Case from: Juliana Serafim da Silveira, M.D, Jason Craft, M.D, Subha V. Raman, M.D, Subha Ghosh, M.D
Institute: The Ohio State University, Columbus, Ohio, USA
Clinical history:
An 84 year-old man presented after an out-of-hospital cardiac arrest and was successfully resuscitated. His past medical history included chronic obstructive pulmonary disease, diabetes mellitus, coronary artery disease and pulmonary hypertension. During admission a left heart catheterization was performed, revealing diffuse but non-occlusive coronary disease. Echocardiography revealed normal LV systolic function and moderate RV systolic dysfunction with elevated RV systolic pressure. Patient was extubated after catheterization, and had a bout of hemoptysis. A CT pulmonary angiogram was performed to rule out acute pulmonary embolism.
CT imaging : CT demonstrated no signs of pulmonary embolism. Prominent aortic atherosclerosis was present and a circumscribed intermediate density para-aortic lesion was observed adjacent to the descending aorta (Figure 1). There was no contrast enhancement of the lesion.
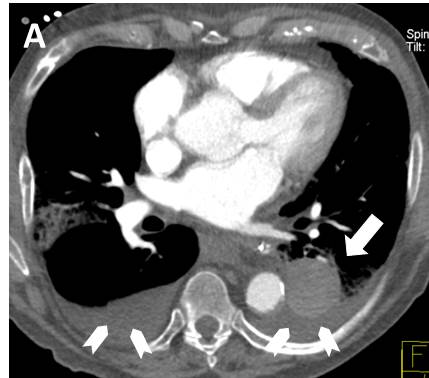
Figure 1a
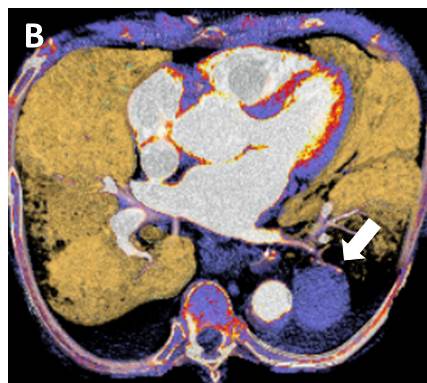
Figure 1b
Figure 1 – Axial contrast enhanced CT (A) and the corresponding volume-rendering image (B). Arrows indicate the intermediate density paraortic mass (+53 Hounsfield units). Note hypodense bilateral pleural fluid measuring +2 Hounsfield units (arrowheads). Also note aortic wall thickening and calcification.
Although there did not appear to be a clear communication between the aorta and the para-aortic lesion, given the extensive aortic atherosclerosis and the para-aortic location, a saccular aortic aneurysm was considered among the differential diagnosis. A dedicated MR study was recommended.
CMR Findings:The para-aortic mass was shown to be hyperintese on both T1 and T2-weighted images (Figure 2).
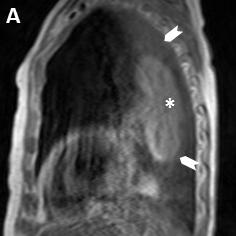
Figure 2a
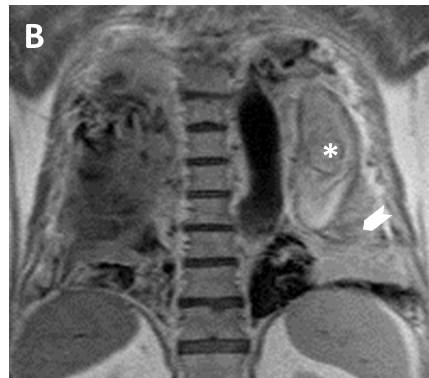
Figure 2b
Figure 2 – (A) Sagital T1-weighted image shows a sausage-shaped hyperintense mass (asterisk) surrounded by pleural fluid (arrowheads). (B) Coronal T2-weighted image shows a well-defined hyperintese lesion with a thin hypointese wall (asterisk). Note that the pleural fluid is hypointese on T1 and hyperintense on T2-weighted images (arrowheads).
First pass perfusion showed absence of mass enhancement (Movie 1); and contrast MR angiography revealed atheromatous aorta with no leak (Movie 2).
Movie 1: First pass perfusion showed absence of mass enhancement
Movie 2: Contrast MR Angiography revealed a diffuse atheromatous descending aorta. No contrast leakage outside the aorta was observed.
These findings excluded the diagnosis of aortic aneurysm. Post-contrast delayed images showed thin walled rim enhancement, suggesting the cystic nature of the lesion (Figure 3).
