Case from: Sohrab Fratz, Andreas Eicken, Heiko Stern, John Hess
Institute: Department of Pediatric Cardiology and Congenital Heart Disease, German Heart Center at the Technical University Munich, Germany
Clinical history: A 5-year old girl with tricuspid valve dysplasia was referred to our center for management of her tricuspid valve regurgitation. At the age of three, the tricuspid regurgitation was treated by a modified Alfieri stich1 and de Vega anuloplasty2. Five months later, the reconstructed valve was replaced by a Perimount™ valve with an inner diameter of 20 mm. This valve is a porcine pericardial bioprosthesis mounted on a cobalt-chromium alloy stent frame. Initial postoperative echocardiography showed no tricuspid regurgitation. However, since then tricuspid regurgitation had increased by echocardiographic assessment.
CMR findings before treatment: Hemodynamic assessment by CMR depicted tricuspid regurgitation of 20%, a reduced cardiac index of 2.5 l/min/m², a large RVEDV, and a small LVEDV (Movie 1, Figure 1A and B, Tables 1 and 2). The patient was reffered to the cath lab for percutaneous tricuspid valve implantation.
Movie 1: stack of axial slices for RV and LV volume analysis acquired during free breathing before treatment
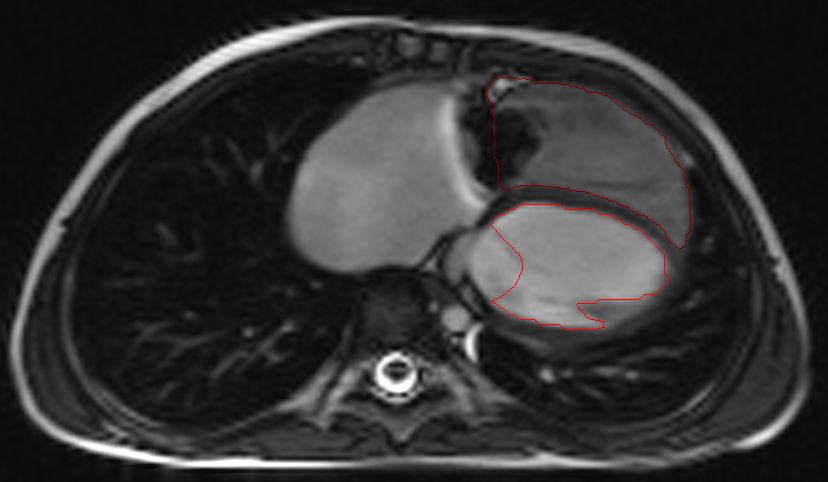
Figure 1A and B: End-diastolic RV and LV endocardial tracing before treatment
| EF [%] | EDV [ml] | ESV [ml] | SV [ml] | EDVI [ml/m²] | ESVI [ml/m²] | |
| RV | 35 | 86 | 56 | 30 | 117 | 77 |
LV | 58 | 39 | 17 | 23 | 54 | 23 |
Table 2: Results of flow measurements at CMR before treatment
| Flow | |||
| net [ml] | forward[ml] | backward [ml] | |
| MPA | 24 | 24 | 0 |
| Aorta | 25 | 25 | 0 |
| RPA | 14 | 14 | 0 |
LPA | 8 | 9 | 1 |
Movie 3 – Right ventriculography before Melody™ transcatheter valve implantation

Movie 4 – Right ventriculography after Melody™transcatheter valve implantation
CMR findings after treatment: The day after the intervention CMR showed significant relevant hemodynamic improvements. Tricuspid valve regurgitation decreased to 0%, cardiac index increased to 3.3 l/min/m², RVEDV decreased, and LVEDV increased (movie 5, figure 2, table 3 and 4).
Movie 5: stack of axial slices for RV and LV volume analysis acquired during free breathing after treatment

Figure 2: Enddiastolic RV and LV endocardial tracing after treatment
| EF [%] | EDV [ml] | ESV [ml] | SV [ml] | EDVI [ml/m²] | ESVI [ml/m²] | |
| RV | 33 | 79 | 53 | 26 | 108 | 72 |
LV | 57 | 48 | 21 | 27 | 65 | 28 |
Table 4: Results of flow measurements at CMR after treatment
| flow | |||
| net [ml] | forward[ml] | backward [ml] | |
| MPA | 27 | 27 | 0 |
| Aorta | 26 | 26 | 0 |
| RPA | 17 | 17 | 0 |
LPA | 11 | 11 | 0 |
Conclusion: Tricuspid valve dysplasia is unlike Ebstein´s disease a rare disease3-5. It is commonly responsible for severe tricuspid regurgitation and presents as a surgical challenge6-10. This is also illustrated by this case. Percutaneous valve implantation was only possible in this case because previously the patient had been treated by a bioprosthesis mounted on stent frame. The stent provided the secure landing zone for the percutaneous valve.
