Case from: Arun Dahiya1,2, Mark Hansen3, Bruno Jesuthasan1,Prasad Challa1
Institutes:
1Logan Hospital, Queensland, Australia
2Royal Brisbane and Women’s Hospital, Queensland Australia
3Qscan Radiology, Queensland, Australia
Clinical history: A 16-year-old boy was found to have an abnormal ECG (Figure 1) during his appendectomy surgery. His background was remarkable for a small muscular VSD, which had undergone spontaneous closure on an echocardiogram performed two years prior. His father had a history of hypertrophic obstructive cardiomyopathy resulting in severe LV systolic dysfunction and requiring heart transplantation. The patient’s echocardiogram and electrocardiograms (Figure 2) performed 2 years ago were not diagnostic of hypertrophic cardiomyopathy. However on this occasion his abnormal ECG led to an Echo followed by CMR. Echo showed mild prominence of the septum and raised the possibility of HCM. Therefore CMR was performed for further delineation.
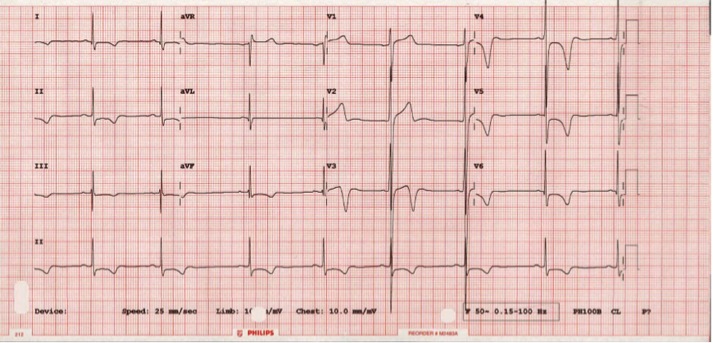
Figure 1. ECG was borderline for LVH by voltage criteria and showed deep t inversion the infero-lateral leads
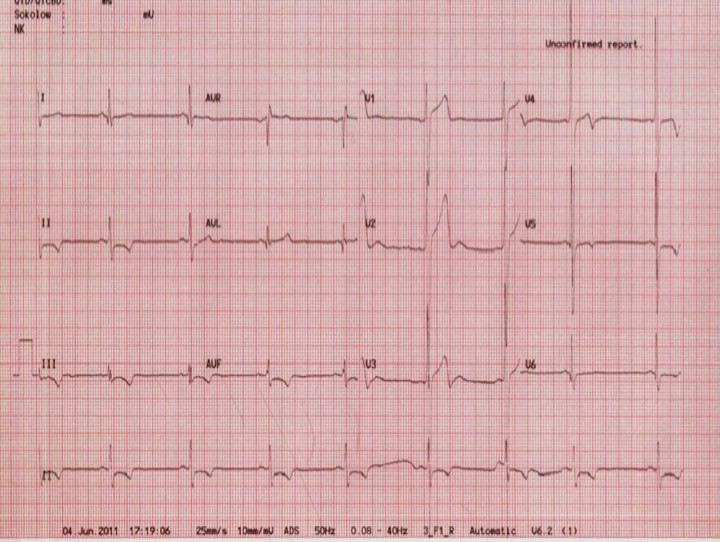
Figure 2. ECG 2 years ago.
CMR Findings: CMR showed asymmetrical hypertrophy of the basal infero-septum (1.6cm, LV mass 60g/m2) with deep intramuscular crypts predominantly involving the infero-septum, inferior wall and anterior wall (Movies 1-4). Overall LV systolic function was normal. Papillary muscles were normal in thickness with normal attachments. There was no LVOT obstruction and there was no obvious VSD seen on this study.

Movie 1 – Two chamber SSFP.

Movie 2 – Three chamber SSFP.
Movies demonstrate asymmetrical hypertrophy of the basal infero-septum with deep intramuscular crypts predominantly involving the infero-septum, inferior wall and anterior wall. Normal aspect of papillary muscles. Movie 2 further demonstrates absence of LVOT obstruction.
Movie 3 – Four chamber SSFP.
Movie 4 – Short-axis SSFP.
Movies demonstrate normal LV systolic function. No obvious VSD seen on these images.
Four chamber perfusion revealed no obvious communication between the left and right (Movie 5). Furthermore flow quantification through pulmonary artery and aorta were not suggestive of significant intra-cardiac shunting (Figure 3).
Movie 5. Four chamber perfusion demonstrating no obvious communication between the left and right ventricle.
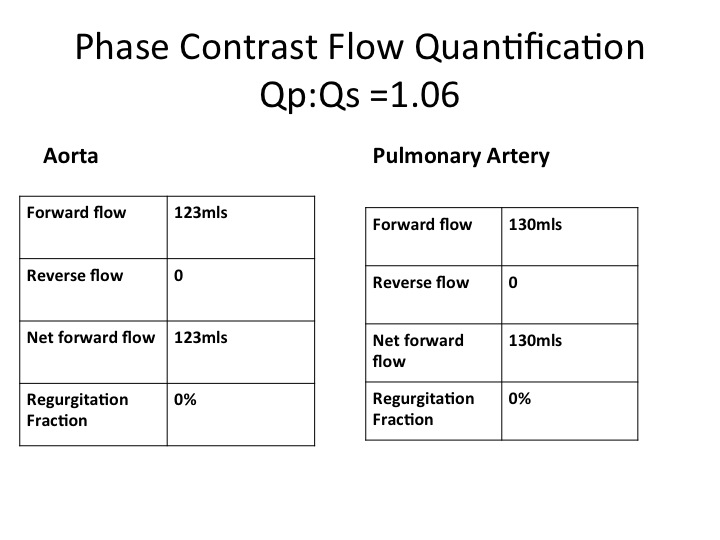
Figure 3. Phase contrast flow quantification.
