CASE FROM: KIRAN K. MALLULA1, UMANG GUPTA1, KEREN HASBANI2
INSTITUTE: 1) RUSH UNIVERSITY MEDICAL CENTER 2) ADVOCATE LUTHERAN GENERAL HOSPITAL
Clinical history: An eighteen-year-old male with history of Acute Myeloid Leukemia in remission presented with acute onset chest pain and shortness of breath. He had multiple admissions for disseminated Candidiasis and pulmonary Aspergillus infections in the past and had been treated with intravenous Amphotericin and Caspofungin. Initial work up during this admission showed elevated acute phase reactants and mildly elevated cardiac troponins. The electrocardiogram showed nonspecific T wave changes in the antero-lateral leads. None of the other laboratory workup was remarkable.
A transthoracic echocardiogram was performed that demonstrated moderate pericardial effusion with no evidence of cardiac tamponade and an abnormality of unknown etiology on the lateral wall of the left ventricle was noted (Movie 1). The effusion was drained and a cardiac MRI was obtained to better delineate the lateral wall abnormality in the left ventricle and cardiac function.
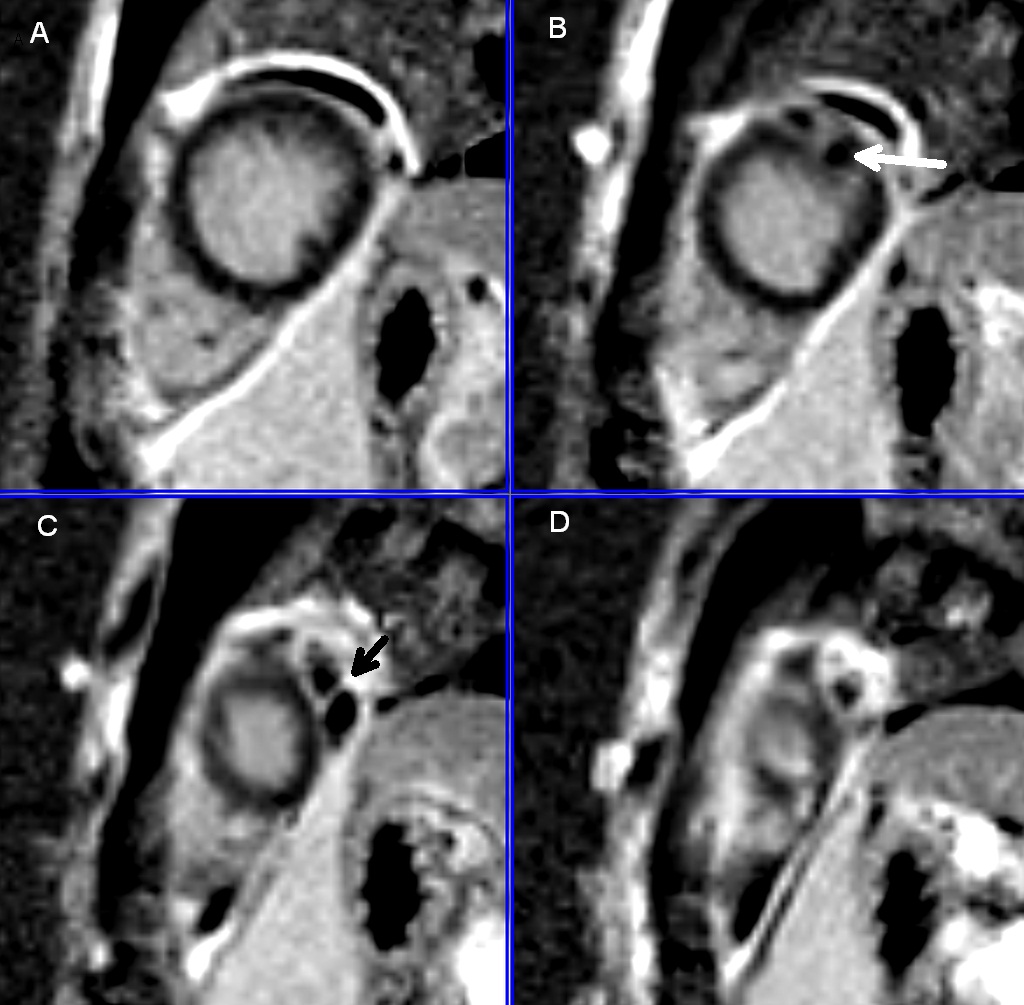
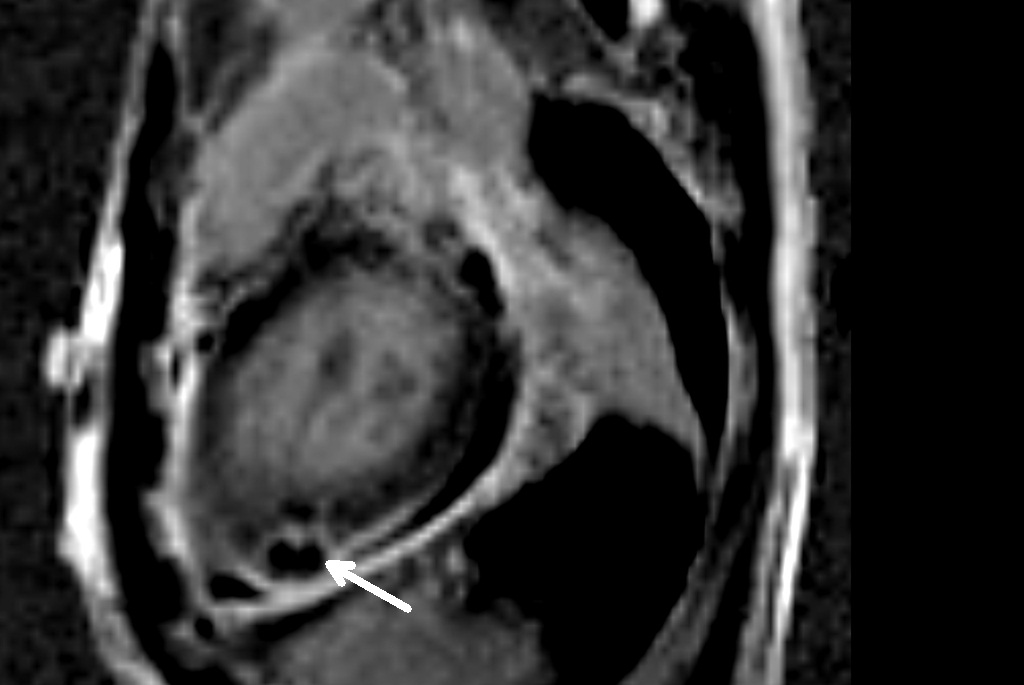
CMR findings: Cine, T2, first pass, and delayed enhancement imaging were all utilized. The cine images showed normal cardiac function, with minimal residual effusion, as well as a sessile mass of different tissue characteristic arising from the lateral wall of the left ventricle (Movie 2).
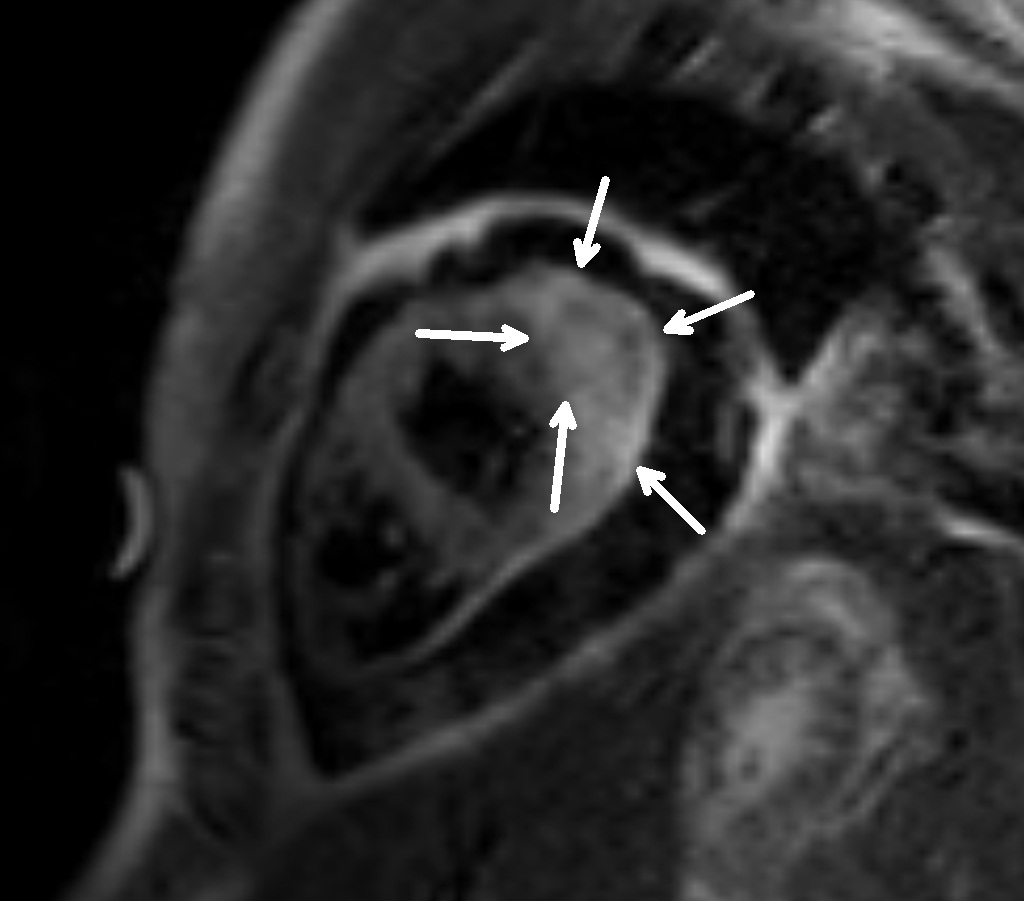
First pass perfusion showed that contrast entered parts of the mass, but the central corre was hypoperfused, therefore a highly vascular lesion was excluded.



Late Gadolinium enhancement showed a well circumscribed lesion embedded in the LV myocardium (Figure 2,3,4).
