Case from: Veronica Aliaga, MD, Angela Paola Sánchez-Herrera, MD, Guillem Pons-Lladó, MD.
Institute: Cardiac Imaging Unit, Radiology Department, Clínica Creu Blanca Barcelona, Spain.
Clinical history: An asymptomatic 42 year-old male is submitted for a CMR study after an echo scan showing asymmetric hypertrophy involving the apical segment of the left ventricle. A noticeable highly echogenic signal is described at the endocardial border of the thickened apical region.
CMR Findings: SSFP cine sequences on long- (Videos 1 & 2) and short-axis (Video 3) planes showed a slightly dilated but normally contracting left ventricle, with a definitely increased wall thickness (33 mm) of the apical segment.

Video 1. SSFP 2 chamber
Video 2. SSFP 4 chamber.
Video 3. SSFP short axis.
Delayed contrast enhancement (DCE) sequences on the same orientation (Figures 1-3) showed two distinctive patterns of hyperenhancement of the hypertrophied apical region: one intramyocardial, diffuse (white arrows), and a second one, dense, distributed as a layer at the endocardial border of the apical region of both the left and, also, the right ventricle (black arrows). There was no evidence of intracavitary thrombosis.
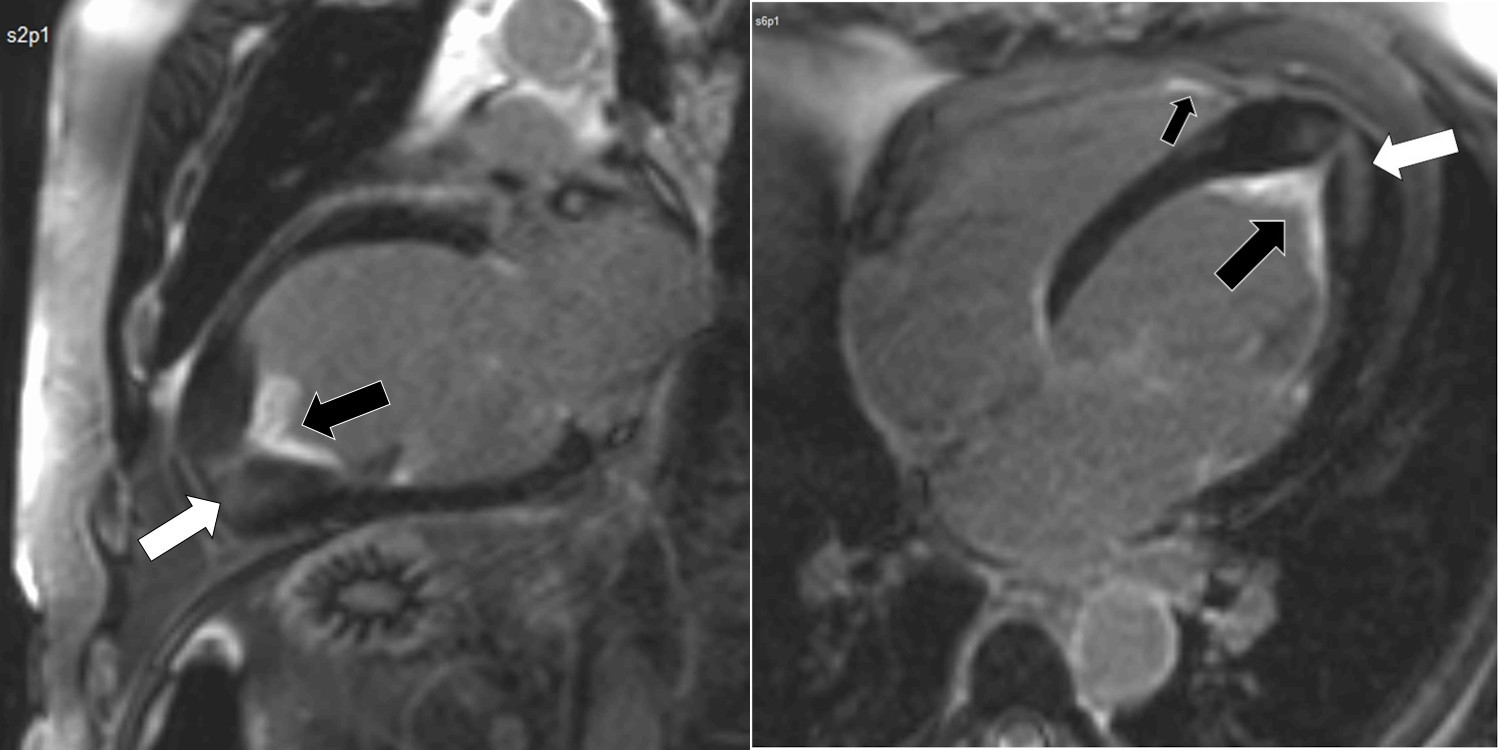
Figures 1 and 2. Delayed contrast enhancement 2 and 4 chamber.
