Case from: Kapildeo Lotun, MD*, W Kyle Stribling, MD**, Hem L Bhardwaj, MD**, Derek Brinster, MD*** and John D Grizzard, MD+
Institute: *Department of Cardiology, Sarver Heart Center, University of Arizona, Tucson, AZ; **Department of Medicine-Cardiology, Virginia Commonwealth University, Richmond, VA; ***Department of Cardiothoracic Surgery, Virginia Commonwealth University, Richmond, VA; +Department of Radiology, Virginia Commonwealth University, Richmond, VA
Clinical history: A 69 year-old male with history of endovascular abdominal aortic aneurysm repair, COPD, and metastatic lung cancer status post resection on radiation therapy was referred to a cardiothoracic surgeon for consideration of aortic valve replacement (AVR) after a routine transthoracic echocardiography (TTE) at an outside facility revealed evidence of severe aortic stenosis (AS) with a peak gradient of 105 mmHg and aortic valve area (AVA) of 0.78 cm2. Despite these findings, the patient exercised up to 90 minutes daily, walking 3-4 miles, riding a bicycle, or going to the gym without angina, syncope, or presyncope. His only symptoms were nonspecific dyspnea and fatigue. He was referred for cardiac magnetic resonance imaging (CMR) to evaluate AS because his echo findings were felt to be out of proportion to his symptoms.
CMR Findings: CMR revealed a congenital bicuspid aortic valve with a central bridge of tissue between the cusps creating 2 valve orifices [Movies 1 & 2- Figures 1 & 2].

Movie 1
CMR short axis view of the aortic valve
showing the congenitally bicuspid valve fused
with a bridge of tissue creating 2 separate orifices
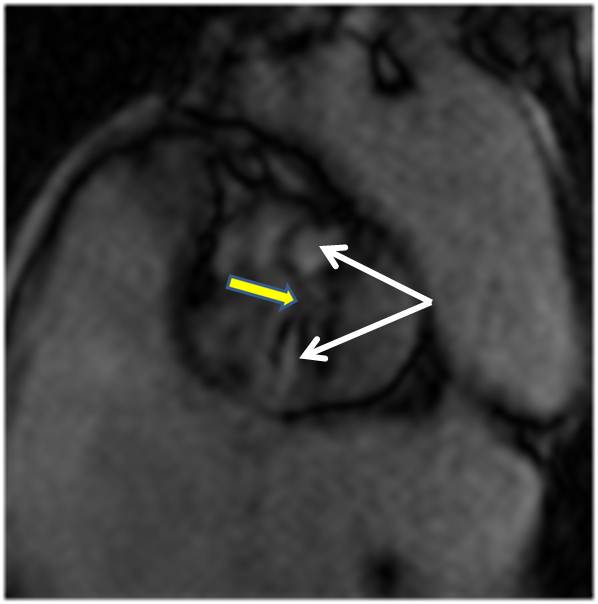
Figure 1: CMR short axis cine view of the aortic valve showing the congenitally bicuspid valve fused with a bridge of tissue (solid arrow) creating 2 separate orifices (arrows)

Movie 2 CMR lateral view of the aortic valve and proximal aorta showing 2 jets of flow through valve into aorta confirming flow through each orifice.

Figure 2: CMR lateral cine view of the aortic valve and proximal aorta showing 2 jets of flow through valve into aorta (arrows) confirming flow through each orifice.
While the individual areas of each orifice were consistent with severe AS, the effective total AVA by planimetry was 1.3 cm2 [Figure 3].
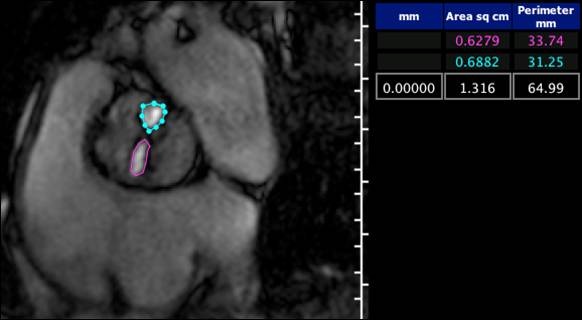
Figure 3: Planimetry of the individual orifices is consistent with severe stenoses, but the sum of the valve areas makes the valve only moderately stenotic.
A subsequent trans-thoracic echo at our institution was unable to accurately assess AS severity, again showing evidence of severe AS [Movies 3 & 4] with an AVA of 1.0 cm2, peak gradient of 93 mmHg, and mean gradient of 55 mmHg [Figure 4].

