Case from: Vijay Anand Dhakshinamurthy and Mark Westwood
Institute: London Chest Hospital, Bart and the London NHS Trust, London, United Kingdom
Clinical history: A 45 year old male smoker with hyperlipidemia presented with out of hospital VF arrest that was preceded by central chest pain. Spontaneous circulation was restored after one cycle of CPR and defibrillation. Post resuscitation ECG demonstrated sinus rhythm with anterior ST depression and an elevated troponin I (1.3 ng/ml). He was transferred to a primary PCI centre via his local district general hospital. No obstructive coronary disease was reported on coronary angiography (Movies 1 & 2 – right click to enlarge) yet there was anteroapical hypokinesis on LV cine angiography (Movie 3).

Movie 1 & Movie 2
Movie 3
He was referred for a CMR study for further evaluation.
CMR Findings: The CMR demonstrated preserved left ventricular function (LV Ejection fraction: 55%). T2 weighted imaging revealed two discrete areas of increased signal intensity in the lateral wall (basal to apical LV segments) and the apical anterior wall (Figures 1 & 2 – click to enlarge). There was basal to apical lateral hypokinesis (Movie 4). The delayed enhancement images demonstrated two areas of discrete infarction involving the lateral and apical anterior wall with two non-viable segments (Figure 3). The peak troponin rise was 3.7 ng/ml.
The LVOT cine images (Movie 5) showed a small mobile mass attached to the posterior aortic wall (1 x 0.3 cm). This mass appeared bright on T2-STIR sequence and was avascular on perfusion imaging at rest (images not shown).
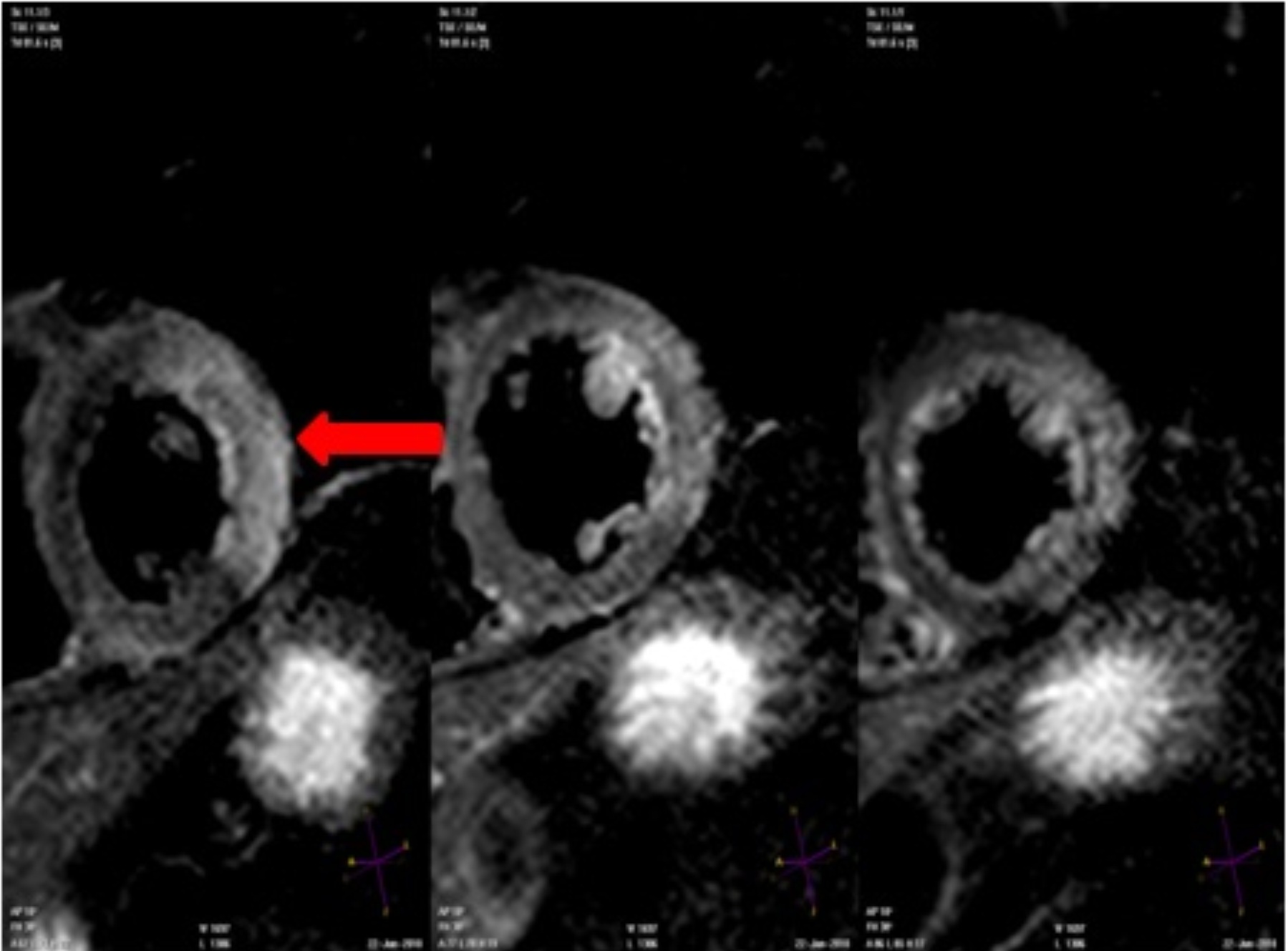
Figure 1: T2-STIR SAX showing myocardial oedema
in the basal lateral wall
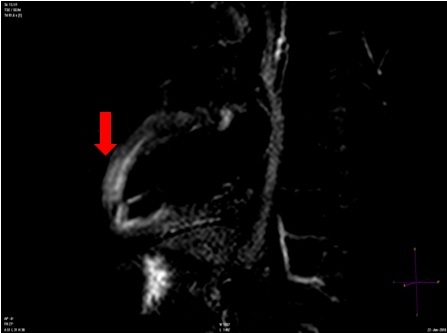
Figure 2: T2-STIR VLA showing myocardial oedema in
the apical anterior wall
Movie 4
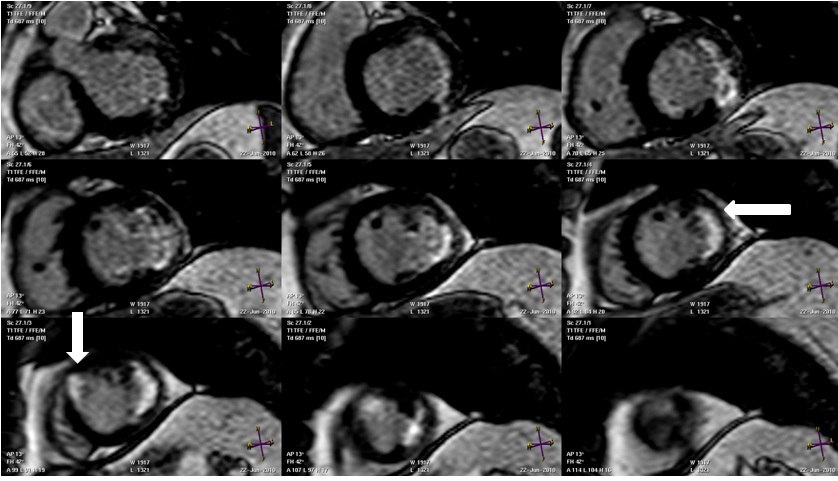
Figure 3: MDE SAX demonstrating two discrete areas
of infarction in the lateral and apical anterior walls
Movie 5: SSFP cine images of the left ventricular outflow tract demonstrating a mobile structure attached to the posterior aortic wall
The initial coronary angiogram was reviewed in the light of the CMR findings. Distal occlusion of the first obtuse marginal branch (Figure 4) was present. Review of the LV cine angiogram also demonstrated a mobile structure in the aortic root (Movie 3).

