Sanja Dzelebdzic MD, Juan Carlos Muniz MD
Nicklaus Children’s Hospital Heart Institute, Miami, FL
Clinical History:
A 16-year-old male presented to our institution for CMR 6 months after an episode of COVID-19 vaccine-related myocarditis (CVAM). He had previously been admitted to an outside hospital with mid-sternal chest pain three days after the second dose of Pfizer-BioNTech COVID-19 vaccine. There was no associated fever, shortness of breath, palpitations, or dizziness. Laboratory work-up revealed elevated inflammatory markers and troponin I level (peak = 9.78 ng/ml, normal value ≤0.08 ng/ml). The work-up was negative for other infectious, rheumatologic and toxicologic etiologies. There was no evidence of other end-organ damage. ECG showed ST segment elevations in precordial leads V4-V6, and no arrhythmias.
Transthoracic echocardiogram showed preserved global left ventricular (LV) systolic function. Coronary angiography demonstrated normal coronary artery anatomy. CMR (images not available) obtained four days after the dose showed a normal LV ejection fraction, elevated T1 and T2 values, and extensive subepicardial and midmyocardial late gadolinium enhancement (LGE) in the LV lateral wall. He was treated with intravenous immunoglobulin. The patient was asymptomatic at discharge, with a significant decrease in troponin level to 0.24 ng/ml.
CMR Findings
CMR obtained six months after the initial presentation showed normal left and right ventricular size and global systolic function (LVEF 64%, RVEF 61%), without evidence of regional wall motion abnormality (Video 1). T2-STIR images demonstrated no evidence of focal edema (Figure 1). Global ECV (29%; reference range 20-32; Kawel-Boehm, JCMR 22:87, Figure 2) and T2 (48 ms) values were normal (Figure 3), however focal ECV elevation was noted in the LV mid lateral wall (41%). Midmyocardial LGE was noted in the LV mid-to-basal lateral wall (Figure 4).

Video 1: Short-axis SSFP cine demonstrating normal left and right ventricular size and global systolic function. No regional wall motion abnormalities noted.

Figure 1: Short-axis T2-STIR images without evidence of focal edema.
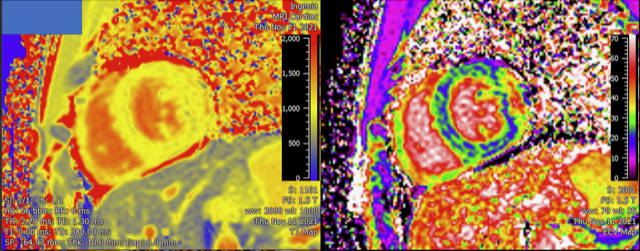
Figure 2: Native T1 (left) and ECV (right) maps demonstrating a regional increase in ECV along the LV free wall.
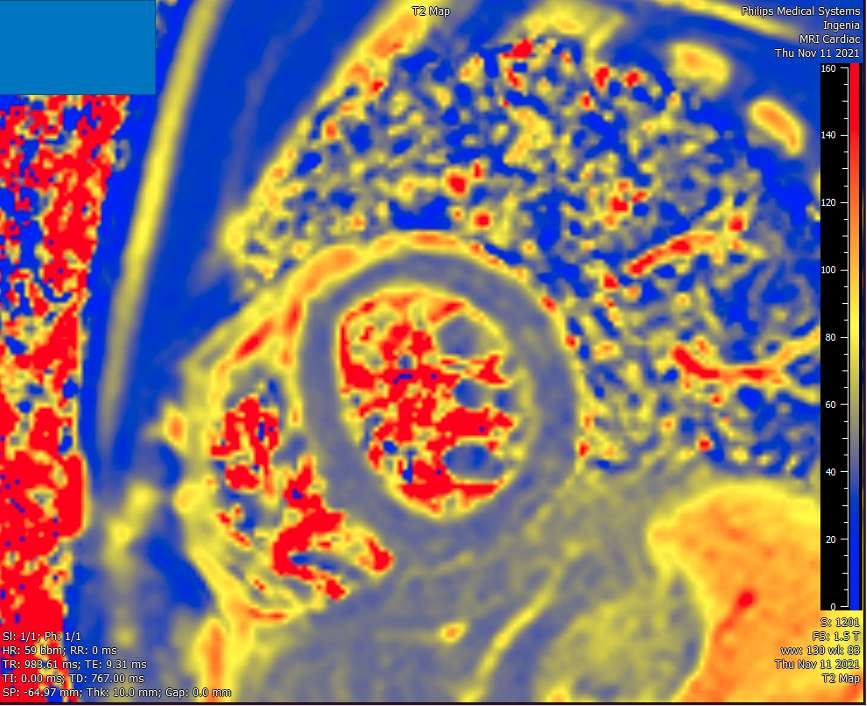
Figure 3: T2 map demonstrating no diffuse edema.

