CASE FROM:
Authors: Jason Darrah, MD ; Raju Ailiani, MD, FACC.
Institute: Gundersen Lutheran Medical Center, La Crosse, Wisconsin, USA.
Clinical history: A 74 year old gentleman with history of CABG and preserved left ventricular ejection fraction (LVEF) and a chronic left bundle branch block (LBBB) presented with chest pain. Prior CABG included a vein graft to RCA. Electrocardiogram (ECG) revealed previously known chronic LBBB and no acute changes. He was treated with Intravenous (IV) Nitroglycerin as a part of acute coronary syndrome protocol which reduced his chest pain. However, after a few minutes, he became profoundly hypotensive without and lost consciousness. Rhythm monitoring showed a slow junctional rhythm at about 30 beats per minute. Cardiopulmonary resuscitation was begun with fluid resuscitation and chest compressions. On revival he remained profoundly hypotensive despite normal heart rate, requiring large amount of IV fluids and vasoconstrictors.
An bed side echocardiogram ( Movies 1 and 2) which was of limited quality showed preserved left ventricular systolic function with septal wall motion abnormality consistent with LBBB, severely hypokinetic and enlarged right ventricle and moderate to severe tricuspid regurgitation. Troponin level was elevated at 1.2ng/ml. His initial hemoglobin also returned at a very low level of 6.9 g/dl which was normal previously. His hemodynamics were supported with IV fluids, packed red cell transfusion, vasoconstrictors and Intra Aortic Balloon Pump (IABP). Differential diagnoses included acute isolated right ventricular infarction complicated by reduced preload due to IV Nitroglycerin causing profound hypotension and cardiorespiratory collapse. Abdominal ultrasound exam revealed large amount of free fluid suggestive of intra abdominal hemorrhage. His over all picture was against the diagnosis of cardiogenic shock due to a massive left ventricular myocardial infarction. An emergent laparotomy revealed large amount of peritoneal hemorrhage with a liver laceration which was repaired. Following this, his hemodynamics improved rather dramatically. This likely resulted from a liver laceration caused by vigorous chest compressions during CPR causing persistent profound hypotension. Additional diagnoses of acute pulmonary embolism and CPR related tricuspid valve damage causing significant tricuspid regurgitation and acute RV volume overload were also entertained but were felt to be less likely. ECG even with right precordial leads was unhelpful due to underlying LBBB . Echo images were sub optimal to make a diagnosis of isolated RV infarction unequivocally.
He improved gradually but his course was complicated by atrial fibrillation and acute renal failure. He continued to have chest pains. Repeat transthoracic echo was difficult due to poor windows given his recent CABG and laparotomy. Trans esophageal echo also did not provide good enough images. At this point, there were a few questions – was the diagnosis of isolated RV infarction secure; what was the cause of significant tricuspid regurgitation ( was it functional due to RV dysfunction or due to tricuspid valve pathology especially CPR related tricuspid valve injury); was the LV systolic function indeed preserved. A cardiac MRI was requested.
Movie 1 & Movie 2
First Cardiac MRI findings: Initial cardiac MRI ( Movie 3 and 4) was limited due to atrial fibrillation and non use of contrast in view of his renal failure. Limited real time cine images revealed severely hypokinetic to akinetic areas of RV free wall with moderately dilated right ventricle and dyskinetic but thickening interventricular septum and other wise preserved LV wall motion and estimated LVEF of 45%. With these findings, the diagnosis of isolated RV infarction was felt to be fairly secure.

Movie 3 & Movie 4
Subsequent clinical course: After recovery of his renal function, the treating cardiologist felt that coronary and graft angiography would be reasonable to corroborate the findings of other tests done thus far especially as the patient continued to complain of intermittent although rather atypical chest pains thereafter. Coronary angiography ( Figure 1 – pre CABG and 2 – current) showed preserved left coronary circulation and totally occluded non dominant RCA in its mid portion and an occluded vein graft to the acute marginal branch of RCA. No interventions were performed. This further supported the diagnosis of isolated RV infarction initially complicated by preload reduction with IV Nitroglycerin and further complicated by hemorrhagic shock caused by CPR related liver laceration. He made a good recovery with supportive care. A follow up cardiac MRI was requested to reevaluate his RV function and tricuspid regurgitation. This was a more detailed study as patient was more cooperative, his rhythm had been restored to sinus and MR contrast was used as his renal function had returned to normal.
