Case from: Daniel M Sado,1 Gianni Quarta,1 Viviana Maestrini,1 Alison Muir,1 Michael Ashworth,2 Antonis Pantazis,1 Perry Elliott,1 James Moon1
Institute: 1Department of Inherited Cardiac Disease, The Heart Hospital, 16-18 Westmoreland Street, London, England, W1G 8PH. 2Department of Histopathology, Great Ormond Street Hospital for Children, London, England, WC1N 3JH.
Clinical history: A 52 year old gentleman presented with a 3-month history of tiredness, severe reduction in exercise tolerance (NYHA 3), orthopnoea, weight loss and progressive ascites.
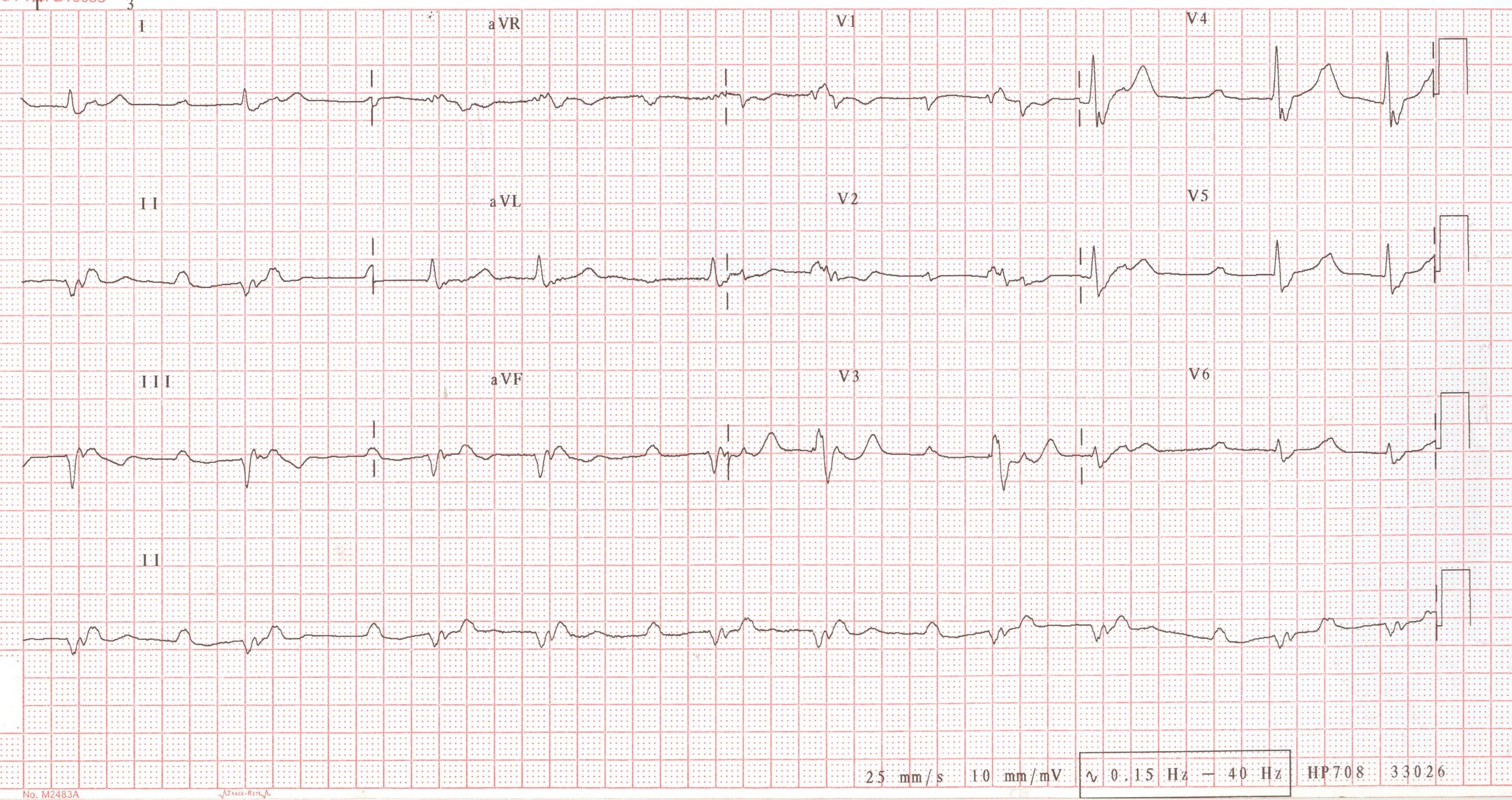
Figure 1
Transthoracic echocardiography (Movie 1) was performed showing mildly dilated left ventricular (LV) dimensions, but severe systolic impairment (EF: 12% using Simpsons Rule). The right ventricle (RV) had moderate dilatation and severe systolic impairment.