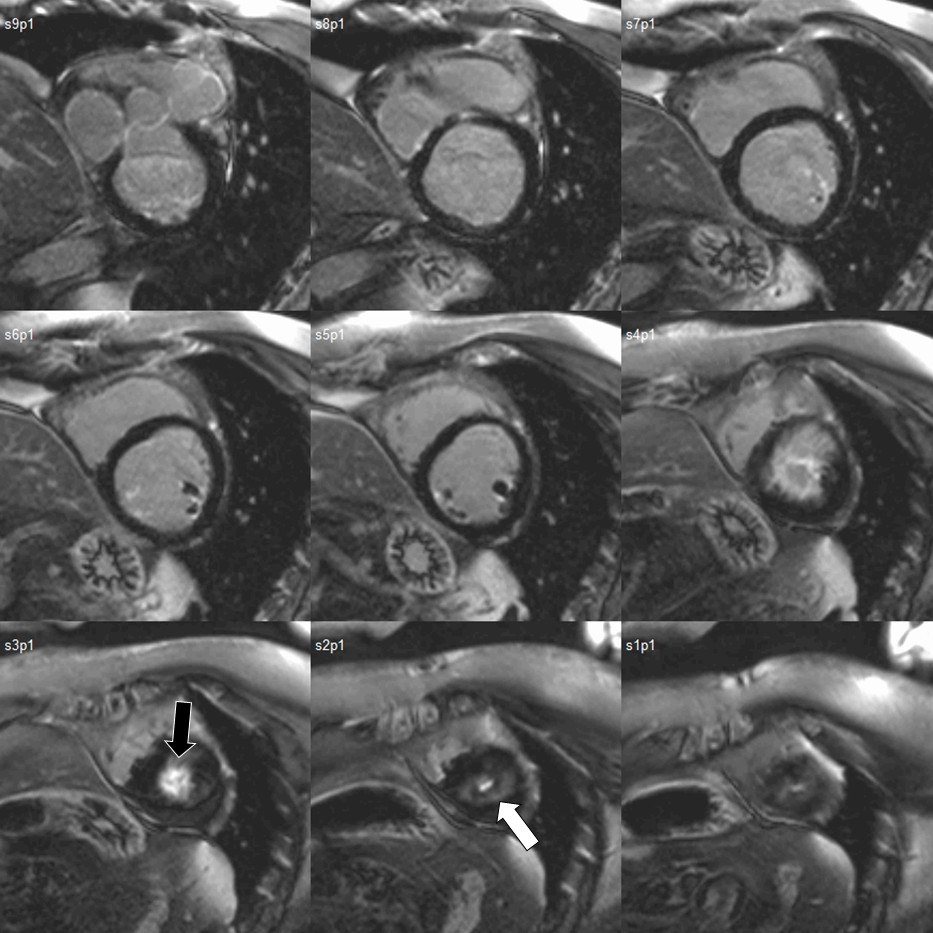
Figure 3. Delayed contrast enhancement short axis.
Conclusion: The CMR findings confirm, on one hand, the clinical suspicion of apical hypertrophic cardiomyopathy, by showing asymmetrically increased myocardial wall thickness of the apical region, with evidence of intramyocardial fibrosis of the hypertrophied segment. On the other hand, the study also shows the coexistence of a second pattern of DCE, characteristic, in this case, of endomyocardial fibrosis, involving both, the right and left ventricular apical regions.
Perspective: Idiopathic hypereosinophilic syndrome (HES) is rare and frequently involves the heart with development of endomyocardial fibrosis, a characteristic restrictive cardiomyopathy with uni- or biventricular endocardial fibrous tissue proliferation, preferably in the apical region and inflow tract, which leads to diastolic dysfunction and, not infrequently, to embolic phenomena arising from an overlying intracavitary thrombus.(1)
Although the diagnosis was initially oriented by echocardiography in this patient, CMR allowed for a confirmation of the presence of both processes given the highly distinctive patterns of DCE in each case.
Cardiac MRI is very useful in differentiating the two entities in this particular case, since the late gadolinium hyper-enhancement in the apical region demonstrates fibrosis occupation and provides a definitive diagnosis of endomyocardial fibrosis, and therefore ruling out the thrombotic component. (2,3)
Although definitive diagnosis would be the demonstration of fibrosis on endomyocardial biopsy, this technique involves invasive embolic risk in this disease.(4)
Therefore, if the diagnosis of Loeffler endocarditis is under suspicion, contrast enhanced cardiac MRI will be very informative. Our case did not have serial imaging available, but a previously reported case has suggested that the endomyocardial lesion in the early stage of Loeffler endocarditis can be regressed by optimal medical therapy.(5)
References:
COTW handling editor: Eddie Hulten, MD