Perspective: CMR guided the treatment and demonstrated significant beneficial hemodynamic changes in this 5-year-old patient without the need of sedation, contrast agent or radiation. No other method can quantify tricuspid regurgitation and RVEDVI. Furthermore, CMR can quantify cardiac index non-invasively. Therefore CMR can and will be used for life long follow-up in this patient. Two specific points need to be mentioned regarding RV and LV volume analysis of children with congenital heart disease. First, at our center, we feel that axial slice orientation is superior to LV short axis orientation when serial follow-up EDV analysis is required clinically11. Secondly, this case demonstrats that the stack of cine slices required for volume analysis can be generated during free-breathing, as shown by others12. This case also highlights the possibilities of quantifing tricuspid regurgitation by combining careful quantification of pulmonary blood flow and accurate measurements of RV volumes using the equation TR = x10013.
References:
- Maisano F, Schreuder JJ, Oppizzi M, Fiorani B, Fino C, Alfieri O. The double-orifice technique as a standardized approach to treat mitral regurgitation due to severe myxomatous disease: surgical technique. Eur J Cardiothorac Surg. 2000;17(3):201-5.
- Kanter KR, Doelling NR, Fyfe DA, Sharma S, Tam VK. De Vega tricuspid annuloplasty for tricuspid regurgitation in children. Ann Thorac Surg. 2001 Oct;72(4):1344-8.
- Sharland GK, Chita SK, Allan LD. Tricuspid valve dysplasia or displacement in intrauterine life. J Am Coll Cardiol. 1991;17:944-949.
- Nathan AT, Marino BS, Dominguez T, Tabbutt S, Nicolson S, Donaghue DD, Spray TL, Rychik J. Tricuspid valve dysplasia with severe tricuspid regurgitation: fetal pulmonary artery size predicts lung viability in the presence of small lung volumes.Fetal Diagn Ther. 2010;27(2):101-5.
- Yam MC, Ng PC, Fok TF. Isolated congenital tricuspid valve dysplasia: a rare condition mimicking persistent pulmonary hypertension of the newborn. J Paediatr Child Health. 1996;32(6):536-8.
- Butera G, Pomè G, Giamberti A, Frigiola A, Chessa M, Carminati M. Surgical treatment of tricuspid valve dysplasia in the neonatal period. Ital Heart J. 2003;4(3):211-3.
- Katogi T, Aeba R, Ito T, et al. Surgical management of isolated congenital tricuspid regurgitation. Ann Thorac Surg 1998; 66: 1571-4.
- Kumar N, Gallo R, Al-Halees Z, Al-Fadley F, Duran CM. Unstented semilunar homograft replacement of tricuspid valve in Ebstein’s malformation. Ann Thorac Surg 1995;59: 320-2.
- Pasque M, Williams WG, Coles JG, Trusler CA, Freedom RM. Tricuspid valve replacement in children. Ann Thorac Surg 1987; 44: 164-8.
- Reddy VM, McElhinney DB, Brook MM, Silverman NH, Stanger P, Hanley FL. Repair of congenital tricuspid valve abnormalities with artificial chordae tendineae. Ann Thorac Surg 1998; 66: 172-6.
- Fratz S, Schuhbaeck A, Buchner C, Busch R, Meierhofer C, Martinoff S, Hess J, Stern H. Comparison of accuracy of axial slices versus short-axis slices for measuring ventricular volumes by cardiac magnetic resonance in patients with corrected tetralogy of fallot. Am J Cardiol. 2009 Jun 15;103(12):1764-9.
- Buechel EV, Kaiser T, Jackson C, Schmitz A, Kellenberger CJ. Normal right- and left ventricular volumes and myocardial mass in children measured by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2009 Jun 21;11:19.
- Cawley PJ, Maki JH, Otto CM. Cardiovascular magnetic resonance imaging for valvular heart disease: technique and validation. Circulation. 2009 Jan 27;119(3):468-78.
Submit your case here
COTW handling editor: Sohrab Fratz
Have your say: What do you think? Latest posts on this topic from the forum







