small LAD-territory infarction. Myocardial viability of most hypokinetic segments was proven by contrast enhanced CMR. Hypokinesis and myocardial edema involved all mid/distal LV segments including the mid inferior and inferolateral segments that are not typically within the mid-LAD territory. Global edema of mid/distal LV segments has been reported in Takotsubo cardiomyopathy.3 Thus, in this case, regional hypokinesis was not solely due to myocardial stunning from epicardial coronary ischemia. Improvement of systolic function was predicted by the original CMR and proven by the follow-up study.4 CMR was crucial to resolve the differential diagnosis and helped to explore the different causes of diseases leading to severe acute heart failure.5
Three months later, after drug treatment for heart failure according to current guidelines our grandma felt much better and no longer complained of poor performance or shortness of breath. 6 7 She also no longer had a feeling of pressure on her chest. Our dad explained everything to us, and we also researched these topics on our own to understand what was happening to our grandma.
As it is rare that two diseases (myocardial infarction and takotsubo cardiomyopathy) which can singularly cause heart failure simultaneously occurred in our grandma, we wanted to share this case with others. We were impressed that such a poorly pumping heart could recover so well and that CMR accurately predicted the recovery of heart muscle strength.
Note: The patient (the first authors’ grandmother) has given full consent for this publication.
The entire initial CMR study may be viewed on CloudCMR by clicking here.
The entire follow-up CMR study may be viewed on CloudCMR by clicking here.
References:
Case prepared by:
Sean G. Hughes, MD, FSCMR
Associate Editor, Cases of SCMR
Vanderbilt University Medical Center





