Case from: Uyen T. Truong, MD; Brian Fonseca, MD
Institute: Division of Cardiology, Children’s Hospital of Colorado; University of Colorado, Denver
Clinical history: The patient is a previously healthy 9 year-old child, who presented to her primary care doctor with complaints of her feet turning white. In addition she was noted to have a murmur and hypertension. Echocardiographic evaluation by a Pediatric Cardiology specialist was concerning for a bicuspid aortic valve and possible interruption of the aortic arch. A referral for a cardiac MRI was arranged to further evaluate the aortic arch.
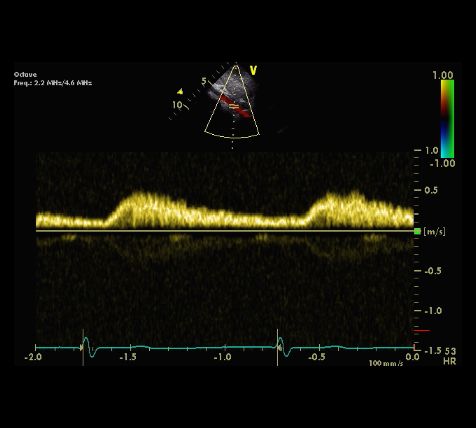
Suprasternal echocardiographic image (2D and color Doppler) indicating concern for obstruction within the descending aorta. Spectral Doppler of the abdominal aorta indicating forward flow in diastole and diminished amplitude.
CMR Findings: The study was performed on a Siemens Avanto 1.5 Tesla scanner using the 6-element body matrix coil/spine coil under general anesthesia.
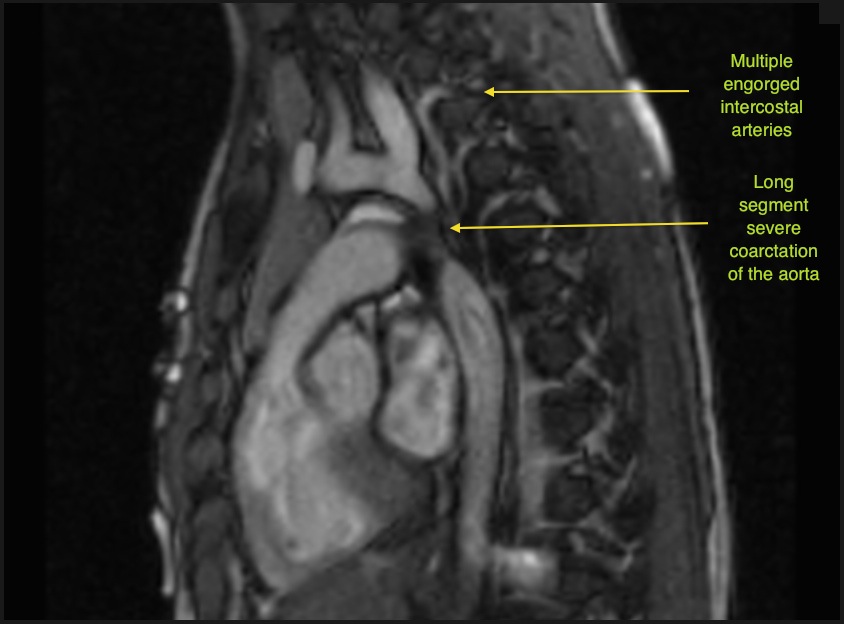
Parasagittal SSFP single shot imaging: shows apparent interruption of the aortic arch distal to the origin of the left subclavian artery and multiple dilated intercostal arteries.