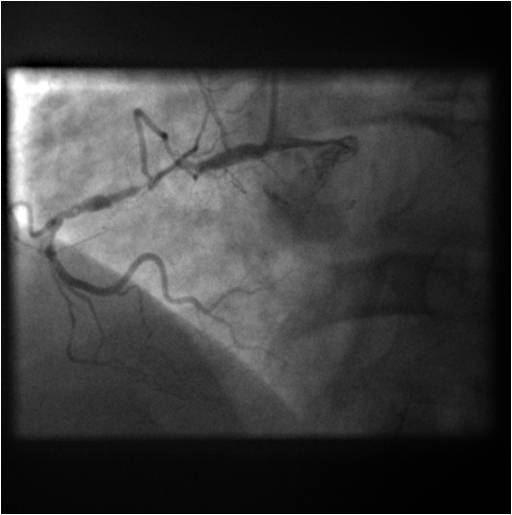
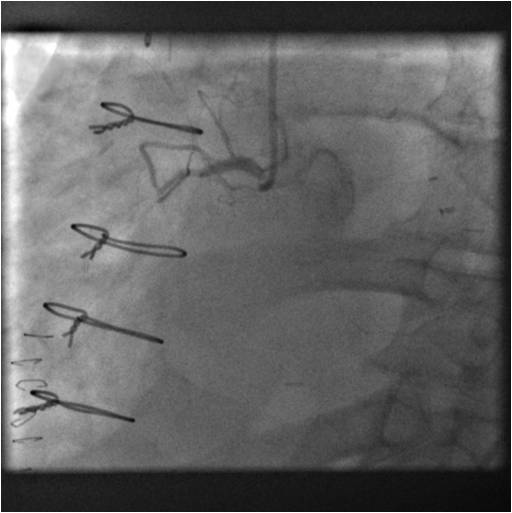
Figure 1 & Figure 2
Follow up Cardiac MRI findings: LV wall motion was normal except septal dyskinesis due to underlying LBBB with LVEF of 51%. RV showed regional focal hypokinesis/akinesis ( Movie 5, 6 and 7). RV appeared dilated in some views but calculated RV volume was not high. RV end diastolic volume was 131ml, RV end systolic volume was 67 ml, RV stroke volume was 64 ml and RVEF was 49.1%. Delayed hyper enhancement was seen post contrast on infarct imaging sequences in RV free wall corresponding to the areas of wall motion abnormalities ( Fig. 3 and 4) without any significant delayed hyper enhancement seen in LV myocardium, confirming the diagnosis of isolated RV infarction. Based on RV stroke volume and RV out flow tract ( RVOT) forward flow measurements, there was felt to be only mild tricuspid regurgitation with RV stroke volume of 64ml and RVOT forward volume of 49ml, rendering tricuspid regurgitant volume of only 15ml. Tricuspid valve was structurally normal. Right atrium appeared to be at least moderately dilated.

