Case from: Robert Huggett, Christina Kamperou, William Moody.
Institute: Department of Cardiology, Russell’s Hall Hospital, The Dudley Group of Hospitals, UK.
Clinical history: A 23 year old gentleman presented to the coronary care unit with “dull aching” central chest pain without pleuritic or pericarditic features. His diagnosis of Eosinophilic Granulomatosis with Polyangiitis (eGPA) had been made last year because of severe extrinsic/allergic asthma associated with paranasal sinus inflammation, high peripheral blood eosinophilia and typical pulmonary infiltrates seen on thin slice CT thorax. His eGPA status was said to be quiescent (CRP= 4mg/l) on long-term prednisolone and cyclophosphamide. He had tested negative for ANCA serology. The presentation ECG showed subtle inferolateral ST elevation. An initial working diagnosis of myo-pericarditis secondary to eGPA was made, but four consecutive day highly-sensitivity Troponin I levels (Normal reference range 0-100 ng/L) were: 653, 24708, 14689, 4588. Given some uncertainty in the history and initial investigations, a cardiac MRI was requested to make clear the diagnosis.
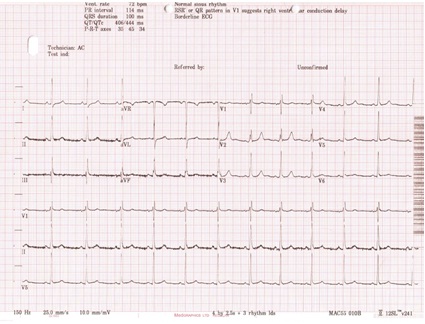
Figure 1. ECG on presentation

Figure 2: CXR on presentation showing clear lung fields and apparent disease remission.
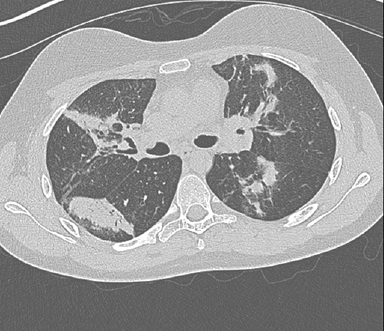
Figure 3: Thin slice CT Thorax done a year before on the same patient showing bilateral random parenchymal consolidation.
CMR Findings: The CMR images showed there was mild LV systolic impairment caused by a transmural inferolateral infarct (LCx terrotory) with signs of adverse microvascular obstruction and myocardial oedema. There was also a small distant LAD territory infarct in mid anteroseptal wall.
Full MRI data: https://www.cloudcmr.com/4730-0002-3818-5374 (best visualized in Google Chrome)
Movie 1
Movie 2
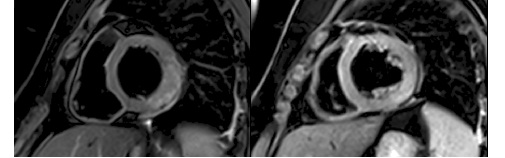
Figure 5: T2 weighted STIR oedema imaging: showed increased SI in the basal to mid inferolateral segments extending just outside the infarct zone.
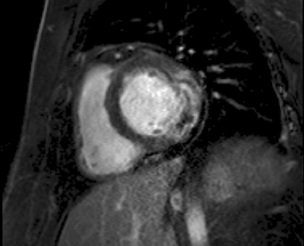
Figure 6: Early Gadolinium enhancement imaging: Shows signs of adverse microvascular obstruction.
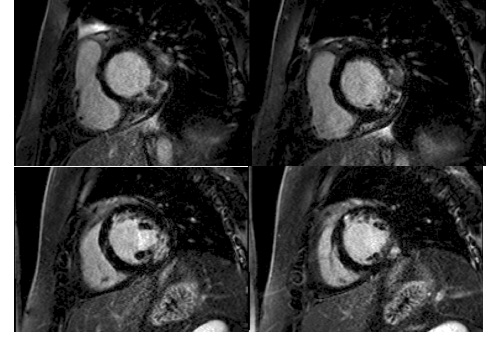
Figure 7: Late Gadolinium imaging: shows infarction/scar in two distinct coronary territories
A catheter coronary angiogram was then done which showed small saccular aneurysms, muscle bridging in LAD and signs of distal occlusions of PLV, septals, and distal OM branches.
Movie 3

Movie 4
Conclusion:This case demonstrates the range of cardiac involvement in Churg-Strauss syndrome is beyond that of cardiac hypereosinophilia characterised by myocarditis, endomyocardial fibrosis, intracardiac thrombus and heart failure. Coronary arteritis and acute infarction is increasingly reported in these patients1,2. Churg-Strauss syndrome is primarily characterised by vasculitis affecting both small and medium-sized blood vessels. Cardiac findings are present in about 50% of cases and are responsible for almost half of all deaths3. Cardiac involvement is reported to be more frequent in the ANCA- negative phenotype4. It has also been shown that the cardiac involvement is common even when their vasculitis is in clinical remission as was seen in this highlighted case5. CMR scanning this patient helped differentiate eosinophilic myocarditis from myocardial infarction by using tissue characterisation and the coronary pattern of late enhancement. The patients therapy was changed to off label use of Rituximab (a monoclonal antibody to CD20) in addition to usual guideline directed therapy post MI. It could be advised to do CMR on all (especially ANCA negative) eGPA patients at diagnosis, as cardiac involvement in this vasculitis, is largely undetected by other non-invasive imaging techniques and CMR could guide treatment and risk assessment 6,7.
References:
- Triantafyllis AS et al. Churg-Strauss syndrome masquerading as an acute coronary syndrome. Am J Emerg Med. 2015;33:313.
- Sulaiman W et al. Acute myocardial infarction as Eosinophilic granulomatosis with polyangiitis (formerly Churg Strauss syndrome) initial presentation]. Rev Bras Reumatol. 2014;54:393-6.
- Guillevin L et al. Churg–Strauss syndrome: clinical study and long-term follow-up of 96 patients. Medicine (Baltimore). 1999;78:26-37.
- Mavrogeni S et al. Cardiac involvement in ANCA (+) and ANCA (-) Churg-Strauss syndrome evaluated by cardiovascular magnetic resonance. Inflamm Allergy Drug Targets. 2013;12:322-7.
- Dennert RM et al. Cardiac involvement in Churg-Strauss syndrome. Arthritis Rheum. 2010;62:627-3
- Mavrogeni S et al. Cardiovascular magnetic resonance for evaluation of heart involvement in ANCA-associated vasculitis. A luxury or a valuable diagnostic tool? Inflamm Allergy Drug Targets. 2014;13:305-11.
- Dennert RM et al. Cardiac involvement in Churg-Strauss syndrome. Arthritis Rheum. 2010;62:627-3





