Case from: Prasanna Sengodan1 MD, James Kennen2 DO, Rajiv Shah2 MD, Sonika Malik1MD, Ashish Aneja1 MD.
Institute: 1Heart and Vascular Center, Case Western Reserve University MetroHealth Campus) Cleveland, Ohio, USA, 2Department of Radiology, Case Western Reserve University (MetroHealth Campus) Cleveland, Ohio, USA.
Clinical history: A 63 year old healthy man was seen in consultation for chest pain and an abnormal electrocardiogram (EKG). He was asymptomatic until about a month prior to initial presentation, when he developed chest discomfort following very strenuous activity (pulling a kayak uphill to his lake house), accompanied by left arm discomfort and minimal shortness of breath. The EKG revealed sinus bradycardia with deep symmetric T wave inversions in anterolateral leads with QT prolongation, along with ST-T wave changes in inferior leads (Figure 1A). A previous EKG done in 2007 was compared and was found to be normal, except for tall T waves in leads V4 – V6, which was considered to be a normal variant (Figure 1B). A transthoracic echocardiogram revealed concentric left ventricular hypertrophy with an ejection fraction of 65% (Figure 2 and Video1). The wall thicknesses measured in the echocardiogram were 16, 15 and 14 mm in the anterior, inferior and lateral walls respectively. The posterior wall thickness was 11mm. Chart review consistently revealed elevated blood pressures in the doctor’s office (140-160 systolic range) but home blood pressure values between 120 to 140 mm Hg were reported. Ambulatory blood pressure monitoring revealed systolic blood pressure values between 130-150 mm Hg. Based upon the abnormal EKG and subtle echocardiographic findings, a diagnosis of apical hypertrophic cardiomyopathy (HCM) was suspected and cardiac magnetic resonance (CMR) imaging was requested.
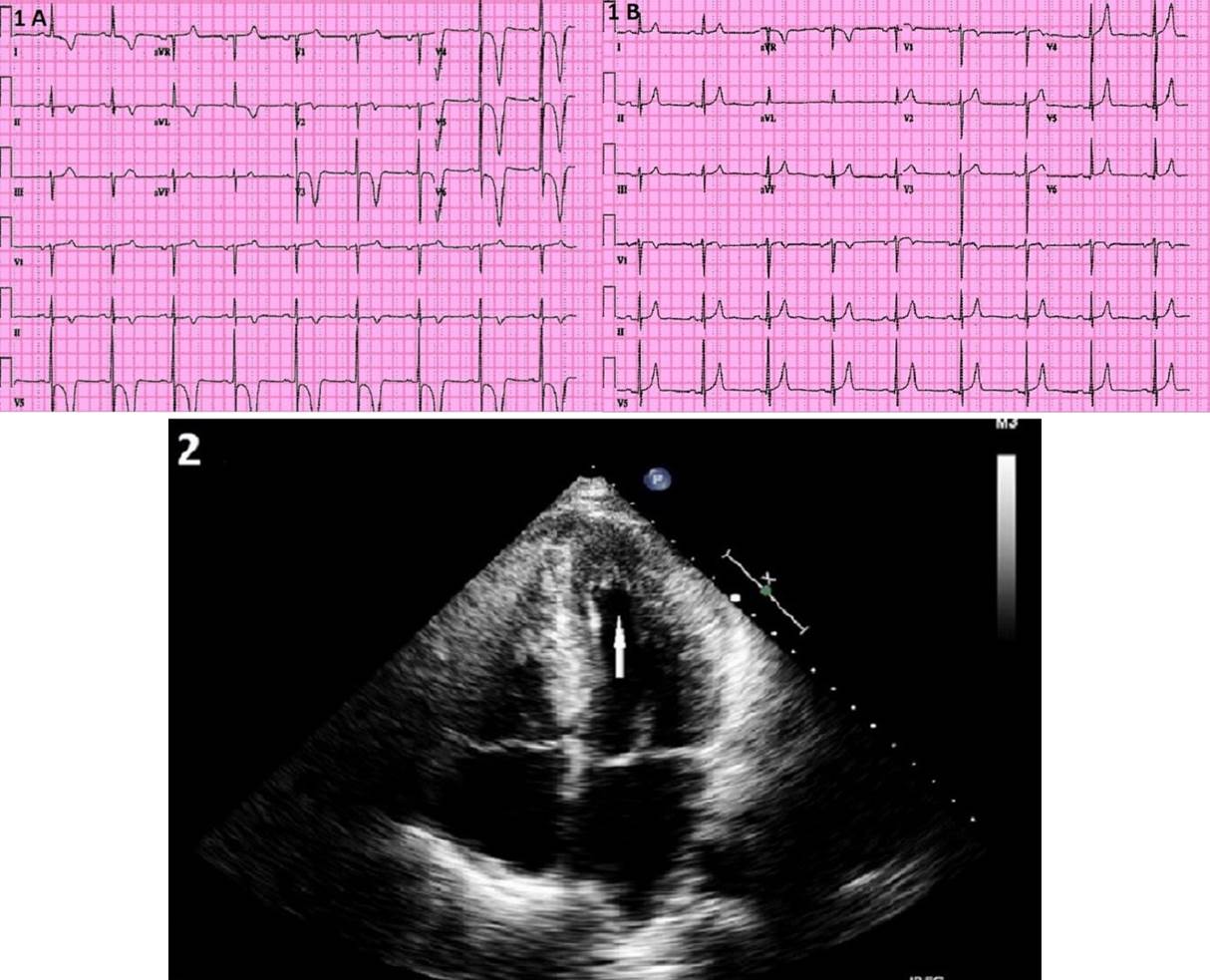
Figures 1 and 2: Patient with new T-wave inversions on EKG (1A, previous EKG is shown in 1B) with echocardiogram demonstrating relative apical hypertrophy on Echocardiography (2).