Figure 4: Left coronary angiography showing occlusion of the first obstuse marginal branch (red arrow)
A transesophageal echocardiogram was also performed to further characterise the aortic lesion. This showed a small mobile strand like structure (1.0 x 0.5 cm) attached to the aortic wall 2 cm above the aortic valve lealfets (Movie 6). The aortic valve appeared to be normal. There was no evidence of a patent foramen ovale or left atrial/ventricular thrombus. The differential diagnosis of this aortic mass included aortic thrombus and fibroelastoma. Although endocarditis was entertained, there were no clinical features to suggest an infective process (no pyrexia, CRP < 5). The patient was commenced on oral anticoagulation with low molecular weight heparin bridging.

Movie 6: Transesophageal echocardiogram long axis view of the aortic outflow tract demonstrating a mobile structure attached to the anterior aortic wall
24 hours later the patient developed a further episode of chest pain with anterior T wave inversion. A CT angiogram was performed and revealed proximal embolic occlusion of a large OM branch (Figure 5) suggesting a further coronary embolic event. No aortic mass was seen on the cine images of the CT coronary angiogram however the aortic wall appeared thickened and irregular (image not shown).
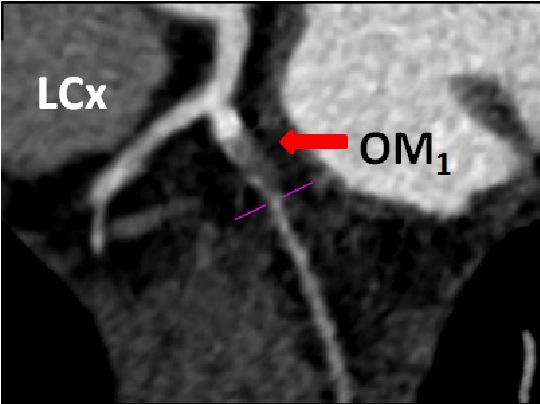
Figure 5: CT coronary angiogram shows proximal occlusion of the first OM branch (red arrow)
Conclusion: Given the concern for fibroelastoma versus thrombus resulting in recurrent cardiac events, the patient underwent surgical exploration of the aortic root. This revealed a thickened, irregular aorta and the presence of atheroma without adherent thrombus. Biopsy of the aortic root was consistent with aortic atherosclerosis and did not reveal any evidence of tumour.
Perspective: CMR is valuable in the assessment of cardiac masses due to its versatility in image planes and tissue characterisation abilities1. In this case CMR was vital in identifying the underlying abnormality. Papillary fibroelastoma is the second commonest benign cardiac neoplasm after myxoma and accounts for 5% of all cardiac tumours. It occurs on the endothelial surface typically attached to the valve leaflets in 75% of cases. Due to their size, they may not be always visualised by CMR. Echocardiography is more sensitive for visualising fibroelastomas, but CMR can complement echocardiography by demonstrating cardiac embolic complications. The clinical presentation of a fibroelastoma varies from asymptomatic presentation to thromboemolic phenomena, myocardial infarction, congestive heart failure, stroke and sudden cardiac death2. Despite the benign nature of this tumour it carries a high thromboembolic risk. Surgical resection should be considered in symptomatic patients and in selected asymptomatic patients based on size, location and mobility of the lesion.
References:
1. Luna A, Ribes R, Caro R, Vida J, Erasmus JJ. Evaluation of cardiac tumors with magnetic resonance imaging. Eur Radiol 2005. 2005;15:1446-55. (Pubmed)
2. Gowda RM, Khan IA, Nair CK, Mehta NJ, Vasavada BG, Sacchi TJ. Cardiac papillary fibroelastoma: a comprehensive analysis of 725 cases. Am Heart J. 2003;146:404–10. (Pubmed)
Submit your case here
COTW handling editors: Kevin Steel & Vijay Anand Dhakshinamurthy
Have your say: What do you think? Latest posts on this topic from the forum