Movie 3 & Movie 4
TTE short axis view of aortic valve showing a TTE short axis view of aortic valve with color thickened calcified valve that appears stenotic. showing no definite evidence of 2 valve orifices or TTE is unable to define the “Alfieri” appearance of the valve. or dual flow.
The average peak gradient of 93 mmHg across the valve is a reflection of the outflow gradient across each individual orifice but cannot be used to accurately assess AS severity since there are 2 separate orifices [Figure 4].
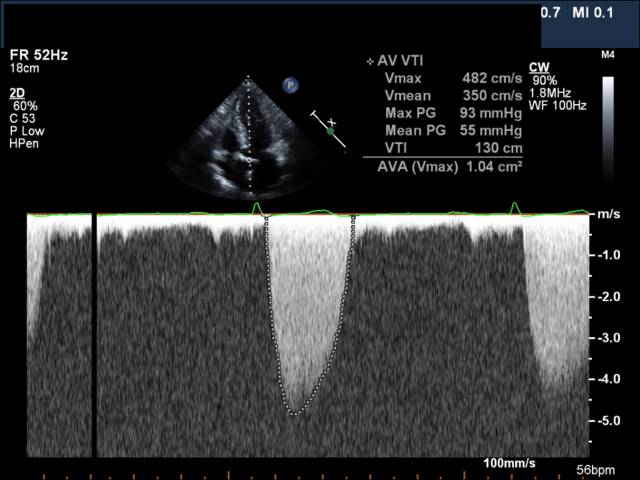
Figure 4: TTE Doppler of velocity through aortic valve and subsequent calculations of gradients and AVA.
Conclusion: The error by TTE was secondary to poor visualization of a calcified aortic valve and calculations based on flow through 1 of 2 valve orifices. Based on CMR findings and lack of symptoms, AVR and valvuloplasty were avoided in this patient.
Perspective: In this case, the TTE evaluations of AS resulted in incorrect measurements with an underestimation of the gradient usually due to measurement error, low output, or paradoxical low flow (1). This case represents an overestimation of the severity of AS by TTE due to unusual dual orifice aortic valve anatomy that was ultimately defined on CMR. In 1995, Alfieri described a surgical technique for improving mitral regurgitation in patients with mitral valve prolapse, whereby the prolapsed leaflet is anchored to the non-prolapsed leaflet in and “edge-to-edge” fashion. In the case of a medial anterior leaflet prolapse, this procedure resulted in a double orifice mitral valve that has come to be known as an “Alfieri” mitral valve (2). A short axis view of the aortic valve in this case has a similar appearance, leading us to call this a pseudo-“Alfieri” aortic valve. To our knowledge, this phenomenon has never previously been described.
References:
1. Dumesnil JG, Pibarot P and Carabello B. Paradoxical low flow and/or low gradient severe aortic stenosis despite preserved left ventricular ejection fraction: implications for diagnosis and treatment. Eur Heart J 2010;31:281-289.
2. Fucci C, Sandrelli L, Pardini A, Torracca L, Ferarri M and Alfieri O. Improved results with mitral valve repair using new surgical techniques. Eur J Cardio-thorac Surg 1995;9:621-627.
COTW handling editor: Monica Deac
Have your say: What do you think? Latest posts on this topic from the forum