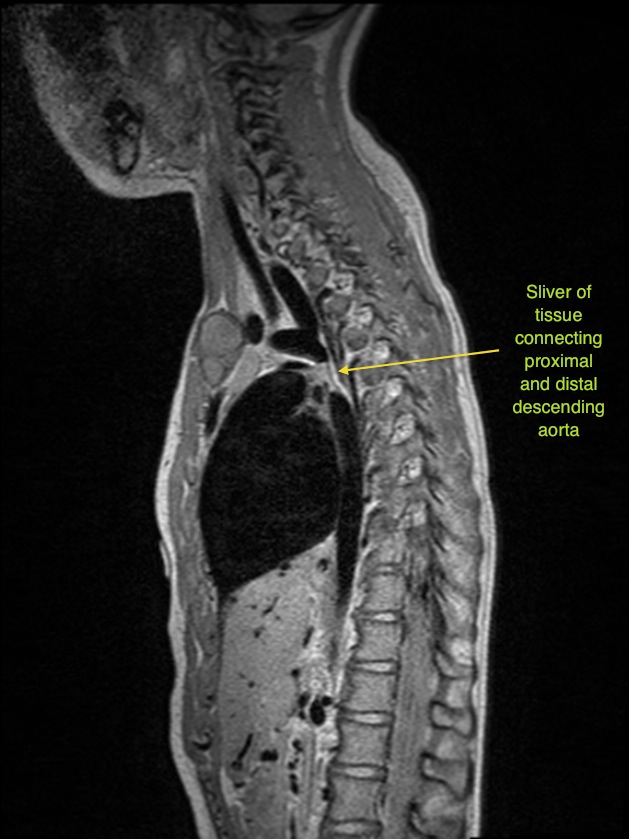
Parasagittal TSE imaging: shows severe long segment narrowing of the aortic isthmus rather than interruption of the aortic arch.
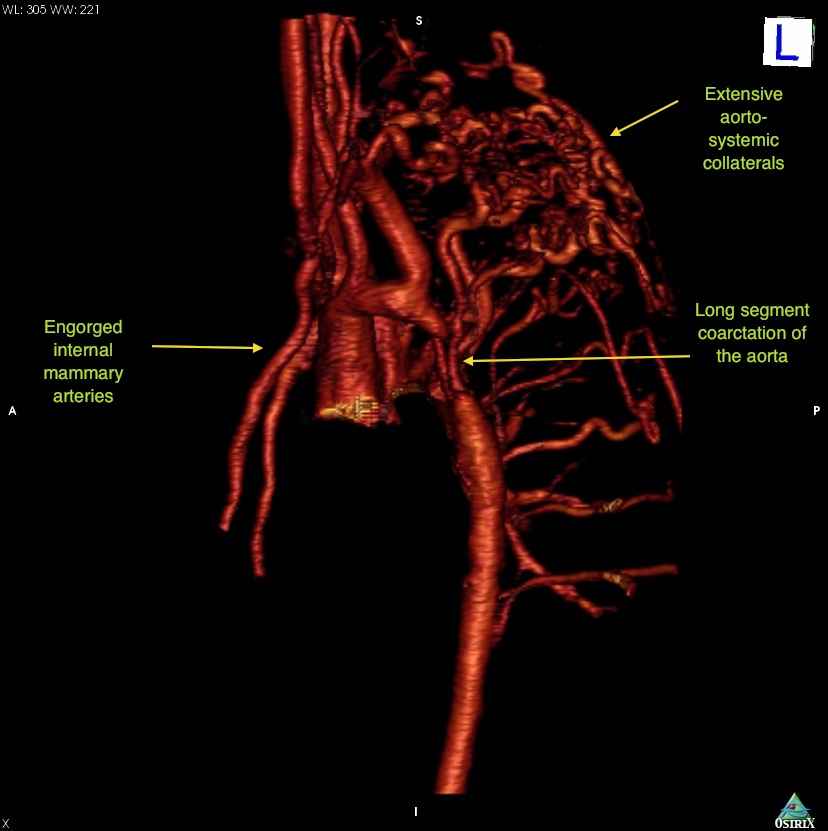
Gadolinium enhanced 3D angiography: shows multiple dilated intercostals, internal mammary and subclavian arteries consistent with significant aortico-systemic collateralization.

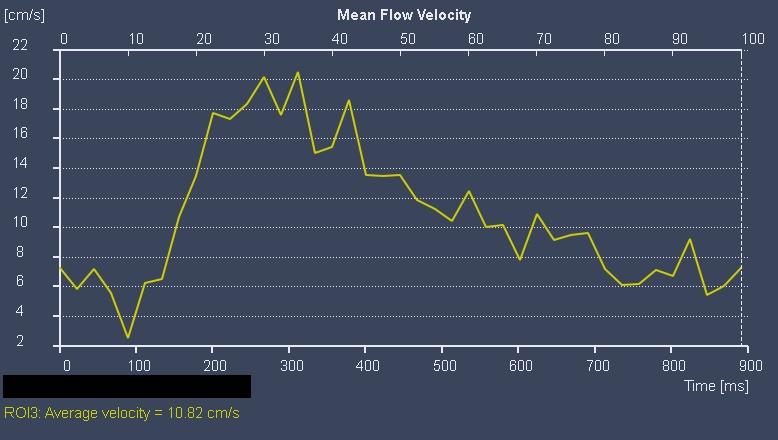
Velocity data obtained by through-plane imaging of the abdominal aorta demonstrates persistent antegrade diastolic flow with no return to the baseline
Conclusion:
CMR confirmed the presence of a long segment severe coarctation of the aorta with multiple aorto-systemic collaterals. Velocity-encoded phase contrast over the proximal and distal descending aorta indicated almost exclusive collateral supply of the descending aorta. Associated findings of a bicommissural aortic valve without significant stenosis or regurgitation was also demonstrated.
