Case From: Barbara E. U. Burkhardt, MD, Christian Balmer, MD PhD, Angela Oxenius MD, Emanuela R. Valsangiacomo Buechel MD PhD
Institute: Pediatric Heart Centre, Division of Pediatric Cardiology, University of Zurich, Switzerland
Clinical history:
An 8-year old girl presented with clinical signs of low cardiac output after symptoms of fever and emesis during a few days. ECG revealed a complete atrio-ventricular (AV) block with a ventricular rate of 35 bpm and wide QRS complexes (120 ms) with variable axis deviation and bundle branch block morphology (Figure 1). Transthoracic echocardiography showed normal cardiac anatomy, normal coronary artery origins, but anomalous left ventricular function with hypokinetic mid inferoseptal and apical septal segments and dyskinetic basal and mid inferoseptal segments, the latter also with hyperechogenic myocardium. Laboratory showed neutrophilia of 12 [1.5 – 8.5] G/L, greatly elevated troponin T of 9.54 [<0.014] mcg/L, LDH of 16505 [<236] U/L, NT-proBNP of 17734 [<390] ng/L, and a mildly elevated C-reactive protein of 27 [<10] mg/L.
The patient was placed on continuous cardiorespiratory monitoring, and complete AV-block treated with temporary VVI pacing in the right ventricle (RV) via a transfemorally inserted pacing catheter. AV conduction improved spontaneously one day later, but a bifascicular block persisted (right bundle branch block and left anterior hemiblock)(Figure 2). Two days later, bigeminal ventricular ectopic beats and an episode of non-sustained ventricular tachycardia occurred (Figure 3). Amiodarone was started, and no further episodes of ventricular tachycardia were observed.