Post-gadolinium delayed enhancement imaging revealed focal area fibrosis in the thickened septum (Figure 4 and 5).
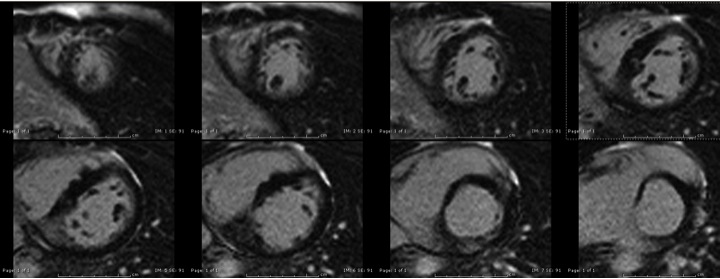
Figure 4. 2D inversion recovery (LGE) in short-axis view demonstrating focal pattern of delayed enhancement in the infero-septal region
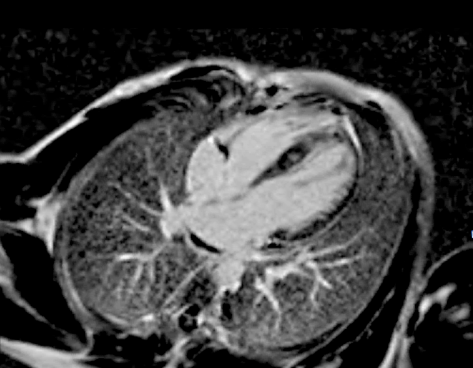
Figure 5. 2D inversion recovery (LGE) in four chamber view demonstrating a focal pattern of delayed enhancement in the septal region.
Conclusion: These findings were consistent with early phenotypic manifestation of HCM in a patient with a family history of HCM. Therefore CMR provided incremental information, which was crucial towards ongoing care of this patient. Subsequent to this study patient was diagnosed with HCM and his family was referred for genetic testing. Results of genetic testing are pending. Patient is not considered for ICD at this stage, as he didn’t have other high-risk features for sudden cardiac death but will be under ongoing surveillance. He was previously involved in active sports therefore it was recommended for him to follow recreational (Noncompetitive) sports activities and exercise guidelines as per the latest AHA/ACCF document.
Perspective: Hypertrophic cardiomyopathy (HCM) is the most common genetic cardiomyopathy with a prevalence of 1:500 in the general population. Cardiac sarcomere mutations form the basis of hypertrophic cardiomyopathy pathophysiology. HCM mutations are transmitted in an autosomal dominant manner therefore each offspring has 50% chance of inheriting the mutation. However phenotypic manifestation of the mutation can be variable with delayed expression at an older age. Unfortunately a genetic mutation is identified in only 40-60% of cases therefore ongoing cardiac imaging surveillance is needed in patients with a family history of HCM (1).
Cardiac MRI has advantages over echocardiography which can be limited by poor acoustic imaging and inaccurate wall thickness measurement because of non co-axial short axis images. The ability of CMR to review the heart in multiple tomographic planes with high spatial and temporal resolution without the use of ionizing radiation makes it the ideal imaging modality for diagnosis and surveillance of HCM family members. Furthermore CMR has a unique ability of identifying myocardial fibrosis by delayed enhancement imaging which is of prognostic value (1).
Due to its superior spatial resolution, CMR can also identify crypts, which can be early phenotypic manifestation of genotype positive but phenotype negative HCM (2). There have been few reports suggesting HCM and LVNC genetic overlap with a recent case report finding HCM and LVNC in members of same family with common genotype mutation (3,4). However in this case, the LV cavity did not have a spongy appearance and LV function was normal. Therefore appearances were not consistent with coexisting LVNC.
We report this case where CMR identified early phenotypic manifestation of HCM in a patient with family history of HCM.
References:
1. Maron MS. Clinical utility of cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 2012;14:13.
2. Maron MS, Rowin EJ, Lin D et al. Prevalence and clinical profile of myocardial crypts in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 2012;5:441-7.
3. Camuglia AC, Younger JF, McGaughran J, Lo A, Atherton JJ. Cardiac myosin-binding protein C gene mutation expressed as hypertrophic cardiomyopathy and left ventricular noncompaction within two families: insights from cardiac magnetic resonance in clinical screening: Camuglia MYBPC3 gene mutation and MRI. Int J Cardiol 2013;168:2950-2.
4. Thavendiranathan P, Dahiya A, Phelan D, Desai MY, Tang WH. Isolated left ventricular non-compaction controversies in diagnostic criteria, adverse outcomes and management. Heart 2013;99:681-9.
COTW handling editor: Pranav Bhagirath