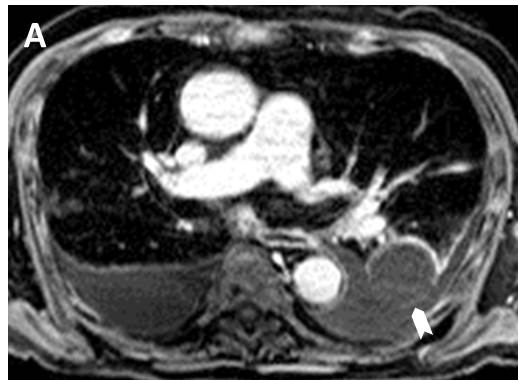
Figure 3a
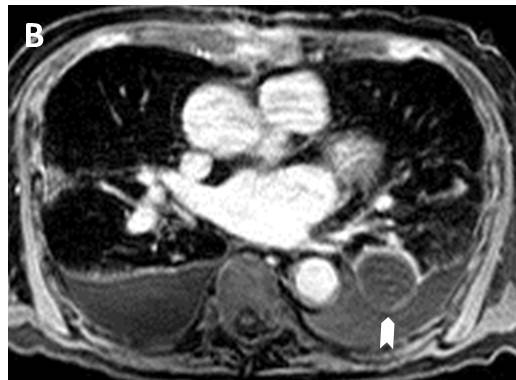
Figure 3b
Figure 3 – Post-contrast delayed images showed thin walled rim of enhancement (arrowheads), suggesting the cystic nature of the lesion. Also note the presence of pleural fluid in between the aorta and the cystic mass.
Conclusion: Hyperintense signal on pre-contrast T1 and T2-weighted images and thin walled rim of enhancement after contrast suggested a cystic lesion with high protein or hemorrhagic content. This suggested an infected bronchogenic cyst, which lead to hemoptysis and septic shock. Significant comorbidities precluded surgical excision. Multifocal parenchymal consolidations were presumed to represent pneumonia, and the patient received prolonged antibiotic therapy.
Perspective: Bronchogenic cysts are congenital lesions resulting from abnormal budding of the embryonic foregut and lung during the first trimester of gestation1. The abnormal bud subsequently differentiates into a fluid-filled blind-ending pouch, and its location varies according to the embryologic stage of lung development at which they appear. Cysts that occur early during bronchial budding and branching are located in the mediastinum and those that occur late, appear within the lung. The later the anomaly develops, the more peripheral it is in the lungs2.
Microscopically, cysts are lined with ciliated, pseudostratified, columnar epithelium3. The fluid within bronchogenic cysts is usually a mixture of water and proteinaceous mucus, and can vary from a very watery fluid to a very viscous mucoid material. Some cysts may have hemorrhagic or purulent content, depending on the presence of hemorrhagic or infectious complications.
Asymptomatic cysts are frequent. Clinical presentations include hemorrhagic complications and infection. Neoplastic transformation is not unusual.
Bronchogenic cysts typically manifest as sharply marginated homogeneous and solitary masses on CT scans4, accompanied by peripheral calcifications in 10% of cases. The attenuation can vary from water to soft-tissue density. After contrast injection, no intralesional enhancement is typically seen but a thin mural enhancement is occasionally reported. On MR imaging, cysts typically have high signal intensity on T2-weighted images regardless of the nature of the cyst contents. Variable cyst contents determine T1 signal characteristics and cysts could be either hypointense or hyperintense on T1-weighted images. If the contents of the cyst are mainly serous, it has low signal intensity on T1-weighted images. On the contrary, cysts with high protein/mucoid content or hemorrhage will show high signal intensity on T1-weighted images. MR imaging can be very useful for differentiating high-attenuating cysts on CT from soft tissue masses.
Conservative treatment has been advocated in asymptomatic adults or in high risk patients, as in this case. The diagnosis of a symptomatic cyst is an indication for resection. Lobectomy is the standard procedure in complicated cysts, as the cyst is always surrounded by areas of atelectasis and pneumonia. Percutaneous catheter drainage and/or alcohol ablation has been performed in selected patients but is a temporary palliative procedure.
References:
1. Nobuhara KK, Gorski YC, La Quaglia MP, Shamberger RC. Bronchogenic cysts and esophageal duplications: common origins and treatment. J Pediatr Surg 1997;32(10): 1408-1413.
2. Ribet ME, Copin MC, Gosselin BH. Bronchogenic cysts of the lung. Ann Thorac Surg 1996;61(6): 1636-1640.
3. Aktogu S, Yuncu G, Halilcolar H, Ermete S, Buduneli T. Bronchogenic cysts: clinicopathological presentation and treatment. Eur Respir J 1996;9(10): 2017-2021.
4. Vos CG, Hartemink KJ, Golding RP, Oosterhuis JW, Paul MA. Bronchogenic cysts in adults: frequently mistaken for a solid mass on computed tomography. Wien Klin Wochenschr. 2011 Mar;123(5-6):179-82. doi: 10.1007/s00508-011-1541-3. Epub 2011 Feb 28.
COTW handling editor: Monica Deac