The patient was additionally treated with intravenous immunoglobulins and methylprednisolone for suspected myocarditis.

Figure 1: Electrocardiogram: complete AV block
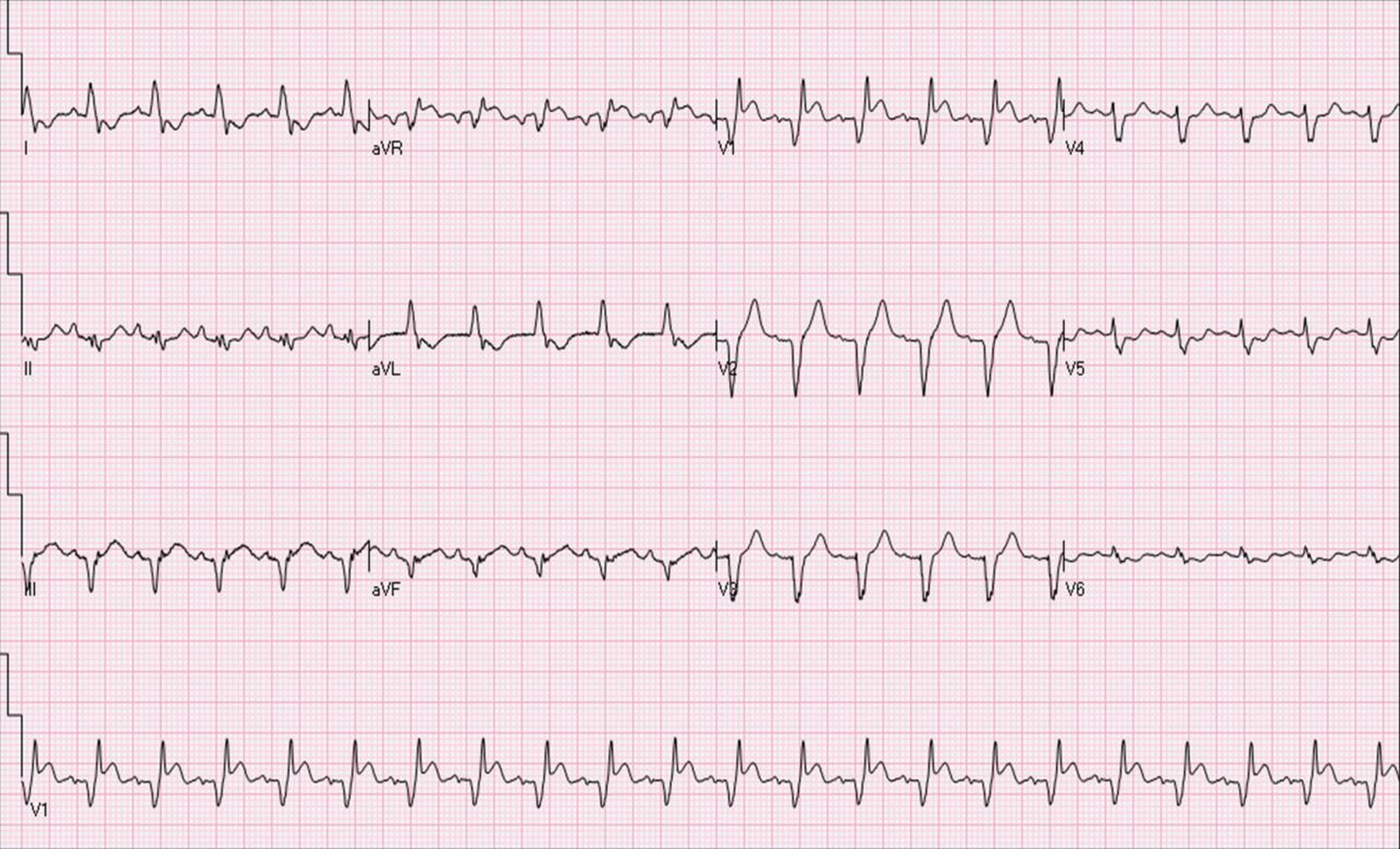
Figure 2: Electrocardiogram: right bundle branch block and left anterior hemi-block
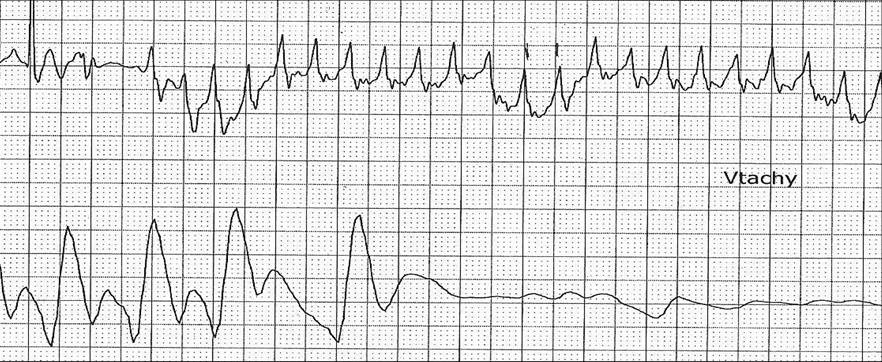
Figure 3: Electrocardiogram (top) and arterial pressure (bottom): ventricular tachycardia
CMR Findings:
Cardiac magnetic resonance (CMR) was performed for assessment of suspected myocarditis [1]. At the first CMR examination, during the acute phase, biventricular function was reduced with ejection fractions of 33% in both ventricles. Cine sequences demonstrated hypokinesia of the left ventricular inferoseptal basal segment and in the right ventricular apex (Movies 1 and 2). In the horizontal long axis, late gadolinium enhancement (LGE) was positive in the basal and mid ventricular septum and the right ventricular apex (Figure 4),
In short axis basal and mid-ventricular slices, LGE was found in the inferior and inferoseptal segments of the left ventricle (LV) as well as the anteroseptal segments on the RV side (Figure 5). The LGE lesions were located along the conduction system and corresponded well with the arrhythmias observed in this patient. No pericardial enhancement was seen, but slight pericardial effusion.