A coronary angiogram showed no flow limiting coronary disease.
Cardiovascular magnetic resonance (CMR) was performed to investigate these findings in more detail.
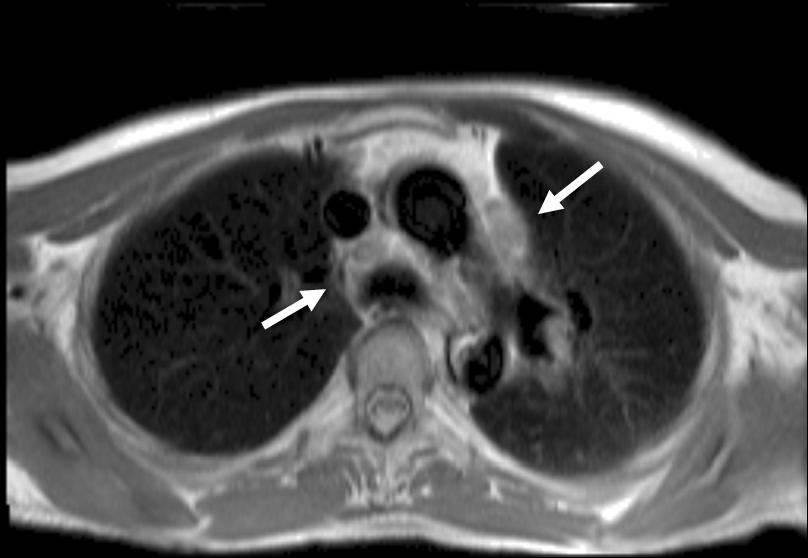
Figure 2
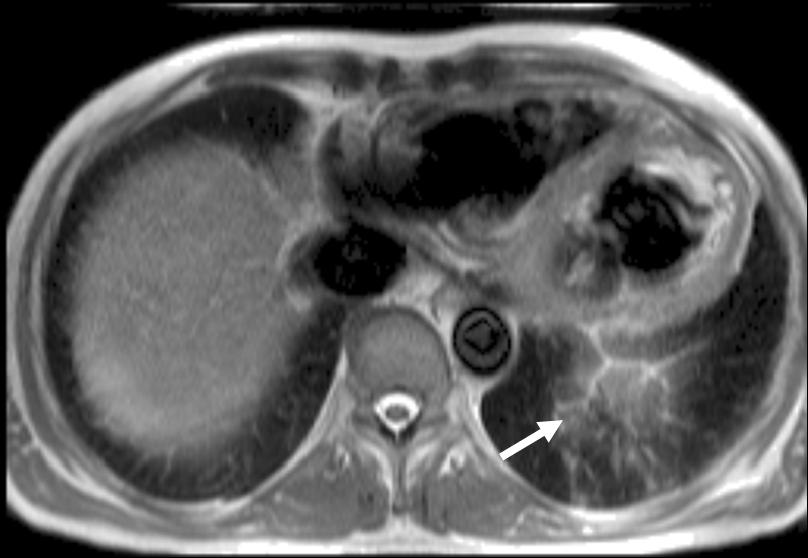
Figure 3
The Black blood transverse stack images depict thoracic lymphadenopathy (Figure 2) and left basal lung parenchymal changes (Figure 3).

Movie 2
Cine images show severe bi-ventricular dilatation and systolic dysfunction (Movie 2). The majority of the LV segments were akinetic. Of note, the wall thickness of the dysfunctional segments was not reduced.
On T2 weighted imaging, there was no evidence of oedema (not shown)
Movie 3
Late-gadolinium enhancement (LGE) images (Movie 3), revealed extensive fibrosis (some of which was transmural) involving the left and right ventricle.
