Case from: Javed M. Nasir1, Andrew Crean2, Kevin Steel1
Institute: 1San Antonio Military Medical Center, San Antonio, Texas, U.S.A; 2Peter Munk Cardiac Center, Toronto General Hospital, Toronto, Canada
Clinical history:
A 28 year old woman with history of Wolf-Parkinson-White syndrome status-post ablation of a right posterolateral bypass tract four years earlier who was referred to us for evaluation of an abnormal transthoracic echocardiogram. She had a prior echocardiogram report with her from four years earlier that showed only mild tricuspid regurgitation with a structurally normal heart. She was asymptomatic without chest pain, orthopnea, dyspnea on exertion, lower extremity swelling, syncope, or palpitations and had recently ran a half-marathon without difficulty. Her heart rate and blood pressure were normal, and the physical exam was notable for an extra early systolic sound and II/VI systolic decrescendo murmur heard best at the right upper sternal border that increased with inspiration.
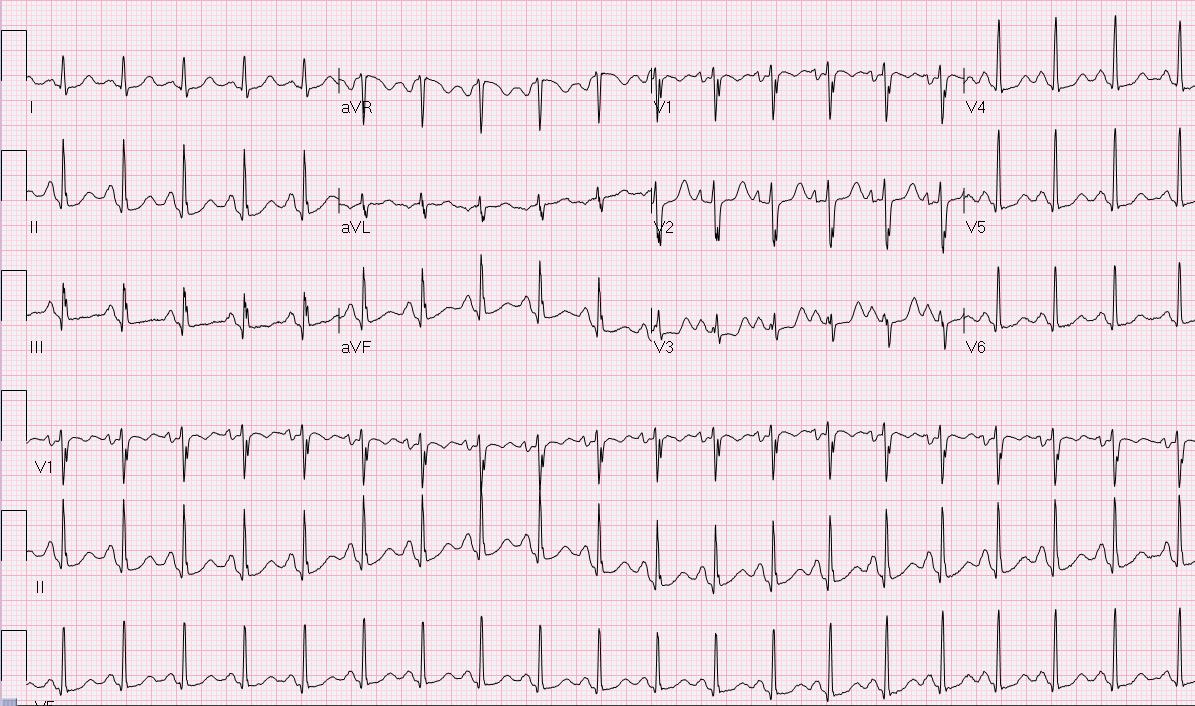
Electrocardiography showed sinus tachycardia and biatrial enlargement.
Chest roentgenography was normal.