Movie 1: ECG-gated SSFP images in horizontal long axis (four chamber) view showing hypokinesia of the left ventricular inferoseptal basal segment and the right ventricular apex (images were slightly blurred because of arrhythmia)

Movie 2: ECG-gated SSFP images in short axis slices showing thinning and hypokinesia of the left ventricular inferoseptal basal segment
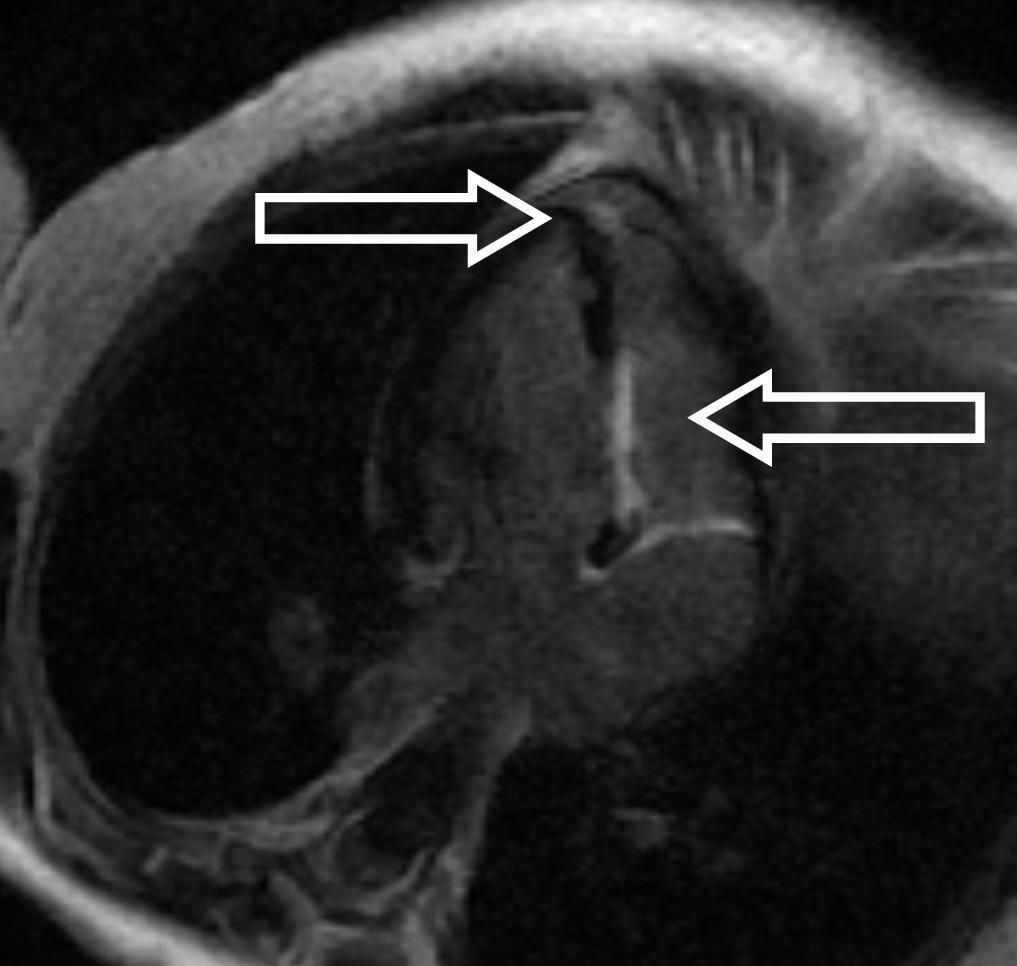
Figure 4: LGE in the basal and mid ventricular septum and the apex (arrows)
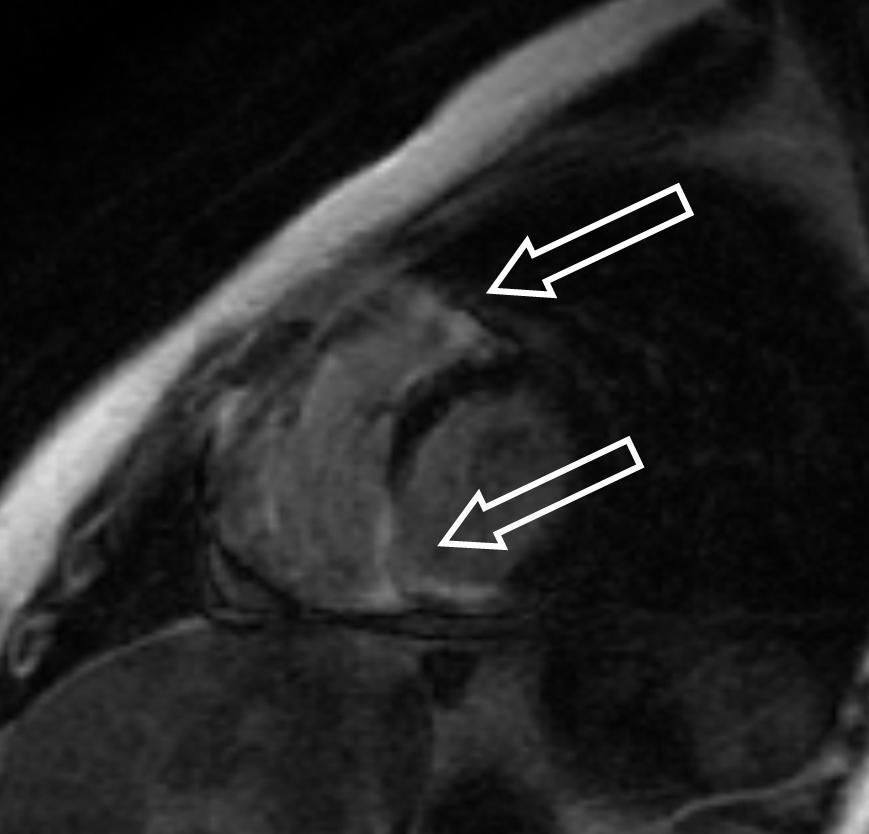
Figure 5: LGE in the basal and mid ventricular septum and the apex (arrows)
Conclusion:
Acute lymphocytic myocarditis was confirmed by endomyocardial biopsy. Coronary angiography revealed normal anatomy and no lesions of the coronary arteries. During follow up, AV conduction recovered further, except for a complete right bundle branch block. Five months later, a follow-up CMR demonstrated improved ventricular function (LVEF 53%) but a persistent scar with inferoseptal thinning and LGE of the left ventricular myocardium (Figure 6).