Video 1: Transthoracic echocardiogram demonstrating 4 chamber view of Apical Hypertrophic Cardiomyopathy
CMR Findings: CMR imaging revealed concentric left ventricular wall thickening without the normally associated tapering of the ventricular wall approaching the apex. No left atrial enlargement, scar or apical aneurysm was observed.(Video 2A, 2B and Video 3 as well as Figures 3A – 3chamber view and 3B – 4chamber view). The actual wall thicknesses on the CMR were 11, 14, 13 and 13 mm in the apical septum, anterior, inferior and lateral apex respectively. The posterior wall thickness was 9.5mm. Figure 4 demonstrates no late gadolinium enhancement (LGE).
Coronary angiography demonstrated no significant coronary artery disease and catheter “Pull back” within the left ventricle revealed no gradient from apex to the base. The patient was started on Lisinopril 10 mg once daily for hypertension control. A beta-blocker was not initiated due to his low resting heart rate of 50.
Video 2A (left): Cardiac magnetic resonance imaging demonstrating relative left ventricular hypertrophy in 3-chamber chamber view. Video 2B (right): Cardiac magnetic resonance imaging demonstrating relative left ventricular hypertrophy in 4-chamber view
Video 3: Short axis SSFP cine images from base to apex.
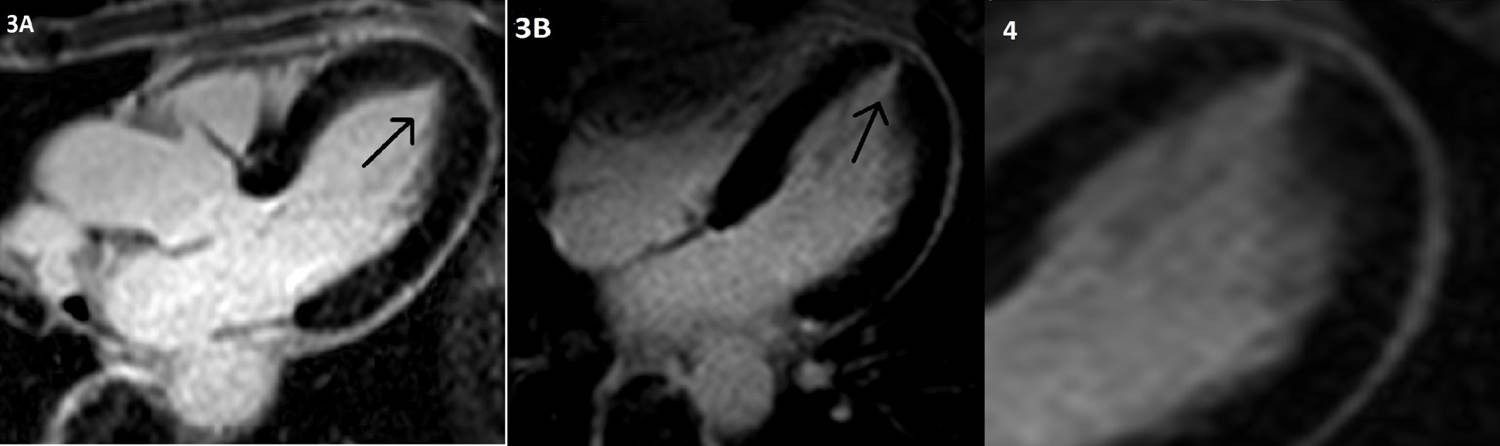
Figure 3 and 4: Concentric left ventricular wall thickening without the normally associated tapering of the ventricular wall approaching the apex (arrow, 3A 3-chamber and 3B, 4-chamber) without any demonstrable LGE (4)
Conclusion: The diagnostic criteria for apical HCM include the demonstration of asymmetric left ventricular hypertrophy (LVH), confined predominantly to the LV apex with an apical wall thickness ≥15 mm and a ratio of maximal apical to posterior wall thickness ≥1.5, based on two-dimensional echocardiography (echo) or MRI (1). Some patients present with EKG changes and symptoms that suggest HCM, but imaging using conventional wall thickness criteria is non-diagnostic (2). Our patient did not meet the conventional criteria for wall thickness as his apical to posterior wall thickness was 1.47 (14:9.5) based on CMR, yet we think our patient has apical HCM (atypical variant), as he had a thickened apical wall and classical EKG findings consistent with deep T wave inversions. It is possible that our patient might have had an extension of wall thickening into other non-apical regions, which could have been missed. One study reported such findings that nearly 50% had extension of wall thickening into other non-apical regions (2).
Perspective: This report enlightens the fact that there are a subset of patients with apical HCM who are a variant from the normal, which merits recognition and treatment. Myocardial infarction incidence among apical HCM patients was found in about 10% of patient in the series of Eriksson et al (1). Screening for first degree relatives has been suggested and is currently being performed. The patient has been doing well without any complaints over a follow up period of 3 months.Screening for first degree relatives has been suggested and is currently being performed.
References:
1. Eriksson MJ, Sonnenberg B, Woo A , et al. Long-Term Outcome in Patients with Apical Hypertrophic Cardiomyopathy. J Am Coll Cardiol 2002;39:638–45.
2. Kebed KY, Al Adham RI, Bishu K, et al. Evaluation of apical subtype of hypertrophic cardiomyopathy using cardiac magnetic resonance imaging with gadolinium enhancement. Am J Cardiol. 2014 Sep 1;114(5):777-82
COTW handling editor: Karima Addetia







