Authors: Manuel De Lazzari, MD1, Francesco Corbetti, MD2, Martina Perazzolo Marra, MD1, Luisa Cacciavillani, MD, PhD1, Massimo Napodano, MD1, Sabino Iliceto, MD1
1Division of Cardiology, Department of Cardiac, Thoracic and Vascular Sciences, University of Padua, Italy
2Radiology, University of Padua, Italy
Clinical History: A 77-year-old male with a history of dyslipidemia and hypertension was admitted to our Emergency Department for unstable angina. While obtaining a complete history, the patient reported that 20 years ago he was in a motor vehicle accident where he suffered a severe precordial thump but suffered no known permanent effects.
The electrocardiogram demonstrated a right bundle branch block and inferior Q waves (Figure 1A); during chest pain, ST-segment depression was noted in the right precordial leads V1-V3 (Figure 1B). An echocardiogram revealed normal left ventricular dimensions and systolic function with hypokinesia of the inferior wall. The patient was referred for coronary angiography which showed occlusion of the mid left anterior descending artery (LAD) with collateral circulation and functional occlusion of the proxmial right coronary artery (RCA) with collateral circulation.
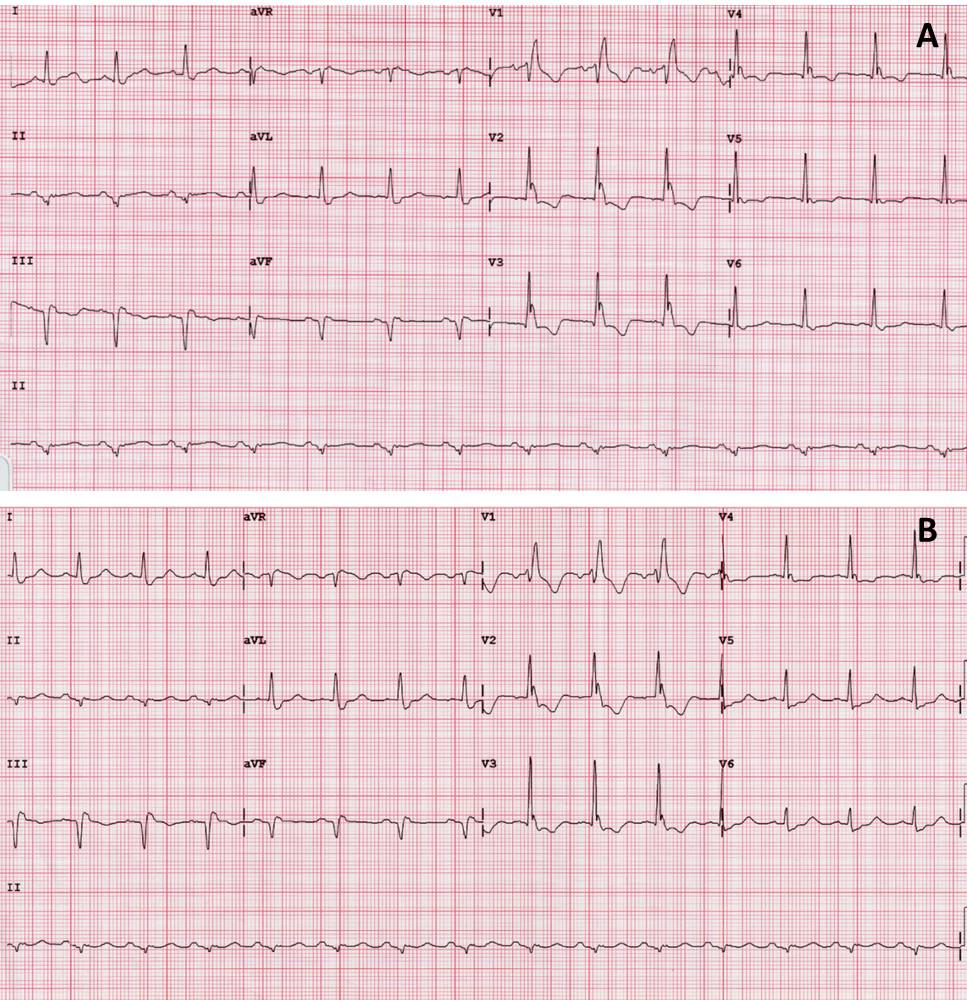
Figure 1
Cardiac MRI: A Cardiac Magnetic Resonance (CMR) was performed to evaluate the extent of suspected previous silent necrosis and myocardial areas at risk. CMR showed non transmural necrosis of the inferior wall on basal and mid segments without signs of myocardial edema. Moreover, the presence of a round structure connected to the sinotubular aorta by a large neck (Figure 2) was noted on the 3-chamber cine images (Movie 1); on short axis compromise of the right coronary artery with thrombosis was also demonstrated (Movie 2). T1-weighted inversion recovery sequences after contrast injection revealed a mural thrombus within the abnormal structure with typical susceptibility effects inside (Figure 3, white asterisk). Interestingly, gadolinium enhancement of the tunica adventitia was present representing the unique aortic layer defining the structure as a pseudoaneurysm (Figure 3, white arrow).

