Case from: Kianoush Ansari-Gilani1 MD, Robert C. Gilkeson1 MD, Arash Aghel2 MD
Institute: 1. Department of Radiology, University Hospitals-Case Medical Center, Cleveland, OH, USA 2. Department of Cardiology, University Hospitals-Case Medical Center, Cleveland, OH, USA
Clinical history: An 18-year-old African American male was admitted to our Emergency Department after developing sudden and severe chest pain, mainly described as chest tightness. He denied any nausea, vomiting, syncope, palpitations, headache, fever, or chills associated with his chest pain. He denied any shortness of breath or lower extremity swelling. Past medical history was negative for any history of cardiovascular disorders; however he reported similar but less severe symptoms approximately 2 weeks and 2 years before the current episode, which had spontaneously resolved without treatment. There was no family history of cardiovascular disease, hypercoagulation or thromboembolic events.
ECG demonstrated sinus rhythm, right axis deviation, anterior T-wave inversions, and changes suggestive of possible right ventricular hypertrophy (Figure 1). Initial troponin T was minimally elevated (0.13 with the upper limit of 0.1 ng/ml) and repeat troponin T was 0.37.

Figure 1: ECG showing sinus rhythm, right axis deviation, anterior T-wave inversion, and changes suggestive of possible right ventricular hypertrophy (click to enlarge).
An echocardiogram revealed right ventricular enlargement with evidence of right ventricular pressure and volume overload (Movie 1).

Movie 1. Apical four chamber view echocardiogram of the heart showing right ventricular enlargement with evidence of right ventricular pressure and volume overload.
CMR Findings: A Cardiac Magnetic Resonance (CMR) was performed to further investigate the cause of his chest pain. Given the signs of right ventricular pressure overload on echocardiogram the possibility of intracardiac shunts were also to be evaluated with CMR.
ECG gated true FISP images demonstrated global right ventricular hypokinesia with mild increase in right ventricular dimensions (Movie 2). There was no evidence of intracardiac shunt.


Movie 2. Global right ventricular hypokinesia with mild increase in right ventricular dimensions and septal flattening.
T2-weighted images showed no evidence of edema. Delayed contrast enhancement sequences performed after the IV administration of gadolinium, showed no evidence of abnormal gadolinium uptake.
Evaluation of the great vessels on the multiplanar true FISP sequence demonstrated filling defects within the right and left main pulmonary arteries suspicious for pulmonary emboli (PE) (Figure 2). Reevaluation of the included lung parenchyma on the rest first pass myocardial perfusion sequences demonstrated areas of parenchymal hypoperfusion (Movie 3).
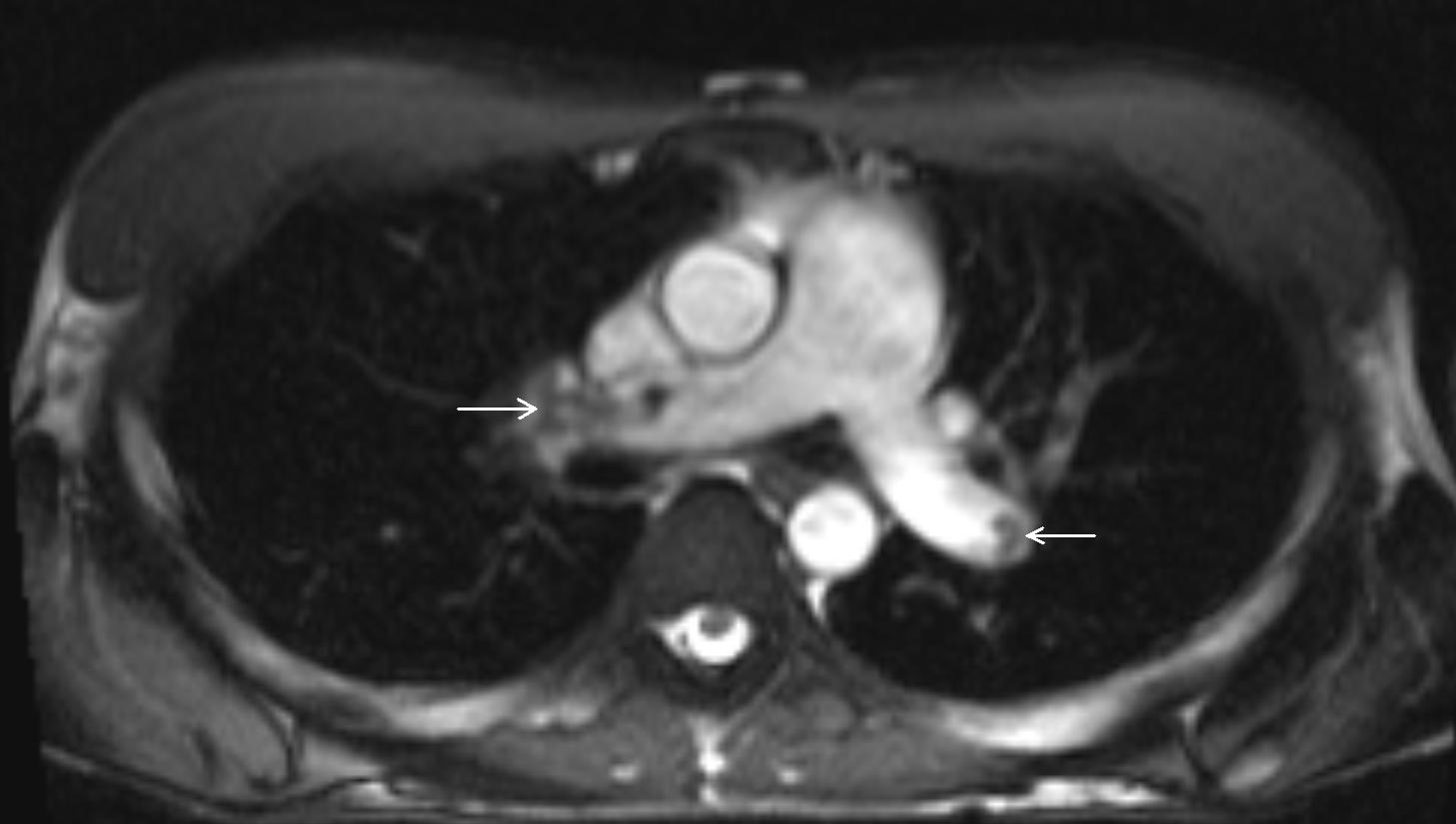
Figure 2. Axial MR image of the heart showing multiple filling defects in the main pulmonary arteries, suggestive of pulmonary embolism (arrows).
Movie 3. Rest first pass myocardial perfusion MR sequences demonstrating areas of parenchymal hypoperfusion.
Computed Tomography (CT) using PE protocol was performed to confirm the CMR findings. CT scan confirmed the presence of multiple filling defects consistent with pulmonary emboli (Figure 3). CT coronal reconstructed images also showed evidence of bronchial artery hypertrophy (Figure 4), suggesting chronic pulmonary thromboembolic disease (chronic PE).
Reconstructed images from the coronal true FISP sequences confirmed bronchial artery hypertrophy (Figure 5)