The patient was referred for surgical repair with an end-to-end anastomosis through a lateral and posterior left thoracotomy. There were no perioperative complications. Although there have been a few very small case series of stenting severe long segment coarctation (1,2), one which showed no complications found at a mean of 33 months of follow-up (1), there has been no clear benefit to percutaneous approach compared to surgical approach, unless in the setting of a vasculitic process.
The presence of a gradient across the bicuspid valve may be masked in the setting of a severe coarctation which increases the peak velocity proximal to the coarctation. This therefore, may decrease the true gradient across the left ventricle and the aortic arch. This was closely evaluated during the post-operative echo, which showed, in fact, no evidence of stenosis across the bicuspid aortic valve.
Perspective:
CMR is a powerful tool to clearly define the anatomy of a complex coarctation of the aorta. Aortic profiles by phase contrast imaging at the proximal and distal descending aorta has been shown to offer additional tools in assessing hemodynamic significance of a coarctation (3). Furthermore, the presence of associated cardiovascular anomalies can be diagnosed with this technique. In a study of 500 patients referred for CMRI for coarctation of the aorta, the most common associated cardiac anomalies are bicuspid aortic valve (60%), arch hypoplasia (14%), and ventricular septal defect (13%) (4). In addition to anatomic clarification, cardiac MRI can detect the presence of myocardial infarction associated with left sided obstruction (5).
We demonstrate here the use of 2mm slices through the parasagittal plane with SSFP single shot imaging. The area of coarctation is easily identified even before angiography is performed. Black blood imaging through this plane has been shown to be a sensitive technique in evaluating for restenosis following surgical intervention (6)Here we show that single shot SSFP is another sequence which can be utilized for accurately defining the aortic defect in a native coarctation without he use of intravenous contrast.
Managing of the patient with coarctation of the aorta requires lifelong follow-up and CMRI is increasingly becoming a critical component of care in adults with congenital heart disease (7). This is because CMR, besides determining initial anatomy, function, flow profile, and tissue characterization without exposure to ionizing radiation, offers a baseline by which further imaging can be compared.
References:
1. Thanopoulos BD, Hadjinikolaou L, Konstadopoulou GN, Tsaousis GS, Triposkiadis F, Spirou P. Stent treatment for coarctation of the aorta: intermediate term follow up and technical considerations. Heart. Jul 2000;84(1):65-70.
2. Thanopoulos BV, Triposkiadis F, Margetakis A, Mullins CE. Long segment coarctation of the thoracic aorta: treatment with multiple balloon-expandable stent implantation. American Heart Journal. Apr 1997;133(4):470-473.
3. Muzzarelli S, Ordovas KG, Hope MD, Meadows JJ, Higgins CB. Diagnostic value of the flow profile in the distal descending aorta by phase contrast magnetic resonance for predicting severe coarctation of the aorta. Journal of Magnetic Reseonance Imaging 2011;33:1440-1446.
4. Teo LL, Canell T, Babu-Narayan SV, Hughes M, Mohiaddin RH. Prevalance of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol 2011; Epub ahead of print.
5. Toro-Salazar OH, Steinberger J, Thomas W, Rocchini AP, Carpenter B, Moller JH. Long term follow-up of patients after coarctation of the the aorta repair. Am J Cardiol 2002;89:541-547.
6. Greenberg SB, Marks LA, Eshaghpour EE. Evaluation of magnetic resonance imaging in coarctation of the aorta: The importance of multiple imaging planes. Pediatric Cardiolgy 1997:18(5).
7. Broberg C, Meadows A. Advances in imaging: the impact of care of the adult with congenital heart disease. Prog Cardiovascular Dis 2011;53(4):293-304.
Submit your case here
COTW handling editor: M. Jay Campbell, MD
Have your say: What do you think? Latest posts on this topic from the forum