Figure 2
Movie 1

Movie 2
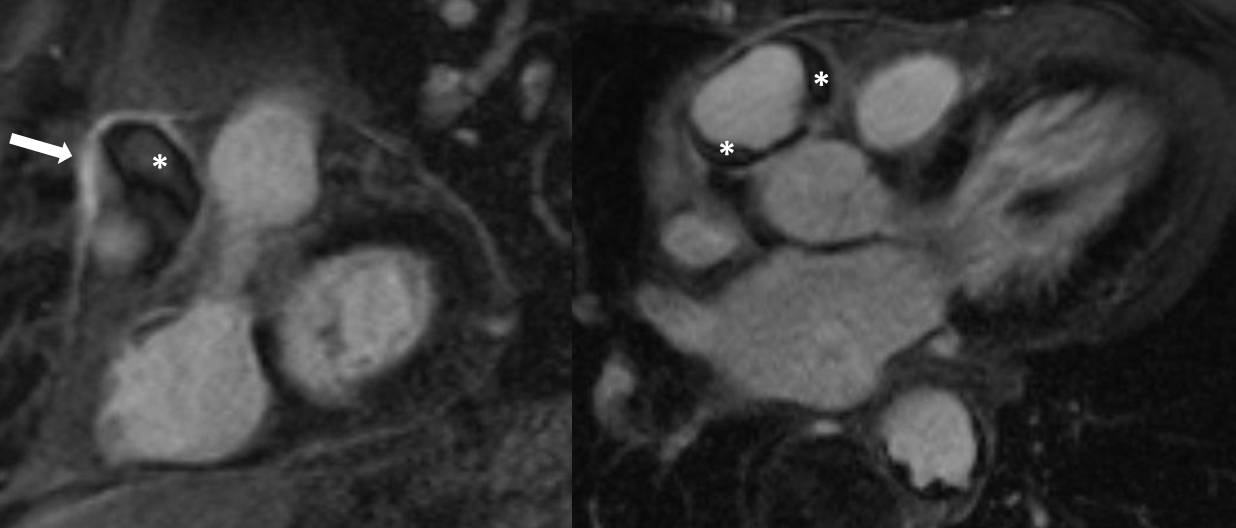
Figure 3
A CT was subsequently performed to evaluate the pseudoaneurysm and its relationship with the coronary arteries (Figure 4). On the basis of the proximal relationship of the RCA ostium and pseudoaneurysm’s neck, an open surgical repair seemed not feasible without impairing aortic valve and coronary ostia integrity. After discussion with the cardiothoacic suregons, we decided to treat the patient with two separate procedures: 1) grafting left internal mammary artery to LAD and circumflex coronary arteries, then 2) repairing the weak point of the aorta by stent graft through the left ventricular apex via left anterior minithoracotomy.
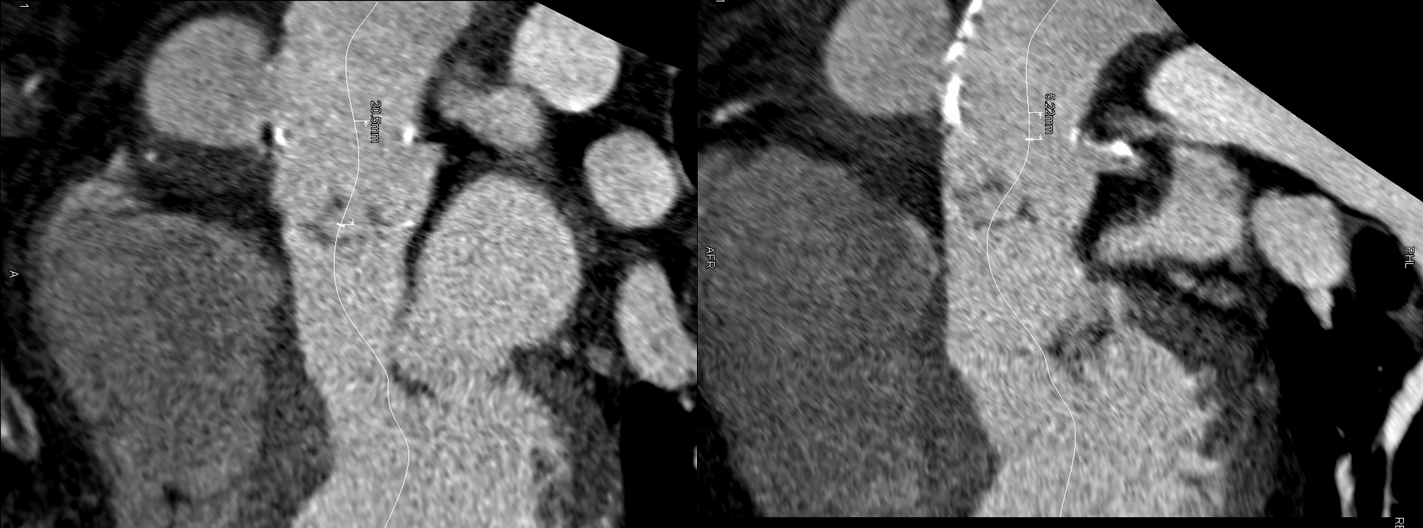
Figure 4
Conclusion: The aim of this case report is to summarize the application of CMR to a patient with a suspected previous myocardial infarction, referred for acute chest pain in which the CMR allowed a complete diagnosis that excluded an acute coronary syndrome, but showing with the same examination the evaluation of aorta layers, beyond traditional endoluminal imaging modalities such as angiography.
References:
- Hiratzka LF, Bakris GL, Beckman JA, et al; 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. 2010;55(14):e27-e129.
- Pennell DJ; Cardiovascular Magnetic Resonance. Circulation 2010;121:692-705.
- Raman SV, Simonetti OP, Winner MW 3rd, et al; Cardiac magnetic resonance with edema imaging identifies myocardium at risk and predicts worse outcome in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol. 2010;55(22):2480-8.
Case of the Week Handling Editor: Kevin Steel







