Case from: Alice Wood, MBBS1, Gerry P McCann, MBChB, MD2, Elved Roberts, MBChB, MD1
Institute: 1. Glenfield Hospital, University Hospitals of Leicester, Groby Road, Leicester LE3 9QP
2. NIHR Leicester Cardiovascular Biomedical Research Unit, Department of Cardiovascular Sciences,
Clinical Sciences Wing, Glenfield Hospital, Groby Road, Leicester LE3 9QP
Clinical history: A 74 year old lady presented with several hours of “heavy” central chest pain, associated with sweating and nausea. ECG revealed deep anterolateral T wave inversion , and initial high sensitive troponin I was 7000ng/L (normal range <20ng/L). She was a current smoker but had no other known cardiovascular risk factors, and there was no relevant family history.
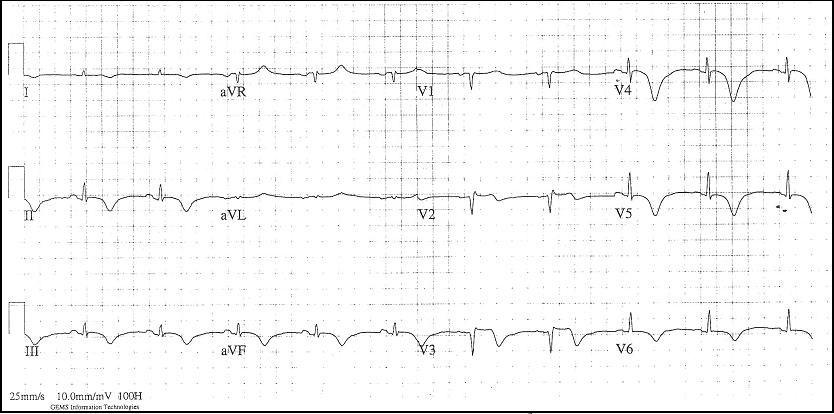
Figure 1: Electrocardiogram revealing deep anterolateral T wave inversion
She was given standard treatment for an acute coronary syndrome, including aspirin and clopidogrel, and was listed for cardiac catheterisation. This revealed moderate mid left anterior descending (LAD) disease, moderate to severe mid circumflex disease, and marked mid ventricular and apical “ballooning” with dynamic basal segments on left ventriculography.
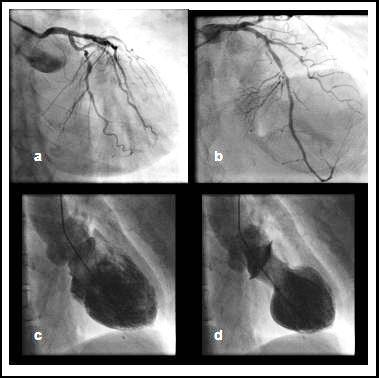
Figure 2: Coronary angiogram and left ventriculography showing a) severe mid circumflex lesion, b) moderate mid LAD disease, c) LV diastole, and d) LV systole
Echocardiography within several hours confirmed severe left ventricular (LV) systolic impairment with apical ballooning. The differential diagnoses at this stage were that she had either had an anterior descending territory infarct with spontaneous recanalisation, or that she had Takotsubo cardiomyopathy with incidental non-obstructive coronary disease. Her history was reassessed and even with direct questioning she was unable to recall any recent stressful events that might have triggered an episode of Takotsubo cardiomyopathy.
She was discharged home 3 days after admission on aspirin, clopidogrel, ramipril, bisoprolol, eplerenone and atorvastatin. She underwent outpatient stress cardiac MRI three weeks later in order to evaluate the functional significance of the coronary lesions found, and to assess for reversible myocardial dysfunction and myocardial infarction.
CMR Findings: The MRI demonstrated features of apical hypertrophic cardiomyopathy with no evidence of the apical ballooning previously seen or other wall motion abnormalities. There was no reversible ischaemia, however there was a small area of lateral apical wall late gadolinium enhancement compatible with a small myocardial infarction in the distribution of the circumflex artery.

Video 1: Left ventriculogram (left) at time of presentation and cardiac MRI (right) performed three weeks after presentation demonstrating recovery of left ventricular function; apical thickening can also be seen on the CMR
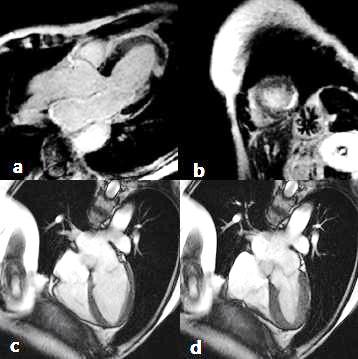
Figure 3: Cardiac MRI with late gadolinium contrast a) 3 chamber view and b) apical short axis both showing apical lateral enhancement. SSFP 4 chamber view in c) end diastole and d) end systole both showing apical hypertrophic cardiomyopathy; note apical segments are thicker than basal segments in diastole
Conclusion: Our hypothesis therefore is that this lady had a small myocardial infarction (due to circumflex acute coronary pathology) which acted as a stressor triggering Takotsubo cardiomyopathy. The resulting severe but totally reversible LV dysfunction is out of keeping with her non-obstructive anterior descending coronary disease. The diagnosis was further complicated by her apical hypertrophic cardiomyopathy, which may explain the fixed anterolateral ECG changes [2], which were initially attributed to ischaemia or Takotsubo cardiomyopathy.
Perspective: Takotsubo cardiomyopathy is reported to occur in patients with normal coronary arteries. This case demonstrates occurrence in a patient with non-obstructive anterior descending disease, in whom the transient severe apical/mid wall ballooning was markedly disproportionate to the degree of lateral wall infarction attributable to the circumflex lesion. Takotsubo cardiomyopathy has previously been reported in association with other severe medical illness, including myasthenic crisis [3], but has not previously been reported coincidentally with myocardial infarction in a territory which would not explain the wall motion abnormalities. The diagnosis of apical hypertrophic cardiomyopathy, which is in itself associated with ECG abnormalities, further complicated the picture. This case highlights the importance of keeping an open mind when managing patients with unusual presentations- there may be more than one unifying diagnosis!
References:
1. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E: Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J 2006 27: 1523–1529.
2. Moon JC, Fisher NG, McKenna WJ, Pennell DJ: Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart 2004 90: 645-649.
3. Thornhill L, Raybould A, Anderson R: Takotsubo cardiomyopathy in a patient with a myasthenia gravis crisis. Cardiology News Dec/Jan 2013, 13-14.
COTW handling editor: Kevin Steel
Have your say: What do you think? Latest posts on this topic from the forum