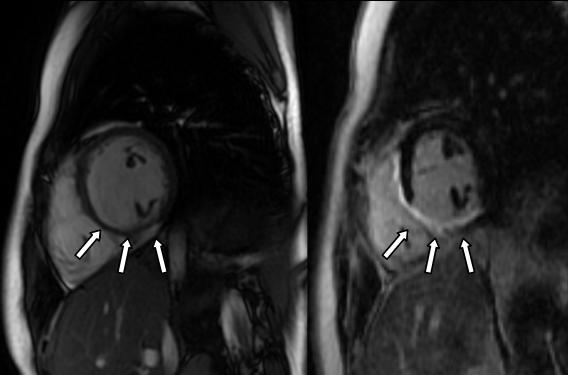
Figure 6: Inferoseptal thinning (left panel) of the left ventricular myocardium and LGE (right panel) in the inferior, inferoseptal, and anteroseptal segments (arrows)
Perspective:
LGE is correlated with inducible ventricular tachycardia and sudden death in many myocardial diseases, such as ischemic, hypertrophic, dilated, or arrhythmogenic right ventricular cardiomyopathy as well as in chronic Chagas’ heart disease [2]. The presence and the extent of LGE is also associated with recurrent tachyarrhythmia and even sudden cardiac arrest [3]. New onset left bundle branch block has been described in patients with myocarditis [4].
We report a case of acute lymphocytic myocarditis with a pattern of LGE correlating with conduction disturbances such as total AV Block, and with ventricular arrhythmia. This case illustrates the ability of CMR to demonstrate the acute changes occurring during myocarditis and by using LGE to show the substrate of electrophysiological disturbances caused by myocardial inflammation. Thus CMR may be used for non-invasive diagnosis of myocarditis also in children, allowing a differentiated treatment strategy, such as conservative watchful waiting for spontaneous resolution of conduction abnormalities without escalation to permanent pacing.
References:
1. Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras A, Laissy JP, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P; International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009 April 28; 53(17): 1475–1487. doi:10.1016/j.jacc.2009.02.007.
2. Mavrogeni S, Petrou E, Kolovou G, Theodorakis G, Iliodromitis E. Prediction of ventricular arrhythmias using cardiovascular magnetic resonance. Eur Heart J Cardiovasc Imaging. 2013 Jun;14(6):518-25.
3. Neilan TG, Farhad H, Mayrhofer T, Shah RV, Dodson JA, Abbasi SA, Danik SB, Verdini DJ, Tokuda M, Tedrow UB, Jerosch-Herold M, Hoffmann U, Ghoshhajra BB, Stevenson WG, Kwong RY. Late gadolinium enhancement among survivors of sudden cardiac arrest. JACC Cardiovasc Imaging. 2015 Apr;8(4):414-23. doi: 10.1016/j.jcmg.2014.11.017. Epub 2015 Mar 18.
4. Mavrogeni S, Sfikakis PP, Karabela G, Stavropoulos E, Spiliotis G, Gialafos E, Panopoulos S, Bournia V, Manolopoulou D, Kolovou G, Kitas G. Cardiovascular magnetic resonance imaging in asymptomatic patients with connective tissue disease and recent onset left bundle branch block. Int J Cardiol. 2014 Jan 15;171(1):82-7. doi: 10.1016/j.ijcard.2013.11.059. Epub 2013 Dec 4.