Movie 5 & Movie 6
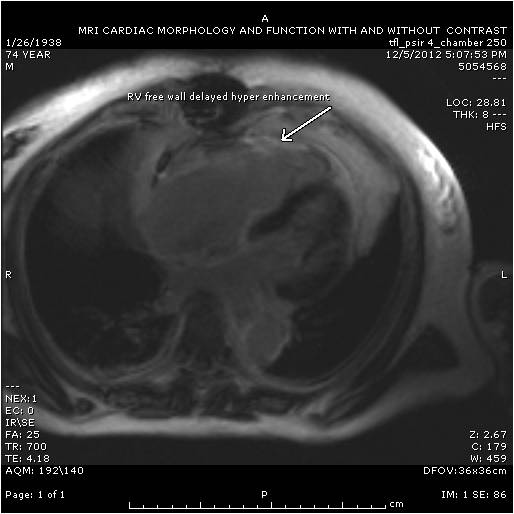
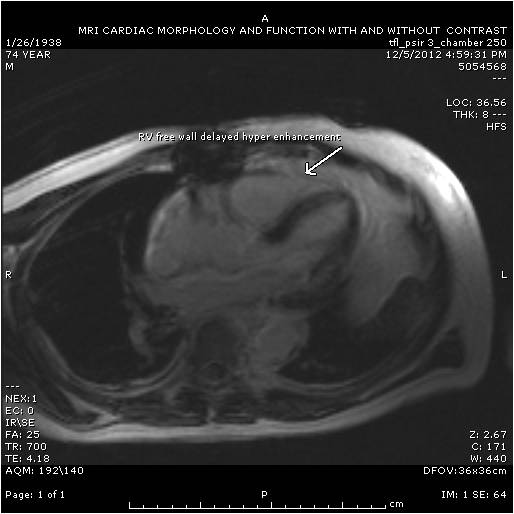
Figure 3 & Figure 4
Conclusion: Acute isolated right ventricular infarction in a patient with pre existing chronic left bundle branch block due to occlusion of native non dominant right coronary artery and its vein graft four days after coronary artery bypass grafting complicated initially by profound hypotension due to associated mild bradyarrythmia and iatrogenic pre load reduction due to Nitrate therapy and further complicated by hemorrhagic shock due to CPR related liver laceration
Perspective:
Learning points from this case include:
- Isolated RV infarction is rare but should be suspected in patients with unexplained profound hypotension and as one of the causes of pulseless electrical activity.
- ECG with right precordial leads in general has good sensitivity to diagnose isolated RV infarction but in the presence of LBBB, sensitivity is limited.
- A bed side echo is very helpful with a suspected diagnosis of acute isolated RV infarction.
- Cardiac MRI with its high resolution capability in identifying RV regional wall motion abnormalities versus global RV systolic dysfunction along with post contrast infarct imaging capability serves as a good definitive test to diagnose RV infarction.
- Real time cine MRI, in patients with arrhythmias affecting gating, although some what low in resolution, provides useful information in certain clinical settings.
- In patients with refractory profound hypotension after recovery of spontaneous circulation post CPR, especially with preserved LV function, a high suspicion needs to be maintained for CPR related visceral injuries and internal bleeding.
References:
- Right Ventricular Infarction – Diagnosis and Treatment; Showkat A. Haji, M.D. and Assad Movahed, M.D., FACP, FACC; Clin. Cardiol. 23, 473–482 (2000).
- Assessment of Isolated Right Ventricular Myocardial Infarction by Magnetic Resonance Imaging; Tareq Ibrahim, Markus Schwaiger and Albert Schömig; Circulation. 2006;113:e78-e79.
- Wellens, H. Right ventricular infarction. New England Journal of Medicine. 1993;328:1036-1038.
- Kakouros, N., Cokkinos, D.V. Right ventricular myocardial infarction: pathophysiology, diagnosis, and management. Postgraduate Medical Journal. 2010;86:719-728.
- Yadav, H., et al. Selective right ventricular impairment following coronary artery bypass graft surgery. European Journal of Cardiothoracic Surgery. 2010;37:393-398.
- Katsuji, I., et al. Pure right ventricular infarction. Circulation Journal. 2002;66:213-215.
- Lainscak, M., Pernat, A. Importance of bedside echocardiography for detection of unsuspected isolated right ventricular infarction as a cause of cardiovascular collapse. American Journal of Emergency Medicine. 2007;25:110-114.
- Braat, S. et al. Value of electrocardiogram in diagnosing right ventricular involvement in patients with an acute inferior wall myocardial infarction. British Heart Journal. 1983;49:368-372.
- Gillies, M., Hogarth, I. Liver rupture after cardiopulmonary resuscitation during peri-operative cardiac arrest. Anaesthesia. 2001;56:387-388.
- Camden, J., Carucci, L. Liver injury diagnosed on computed tomography after use of an automated cardiopulmonary resuscitation device. Emergency Radiology. 2011;18:429-431.
COTW handling editor: Vikas K. Rathi
Have your say: What do you think? Latest posts on this topic from the forum