Figure 3. Axial CT of the chest at the level of the pulmonary arteries, showing multiple filling defects, compatible with multiple pulmonary embolisms (arrow).

Figure 4. Coronal reconstructed CT of the chest showing evidence of bronchial artery hypertrophy (arrow).

Figure 5. MR coronal reconstructed image, showing bronchial artery hypertrophy (arrow), suggesting chronicity of pulmonary embolism.
Perspective: In this case CMR was done to evaluate cause of chest pains and/or associated congenital heart disease (CHD) causing RV overload in a young patient. The finding of filling defects in the pulmonary artery and its branches were consistent with PE which was confirmed on CT scan.
MRI is an ideal imaging modality for evaluating a patient with chest pain as it is uniquely able to integrate, in a single examination, an accurate quantitative assessment of ventricular function, ischaemia, structural abnormalities of the myocardial tissue including edema, infarct size, and myocardial salvage as well as its microvascular abnormalities1. Furthermore, high resolution MR angiography may diagnose proximal arteries PE2-5 or aortic dissection6.
In our case, CMR did not show evidence of myopericarditis and excluded intracardiac shunts as the possible reasons for patient’s clinical manifestations. Though not suspected clinically, because of patient’s young age, the imaging capabilities of CMR established the diagnosis of pulmonary embolism and enabled to start correct treatment. Patient was started on anticoagulation medication. Further workup was not able to identify the source of emboli and screening for hypercoagulable state was negative.
References:
1. Eitel I, Friedrich MG. T2-weighted cardiovascular magnetic resonance in acute cardiac disease. J Cardiovasc Magn Reson. 2011; 13:13.
2. van Langevelde K, Tan M, Srámek A, Huisman MV, de Roos A. Magnetic resonance imaging and computed tomography developments in imaging of venous thromboembolism. J Magn Reson Imaging. 2010; 32:1302-12.
3. Kanne JP, Lalani TA. Role of computed tomography and magnetic resonance imaging for deep venous thrombosis and pulmonary embolism. Circulation. 2004; 109:I15-21.
4. Fink C, Ley S, Puderbach M, Plathow C, Bock M, Kauczor HU: 3 D pulmonary perfusion MRI and MR angiography of pulmonary embolism in pigs after a single injection of a blood pool MR contrast agent. Eur Radiol 2004; 14:1291-6.
5. COTW: Number 09-19: Pulmonary embolism by CMR.
6. Nienaber CA, Spielmann RP, von Kodolitsch Y, Siglow V, Piepho A, Jaup T,Nicolas V, Weber P, Triebel HJ, Bleifeld W: Diagnosis of thoracic aortic dissection. Magnetic resonance imaging versus transesophageal echocardiography. Circulation 1992; 85:434-47.
COTW handling editor: Giovanni Quarta
Have your say: What do you think? Latest posts on this topic from the forum