Figure 4: Short-axis (top panel) and 4-chamber (bottom panel) LGE images demonstrating patchy subepicardial and midmyocardial enhancement in the mid-to-basal LV free wall.
Conclusion
These findings are consistent with prior myocarditis with residual fibrosis. During the follow-up period, the patient reported occasional palpitations, however, serial Holter monitors did not reveal any arrhythmia. The long-term implications of residual fibrosis remain unknown, and the patient will require close follow-up.
Perspective
Since the COVID-19 vaccines were approved for children aged 12 and older, multiple reports of CVAM have been published (1-5). CVAM has predominantly affected white adolescent males. The vast majority of cases involved the mRNA vaccines and presented after the second dose. The most common presenting symptom was chest pain. Most patients presented with normal LV systolic function. Two North American multicenter studies have shown that 51-88% of CMR studies in the acute phase met Lake Louise criteria (4-5). Hospital course was relatively benign. Most hospitalizations lasted under a week, without the need for intensive care unit admission or inotropic support. Arrhythmias were rare. These findings differ from other forms of pediatric myocarditis, which overall have a higher rate of LV dysfunction, need for inotropic support, and arrhythmia burden (6). The long-term prognosis of CVAM remains unknown. This case highlights the importance of close follow-up of these patients. The utility of CMR in the diagnosis of myocarditis is well established. In a pediatric population, the typical findings of myocarditis on CMR generally obviate the need for further dedicated coronary angiography. Despite having a relatively benign clinical course and normal echocardiographic evaluations in follow-up period, this patient showed residual fibrosis six months after the onset of CVAM. The clinical significance of LGE after CVAM remains unknown. However, large outcome studies of myocarditis in adults have consistently shown adverse outcomes associated to LGE (7-9).
Click here to view the entire study on CloudCMR.
References
1. Dionne A, Sperotto F, Chamberlain S, et al. Association of Myocarditis with BNT162b2 Messenger RNA COVID-19 Vaccine in a Case Series of Children. JAMA Cardiol. 2021;6(12):1446-1450.
2. Shiyovich A, Witberg G, Aviv Y, et al. Myocarditis following COVID-19 vaccination: magnetic resonance imaging study. Eur Heart J Cardiovasc Imaging. 2021;2019:1-8.
3. Kim RJ, Kim HW, Jenista ER, et al. Patients with acute myocarditis following mrna COVID-19 vaccination. JAMA Cardiol. 2021;6(10):1196-1201.
4. Jain SS, Steele JM, Fonseca B, Huang S, Shah S. COVID-19 Vaccination – Associated Myocarditis in Adolescents. Pediatrics. 2021;148(5):e2021053427.
5. Truong DT, Dionne A, Muniz JC, et al. Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults. Circulation. 2022;145(5):345-356.
6. Law YM, Lal AK, Chen S, et al. Diagnosis and Management of Myocarditis in Children: A Scientific Statement from the American Heart Association. Circulation. 2021;(1):E123-E135.
7. Aquaro GD, Perfetti M, Camastra G, et al. Cardiac MR With Late Gadolinium Enhancement in Acute Myocarditis With Preserved Systolic Function: ITAMY Study. J Am Coll Cardiol. 2017;70(16):1977-1987.
8. Gräni C, Eichhorn C, Bière L, et al. Prognostic Value of Cardiac Magnetic Resonance Tissue Characterization in Risk Stratifying Patients With Suspected Myocarditis. J Am Coll Cardiol. 2017;70(16):1964-1976.
9. Greulich S, Seitz A, Müller KAL, et al. Predictors of mortality in patients with biopsy-proven viral myocarditis: 10-year outcome data. J Am Heart Assoc. 2020;9(16):e015351.
Case prepared by:
Jason N. Johnson, MD MHS
Associate Editor, SCMR Case of the Week
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center, St. Jude Children’s Research Hospital