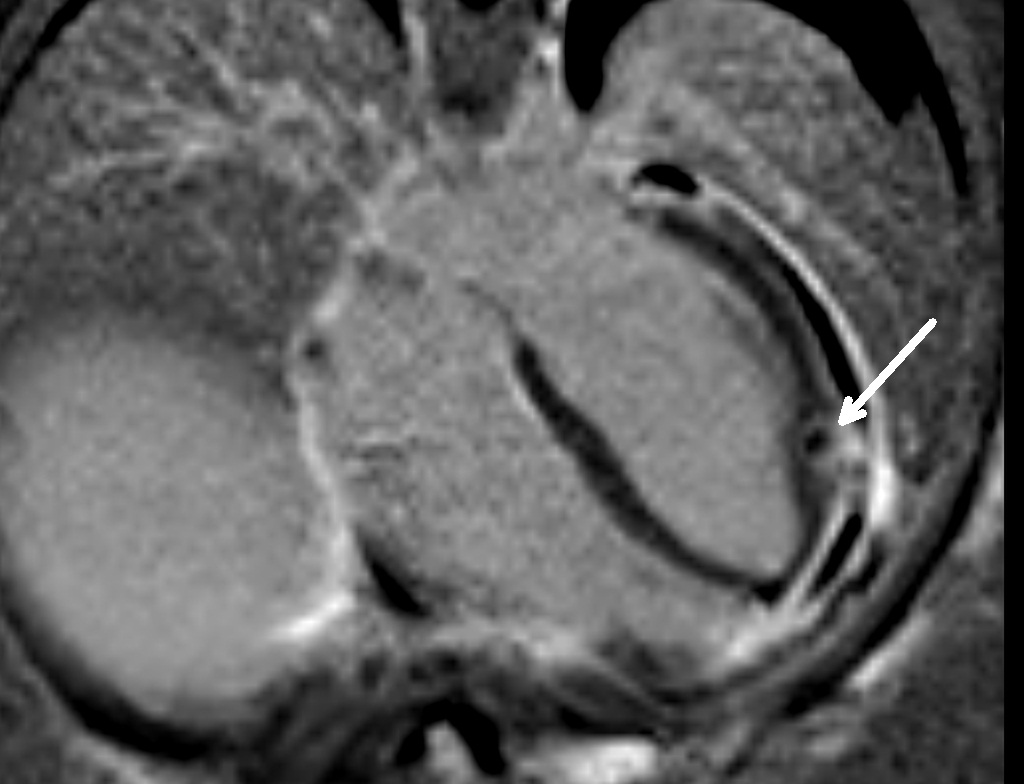
The pericardial fluid that was drained was sent for laboratory analysis, including microbial testing. Cultures were positive for septate mycelia, compatible with a diagnosis of cardiac fungal infection. This, along with the clinical presentation, was diagnostic of a cardiac aspergilloma. Due to rarity of the condition and high degree of fatality associated with the lesion in reported cases in the literature (1-4), the management of the condition posed a dilemma. Surgical resection of the mass and/or direct intralesional injection of amphotericin B were considered as possible approaches but both the ideas were shelved due to fear of spreading the disease to the other uninvolved parts of the myocardium. The final consensus was to initially treat the patient with intravenous amphotericin B with close monitoring of patient’s condition and to repeat CMRs at regular intervals.
