Case from: Lorenzo Monti, Tiziana Manias, Barbara Nardi, Luca Balzarini.
Institute: Radiology and Cardiology Department, I.R.C.C.S. Istituto Clinico Humanitas, Rozzano (MI) ITALY
Clinical history: An asymptomatic 38 year-old man was referred to our center for further assessement because of his family history. The patient’s father was previously diagnosed with right ventricular arrhythmogenic cardiomyopathy, a diagnosis that was confirmed on endomyocardial biopsy and subsequently on the explanted heart following heart transplant for ventricular arrhythmias and dilated cardiomyopathy.
Our young patient’s current echocardiogram was reported as nor mal.
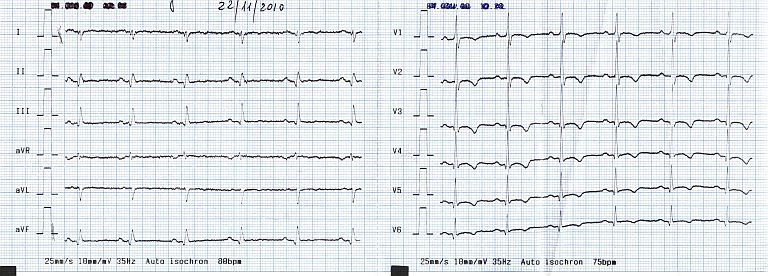
ECG 1
His resting 12-lead ECG however was abnormal, showing non-significant Q waves in the inferior leads, diffuse T wave inversion in the precordial leads, and T-wave flattening in the peripheral leads (see ECG 1).
Given the family history, a new CMR study was prescribed for him. Of note, he had already undergone a previous CMR study in 2001 (images not available). There was no evidence at that time of fatty infiltration of the myocardium; gadolinium had not been administered on that occasion. His ECG in 2001 was however already abnormal, showing similar diffuse T wave abnormalities already.

Movie 1 & Movie 2
Movie 3 & Movie 4
CMR Findings:.
Both the right and left ventricles are dilated, with moderately reduced bi-ventricular ejection fraction and extensive regional wall motion abnormalities (Movies 1 -4, four-chamber, 2-chamber, 3-chamber and RVOT views) and measurements as follows:
Left ventricle: LVEDV 190 ml (=102 ml/m2); LV mass 149 g (80g/m2); LVEF = 48%.
Right ventricle: RVEDV 219 ml (=117 ml/m2); RVEF = 41%.
Of note, there is localised akinesia of the RV apex (Movie 4).
Movie, 5, Movie 6, and Movie 7
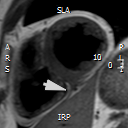
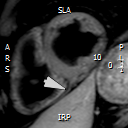
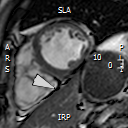
There is suspicion of extensive fibro-fatty replacement of the inferior left and right ventricular wall as shown in Figure 1. The site of fatty infiltration (white arrows) can be appreciated on T1 weighted sequences (Figure 1a) when compared to the T1-weighted images with fat-saturation in the same image position (Figure 1b). This infiltration is further unveiled by presence of an unusual chemical shift artefact in the steady-state free precession cine (SSFP) sequences (Figure 1c, still frame, white arrow).
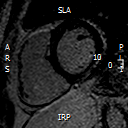
Figure 2
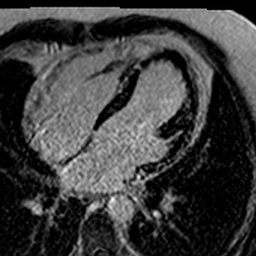
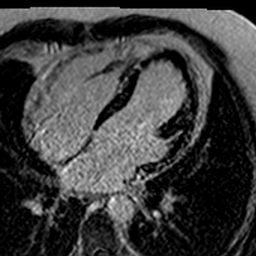
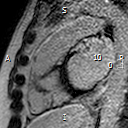
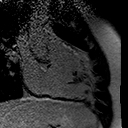
Figure 3 (a, b, c, d)
Late Gadolinium enhancement images (PSIR sequences) confirm the presence of fibrous replacement which is visible in the left inferior and infero-lateral wall (Figure 2, short-axis view). This is also seen on the long axis views (Figure 3 top panel left = 3-chamber view, and top panel right = 4-chamber view). There is also fibrosis of the right ventricular outflow tract (Figures 3 bottom panel).
Conclusion:
In this patient, echocardiography failed to identify the initial bi-ventricular dilatation and dysfunction. The number of structural heart abnormalities observed by CMR in this patient allowed a new diagnosis of arrhythmogenic cardiomyopathy with left ventricular involvement to be made. In our case, the newly-modified 2010 diagnostic criteria for ARVC 1 are met in this patient with 3 major criteria being fulfilled: (1) pathologically confirmed diagnosis of ARVC in a first degree relative; (2) RV dilatation with regional akinesia and (3) T wave inversion in V1 – V3. In addition, our CMR data supports not only right but also left ventricular disease involvement, although the left ventricular involvement could already be suspected from the ECG considering the T wave abnormalities extending to the lateral leads3-5.
Perspective:
Cardiomyopathies, including ARVC, may progress over the years. Therefore, a normal imaging study should be repeated after a couple of years to detect potential disease progression, along side other diagnostic tools, such as ECG and Holter monitoring.
Ventricular dilatation and dysfunction are the consequence of advanced ventricular damage; CMR has the unique opportunity to combine various pulse sequences (SSFP, T1,T1 fat-sat and LGE images ) for the detection of not only the advanced stages of the disease, but also for the detection of early structural heart changes, which can be of great help for early diagnosis – although ECG and Holter monitoring are also very helpful and sensitive tools in this setting.
Of note, the presence of fat in scars is non-specific6.
To base a diagnosis only on dilatation and dysfunction may delay the diagnosis of cardiomyopathy, especially in relatives of an index patient, and may be misleading in patients with other still unknown causes of right heart failure (for example, anomalous pulmonary venous return).
Equally, family screening remains a cornerstone of clinical management, since advanced stages of the disease can be asymptomatic, as in this case.
References:
1.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Pro tonotarios N, Saffitz JE, Sanborn DM, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, Zareba W. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010 Apr 6;121(13):1533-41.
2. McKenna WJ, Thiene G, Nava A, Fontaliron F, Blomstrom-Lundquist G, Fontaine G, Camerini F, on behalf of the Task Force of the working group myocardial and pericardial disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Diagnosis of arrhythmogenic right ventricular dysplasia cardiomyopathy.