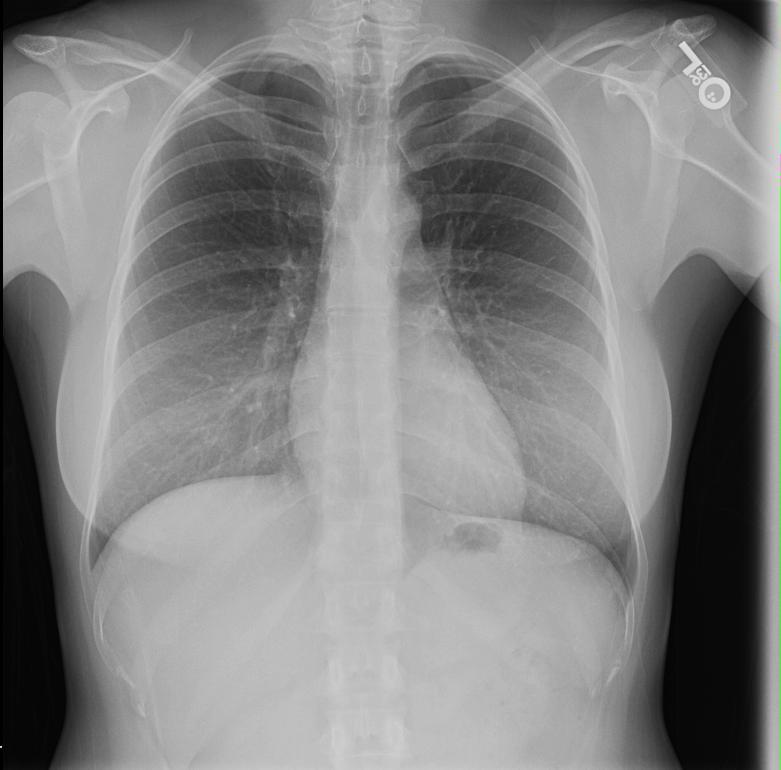
CXR
She then underwent transthoracic echocardiography which showed mild TR, Ebstein anomaly, and a weakly positive bubble study. There was no evidence of right ventricular outflow obstruction, and subsequent transesophageal echocardiogram showed no atrial or ventricular septal defects.
TTE 4 chamber
TTE 4 chamber with color
CMR Findings:
CMR confirmed the diagnosis of Ebstein anomaly. While her septal tricuspid annulus was only displaced 19 mm, when normalized for her body surface area, 1.6 m2, it was displaced 12 mm/m2. The MRI was not sequenced for evaluation of flow. The left ventricular end systolic volume, end diastolic volume, and ejection fraction were 21ml, 83ml and 74%, respectively. The right ventricular end systolic volume, end diastolic volume, and ejection fraction were 61ml, 115ml and 47%, respectively.

4chamber CMR with TR

2chamber CMR
After diagnosing Ebstein anomaly in this active duty airwoman, she was returned to her prior duties with no limitations on her career or physical training, other than following up annually with a cardiologist.