A repeat CMR showed no change in the size of the mass, and surgical intervention was once again considered and finally undertaken. Subsequent histological analysis confirmed invasive aspergillosis. He was finally discharged on antifungal therapy to be taken for approximately 1 month after his initial presentation. He has been clinically doing well at latest follow up.
Perspective: Fungal infections account for 1.3-6% of all cases of infective endocarditis [1,2]. The most common fungal organisms causing endocarditis are Candida (62%), followed by Aspergillus (18%) [3]. Though an aspergilloma developing in the lungs of immunocompromised patients is a common complication and is a well described entity, cardiac aspergillomas are rare and much of what is known about this condition comes from early pathological reports [4]. There are few case reports in the literature describing it [5-9]. Most of these descriptions are in immunocompromised individuals similar to our case [7, 9]. Others develop after permanent pacemaker implantation [4, 5]. In all these cases, the diagnosis was presumed by echocardiography and confirmed by direct observation and biopsy of the fungal mass [5-9].
To our knowledge, this is the first description of the cardiac involvement of Aspergillus diagnosed by CMR in a young patient. As this case demonstrates, CMR has distinct advantages when compared to other imaging modalities like echocardiography, in the clinical work-up of cardiac masses. First, it is a non-invasive test, with no radiation. Second, it gives excellent tissue characterization, although the gold standard remains histology.
References:
1. Maderazo EG, Hickingbotham N, Cooper B, et al. Aspergillus endocarditis: cure without surgical valve replacement. South Med J. 1990;83:351-352.
2. Pierrotti LC, Baddour LM. Fungal endocarditis, 1995-2000. Chest.2002;122:302-310.
3. Esmaeilzadeh M, Parsaee M, Peighambari MM, et al. Late occurrence of fatal aortitis: a complication of Aspergillus endocarditis following coronary artery bypass graft surgery. Eur J Echocardiogr.2009;10:165-167.
4. JB Atkinson, DH Connor, M Robinowitz, HA McCalister and R. Virmani, Cardiac fungal infections: review of autopsy findings in 60 patients, Hum Pathol 15 (1984), pp. 935–942.
5. Upadhyayula S, Kapur KK, Seth A.Three-Dimensional Echocardiographic Evaluation of an Aspergilloma Complicating Right Ventricular Permanent Pacemaker Implant. Echocardiography. 2006 Aug;23(7):614-5.
6. Chambers J, Blauth C, Bucknall C, Eykyn S. Images in clinical medicine. Aspergilloma as a complication of pacemaker implantation. N Engl J Med. 2002 Feb 7;346:428.
7. Rubio Alvarez J, Sierra Quiroga J, Rubio Taboada C, Fernandez Gonzalez A, Martinon Torres F, Garcia-Bengochea J. Cardiac Aspergillosis with pedunculated mass in the left ventricle.Tex Heart Inst J. 2004;31:439-41.
8. Chamsi-Pasha H, Abdulmoneim A, Ahmed WH, Al-Shaibi KF, Ajam A, Bakhamees H, Ashmeg AK. Biatrial aspergillosis in a patient with immunocompetency. J Am Soc Echocardiogr. 2004 Jan;17:70-2.
9. Berarducci L, Ford K, Olenick S, Devries S. Invasive intracardiac aspergillosis with widespread embolization. J Am Soc Echocardiogr. 1993 Sep-Oct;6:539-42.
COTW handling editor: Giovanni Quarta, MD
Have your say: What do you think? Latest posts on this topic from the forum