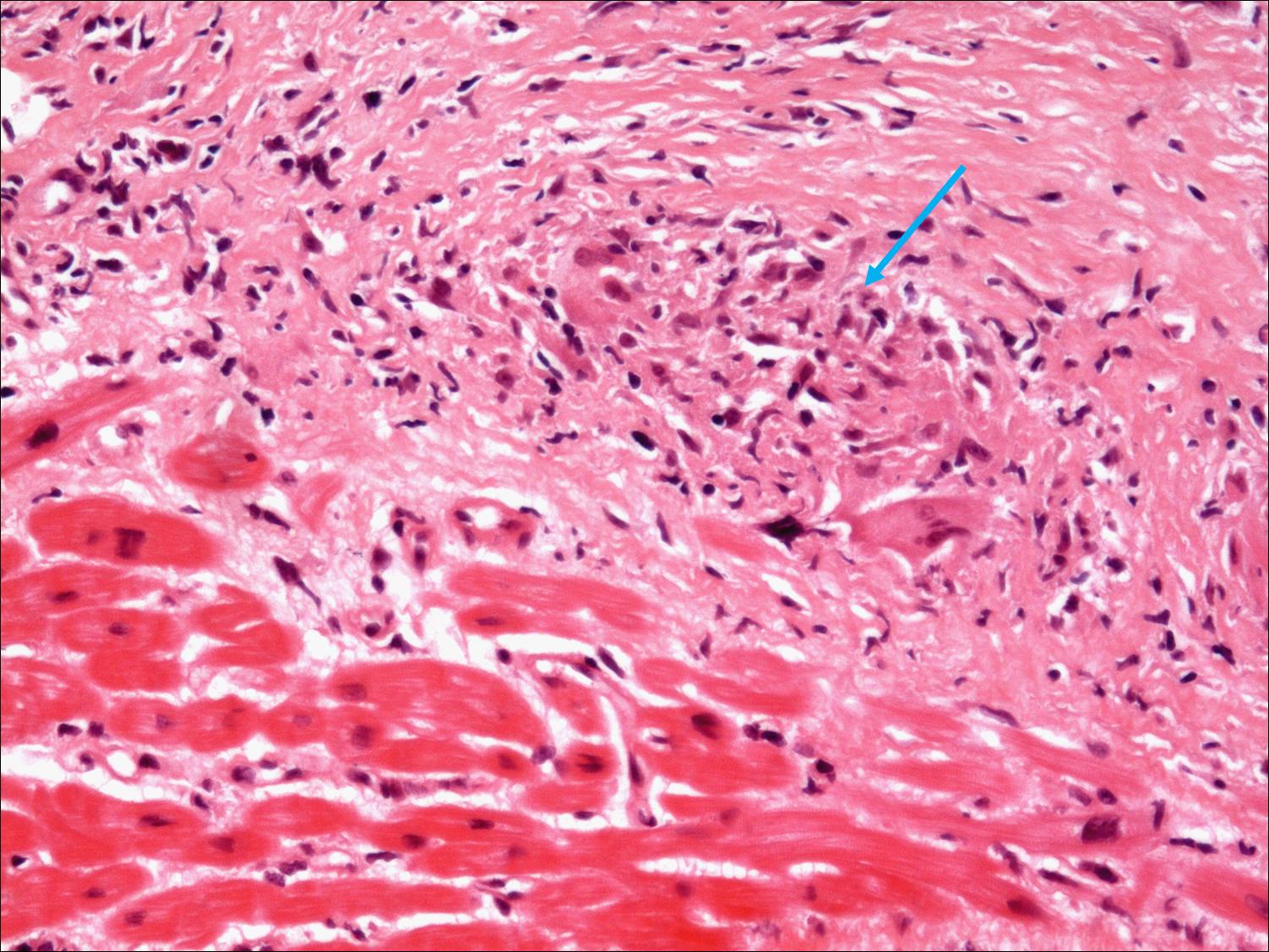
Figure 4
The patient was treated with optimisation of his heart failure medication and insertion of a biventricular pacemaker with implantable cardioverter defibrillator. Steroid treatment and Methotrexate were also initiated.
Perspective: CMR is a very useful investigation for patients with impaired left ventricular systolic function, often suggesting the underlying cause. There are a variety of conditions associated with dilated cardiomyopathy and conduction disease: inflammatory/infective (sarcoidosis, giant cell myocarditis, Chagas disease), genetic (laminopathies, end-stage HCM, ARVC, LVNC) and infiltrative/metabolic (Danon disease, AMP-kinase disease, end-stage forms of Anderson-Fabry disease, cardiac amyloidosis, cardiac iron overload).1 CMR is very useful in the differential diagnosis and may guide clinical management, identifying patients that may benefit from invasive procedures like endomyocardial biopsy. In the case described, both cardiac and extracardiac features of sarcoidosis could be identified by CMR, which along with the abnormal ECG findings was highly suggestive of the diagnosis.2-5 This was then confirmed by endomyocardial biopsy, allowing specific therapy to be administered.
References:
- Lakdawala NK, Givertz MM. Dilated cardiomyopathy with conduction disease and arrhythmia. Circulation. 2010;122:527-34.
- Doughan AR, Williams BR. Cardiac sarcoidosis. Heart. 2006 Feb;92:282-8.
- Smedema JP, Snoep G, van Kroonenburgh MP, van Geuns RJ, Dassen WR, Gorgels AP, Crijns HJ. Evaluation of the accuracy of gadolinium-enhanced cardiovascular magnetic resonance in the diagnosis of cardiac sarcoidosis. J Am Coll Cardiol.2005;45:1683-90.
- Mehta D, Lubitz SA, Frankel Z, Wisnivesky JP, Einstein AJ, Goldman M, Machac J, Teirstein A. Cardiac involvement in patients with sarcoidosis: diagnostic and prognostic value of outpatient testing. Chest. 2008;133:1426-35.
- Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357:2153-65.
COTW handling editor: Giovanni Quarta





