Case from: Kaoru Tanaka M.D., PhD1, Guy Van Camp M.D., PhD2, Douwe E Verdries M.D. 1, Johan De Mey M.D., PhD1
Institute: Department of Radiology1 and Department of Cardiology2, UZ Brussel, Brussels, Belgium
Clinical history: A 40 year-old male with no significant past medical history was referred for a chest CT due to the discovery of an enlarged pulmonary artery on routine chest x-ray. The patient was minimally symptomatic but complained of chest heaviness when lying on his left side. A grade III/VI systolic murmur was auscultated over the pulmonary artery.

Figure 1 Contrast enhanced chest CT showing dilated pulmonary trunk and left main pulmonary artery extending to the distal left pulmonary artery
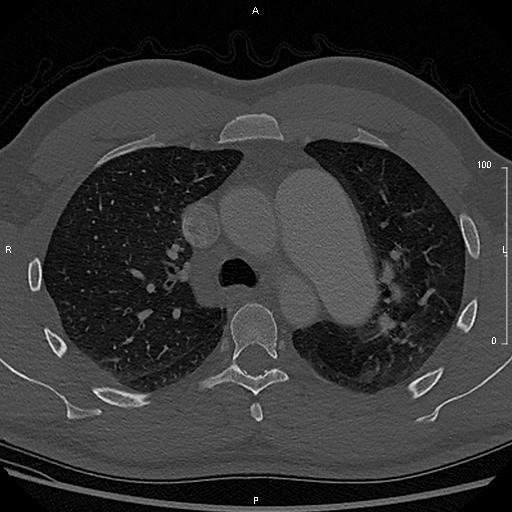
Figure 2 Chest CT showing mosaic perfusion in the left upper lobe due to the dilated pulmonary artery
A non-ECG gated chest computed tomography (CT) with contrast showed dilated pulmonary trunk (up to 48mm) and left pulmonary artery (up to 46mm) extending to the distal left pulmonary artery (Figure 1). Chest CT also showed mosaic perfusion in the left upper lobe due to the dilated pulmonary artery (Figure 2).
Transthoracic echocardiography showed mild pulmonary stenosis with a pressure gradient of 35mmHg and mild pulmonary regurgitation. The aortic valve was tricuspid without any abnormalities. Pulmonary hypertension was ruled out. The patient was referred for a CMR for a further assessment of the pulmonary valve.
CMR Findings:


Movie 1: RVOT cine by CMR demonstrates severe dilatation of the pulmonary trunk and left pulmonary artery, accelerated flow through the pulmonary valve, and pulmonary regurgitation.
Movie 2: Pulmonary valve cine imaging shows a quadricuspid pulmonary valve.
Right ventricular outflow tract (RVOT) cine view by CMR (Philips Achieva 1.5 T) demonstrated severe dilatation of pulmonary trunk and left pulmonary artery, accelerated flow through the pulmonary valve, and pulmonary regurgitation (Movie 1). Subsequent pulmonary valve cine imaging showed a quadricuspid pulmonary valve (Movie 2). The anterior and the right cusp were equal in size and the left cusp was divided into two smaller cusps.

Figure 3: CMR flow quantification showing mild pulmonary stenosis with maximum velocity of 3.3 m/sec and moderate pulmonary regurgitation with regurgitant fraction of 30%
The flow quantification showed a mild pulmonary stenosis with maximum velocity of 3.3 m/sec and mild pulmonary regurgitation with a regurgitant fraction of 30% (Figure 3). This corresponded to the echo findings
Movie 3: The four chambers cine imaging shows normal right and left ventricular systolic function with mild tricuspid regurgitation and slightly prominent trabeculation of RV, and also a dilated distal branch of the left pulmonary artery
The four chambers cine imaging showed normal right and left ventricular systolic function, mild tricuspid regurgitation, slightly prominent RV trabeculations, and a dilated distal branch of the left pulmonary artery (Movie 3). No other congenital abnormalities, such as patent ductus arteriosis, atrial septal defect or ventricular septal defect were found.
Conclusion & Perspective: The anatomy of the pulmonary valve is difficult to assess by echocardiography. The quadricuspid pulmonary valve (QPV) has been considered to be a relatively rare congenital anomaly (from 1 in 400 to 2,000 autopsies), though there have been more case reports published in the last 5 years due to the increase use of CMR and ECG-gated CT. Our case demonstrates both mild pulmonary stenosis and regurgitation, but a QPV is usually clinically benign.
The pulmonary aneurysm has also been considered to be uncommon (1 in 14,000 autopsies). However, three case reports of the QPV with the pulmonary aneurysm have been published since 2009: two cases of QPV and idiopathic pulmonary aneurysm1, 2, and one case of QPV with post-stenotic dilatation of the pulmonary artery3. Nollen et al have well described that the pulmonary aneurysm might be accompanied by congenital heart disease, infectious disease, connective tissue disease, Behcets syndrome, pulmonary hypertension, trauma and atherosclerosis2.
A large pulmonary aneurysm needs to be carefully monitored as this could be a cause of a sudden death by rupture, though there are no clinical guidelines for the management of these aneurysms as yet. Muthialu et al has reported a case with successful operation for an idiopathic pulmonary aneurysm of 6cm, and concluded that it is wise to consider intervention for larger asymptomatic aneurysms4.
In our case, a question still remains as to whether the pulmonary aneurysm is idiopathic or whether it is also influenced by the mild pulmonary valve stenosis, or even possibly whether such congenital valve abnormality itself could be linked to abnormal vasculature (akin to bicuspid aortic valve aorthopathy).
Follow-up imaging assessments are planned.
The excellent visualization of pulmonary valve by CMR will surely enable the discovery of more live cases with QPV. In this setting, the presence of other congenital abnormalities or aortic valve disease should always be ruled out. CMR also allows to monitor the size of the pulmonary artery. Equally, the patient with pulmonary aneurysm should always be assessed by CMR to exclude abnormal anatomy of the pulmonary valve or any other underlying pathologies.
References:
1. Delicia I, Lorente G. The pulmonary valve and the pulmonary artery. Eur Heart J. 2009 Oct; 30(19):2326.
2. Olivares-Reyes A, Molina-Bello E, Espinola-Zavaleta N. Congenital quadricuspid pulmonary valve in an adult patient with double valvular lesions and poststenotic dilatation of the trunk and the left branch of the pulmonary artery: a case presentation and review of the literature. Congenit Heart Dis. 2012 Nov-Dec; 7(6): E103-8.
3. Nollen GJ, Kodde J, Beek AM, Res JC, van Rossum AC. Quadricuspid pulmonary valve and left pulmonary artery aneurysm in an asymptomatic patient assessed by cardiovascular MRI. Neth Heart J. 2013 Apr; 21(4):196-8.
4. Muthialu N, Raju V, Muthubaskaran V, Chandrasekar P, Muralidharan S, Kuppanna PJ. Idiopathic pulmonary artery aneurysm with pulmonary regurgitation. Ann Thorac Surg. 2010 Dec;90(6):2049-51.
COTW handling editor: Monica Deac
Have your say: What do you think? Latest posts on this topic from the forum