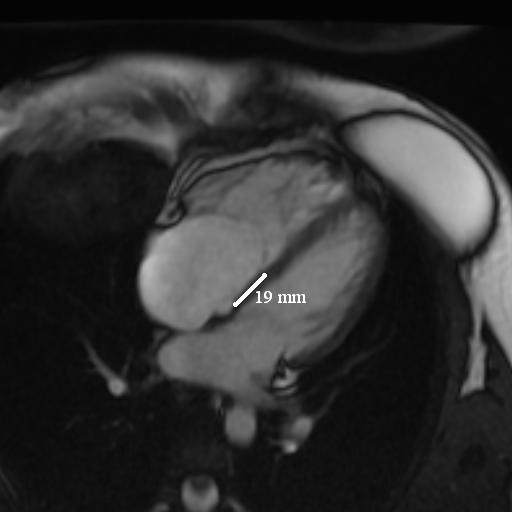
4 chamber CMR static with measurement
Ebstein anomaly is a rare congenital disorder that occurs in approximately 1 out of every 200,000 live births and accounts for <1% of congenital heart disease.1 This disease is characterized by an apical displacement of the tricuspid leaflets (septal>posterior>anterior). This anomaly causes an atrialization of the right ventricle and can lead to cyanosis, tricuspid regurgitation, and right ventricular outflow tract (RVOT) obstruction or functional tricuspid stenosis. Ebstein is associated with many other cardiac defects and more than half of patients with Ebstein anomaly have atrial shunts, 25% have an accessory conduction pathway, and there is also an increased risk of ventricular septal defects and varying degrees of RVOT obstruction.2
Conclusion: Diagnosis of mild Ebstein anomaly can be difficult as both the septal and posterior leaflets are apically displaced in normal hearts. While there is considerable overlap in septal leaflet displacement between normal patients and patients with Ebstein anomaly, in the apical 4 chamber view utilizing transthoracic echocardiography, displacement of the septal leaflet of more than 20 mm from the mitral annulus has been advocated as diagnostic criterion in adults.3 When this septal leaflet displacement is normalized for the body surface area (BSA), a displacement of more than 8mm/m2 by 2D echocardiography has been shown to completely discriminate patients with Ebstein anomaly.4 Only recently has a CMR study been published which validates the measurement of septal displacement by CMR imaging when compared to echocardiography and determines references ranges of right ventricular volumetric data for Ebstein anomaly.5
While the overall prognosis for Ebstein anomaly is poor, most of the natural history trials were published prior to use of echocardiography and mainly included severe disease that was diagnosed as an infant. More recent data demonstrates that when Ebstein anomaly is initially diagnosed in adulthood, there are less associated cardiac defects, cyanosis is rare, and it is associated with a much lower mortality and morbidity.6
Perspective: Ebstein anomaly remains a rare type of congenital heart disease with many associated cardiac defects. As this case illustrates, Ebstein anomaly can be subtle on the MRI and it is important to routinely measure the tricuspid septal leaflet apical displacement and normalize for BSA to ensure mild cases of Ebstein anomaly are not missed.
Do you want to comment on the breast implants of the patient and the possible effects on ECG findings (decrease in voltage)? When were the breast implants implanted? Before or after the ablation in 2006?
Note: The breast implants were implanted four years prior to the ablation and may have masked some of the voltage from her pathway. However, no pre ablation ECG is available.
References:
1. Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein’s Anomaly. Circulation. 2007;115:277-285.
2. Warnes CA, Williams RG, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). J Am Coll Cardiol. 2008 Dec 2;52(23):e1-121.
3. Gussenhoven EJ, Stewart PA, Becker AE, Essed CE, Ligtvoet KM, De Villeneuve VH “Offsetting” of the septal tricuspid leaflet in normal hearts and in hearts with Ebstein’s anomaly. Anatomic and echographic correlation. Am J Cardiol. 1984;54(1):172-6.
4. Shiina A, Seward JB, Edwards WD, Hagler DJ, Tajik AJ. Two-dimensional echocardiographic spectrum of Ebstein’s anomaly: detailed anatomic assessment. J Am Coll Cardiol. 1984;3(2 Pt 1):356.
5. Yalonetsky S, Tobler D, Greutmann M, Crean AM, Wintersperger BJ, Nguyen ET, Oechslin EN, Silversides CK, Wald RM. Cardiac magnetic resonance imaging and the assessment of ebstein anomaly in adults. Am J Cardiol. 2011 Mar 1;107(5):767-73. Epub 2011 Jan 19.
6. Celermajer DS, Bull C, Till JA, Cullen S, Vassillikos VP, Sullivan ID, Allan L, Nihoyannopoulos P, Somerville J, Deanfield JE. Ebstein’s anomaly: presentation and outcome from fetus to adult. J Am Coll Cardiol. 1994;23(1):170.
COTW handling editor: Sohrab Fratz, MD





