Case from: Tayeb Rahim, MS3, Clint Walters, MD, Aamisha Gupta, MD, Jayanth Keshavamurthy, MD, William B. Bates, MD, and Gyanendra Sharma, MD
Institution: Augusta University, Augusta, GA, United States
Clinical history:
A 20-year-old male with a history of hypertension presented to the emergency department because of a severe headache. On examination, the patient was confused and disoriented. His BP was 135/61 mmHg, temperature 35.6°C (97.9°F), pulse 78, and respiratory rate 24. Cardiovascular exam showed a regular heart rhythm, a grade III/VI diastolic murmur heard best in the third left intercostal space, strong pulse, no edema, warm skin, and capillary refill of < 3 seconds. No lower extremity blood pressures were obtained.
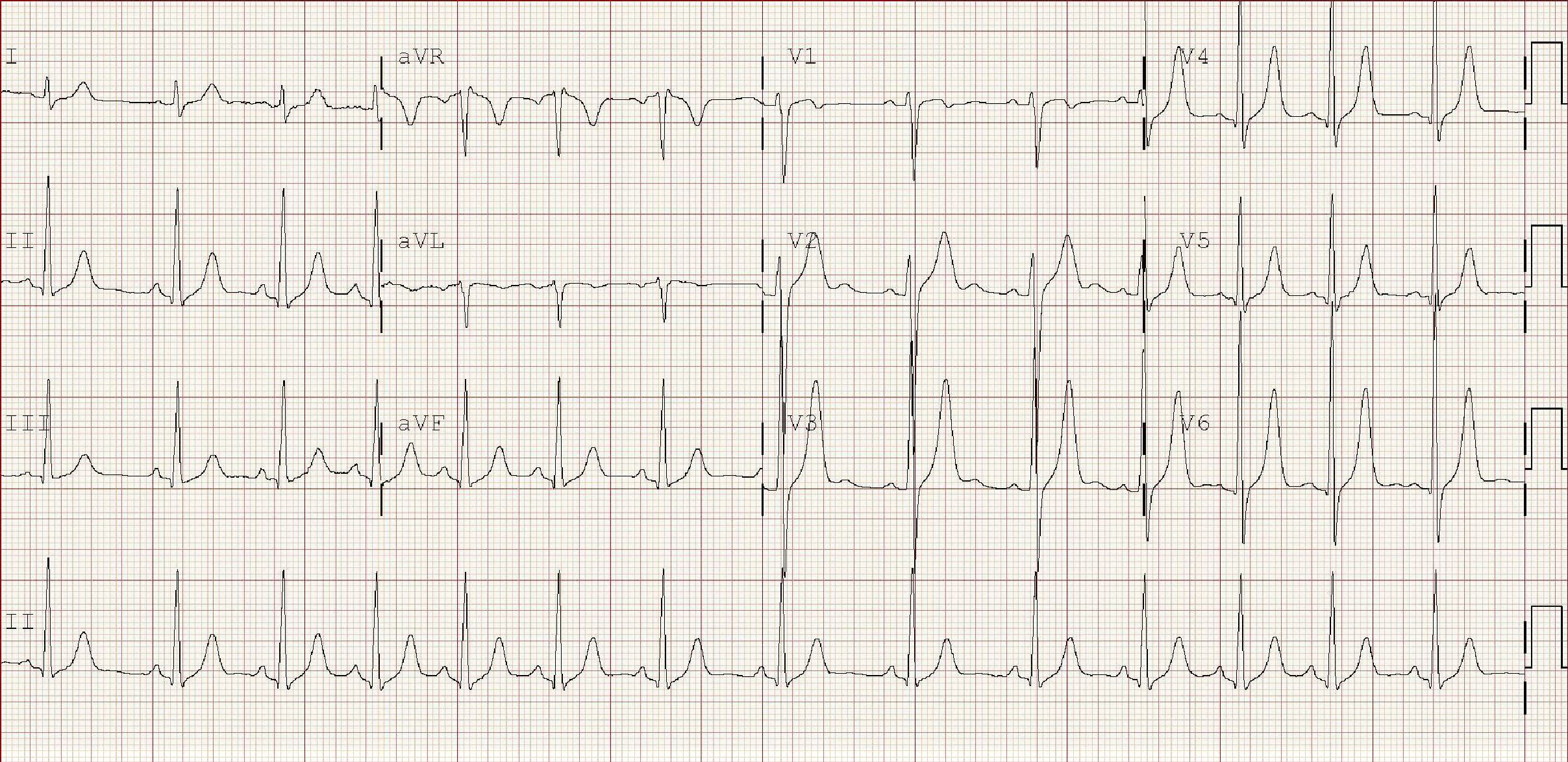
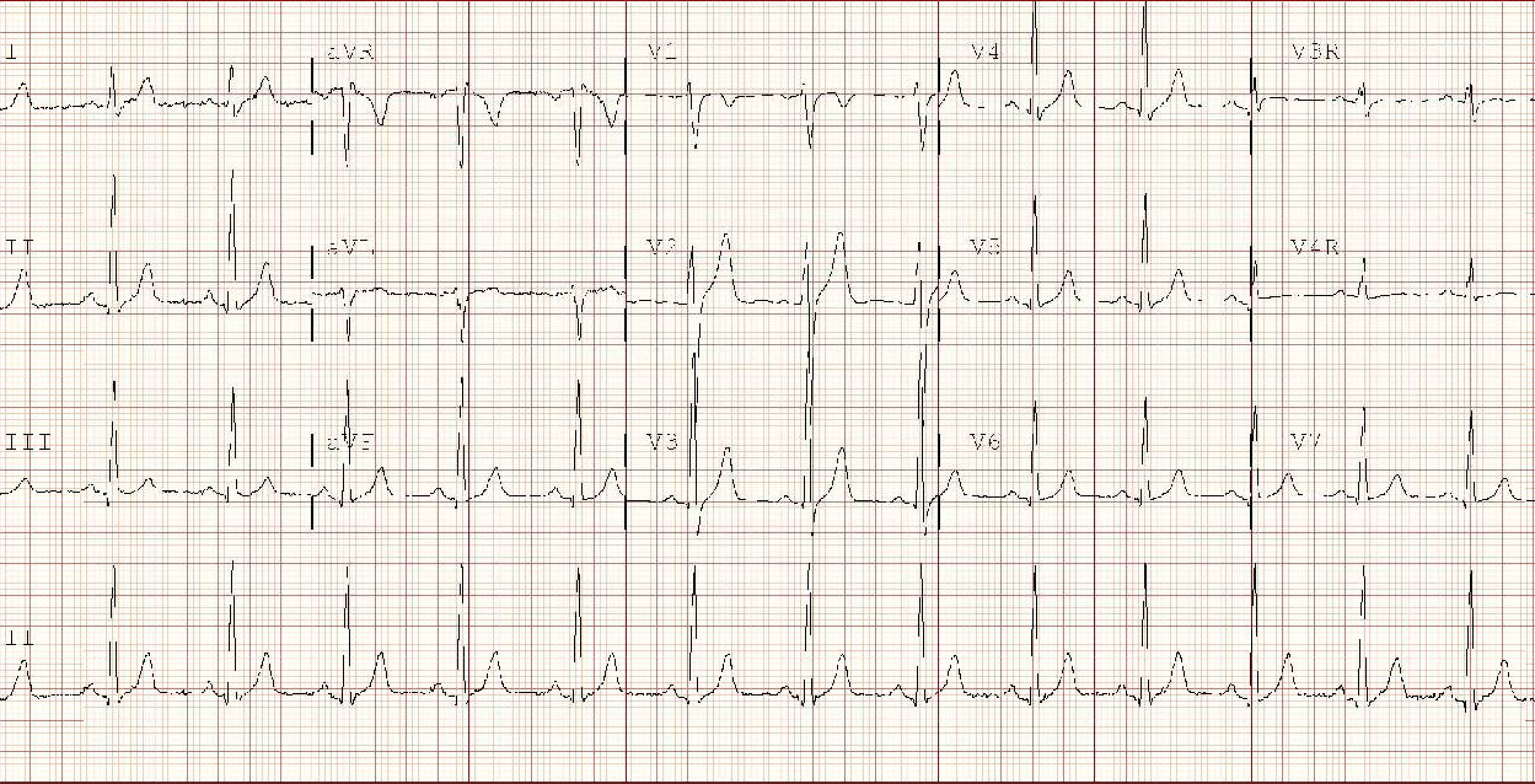
EKG suggested left ventricular hypertrophy and showed tall T-waves and ST-elevations (Figure 1).
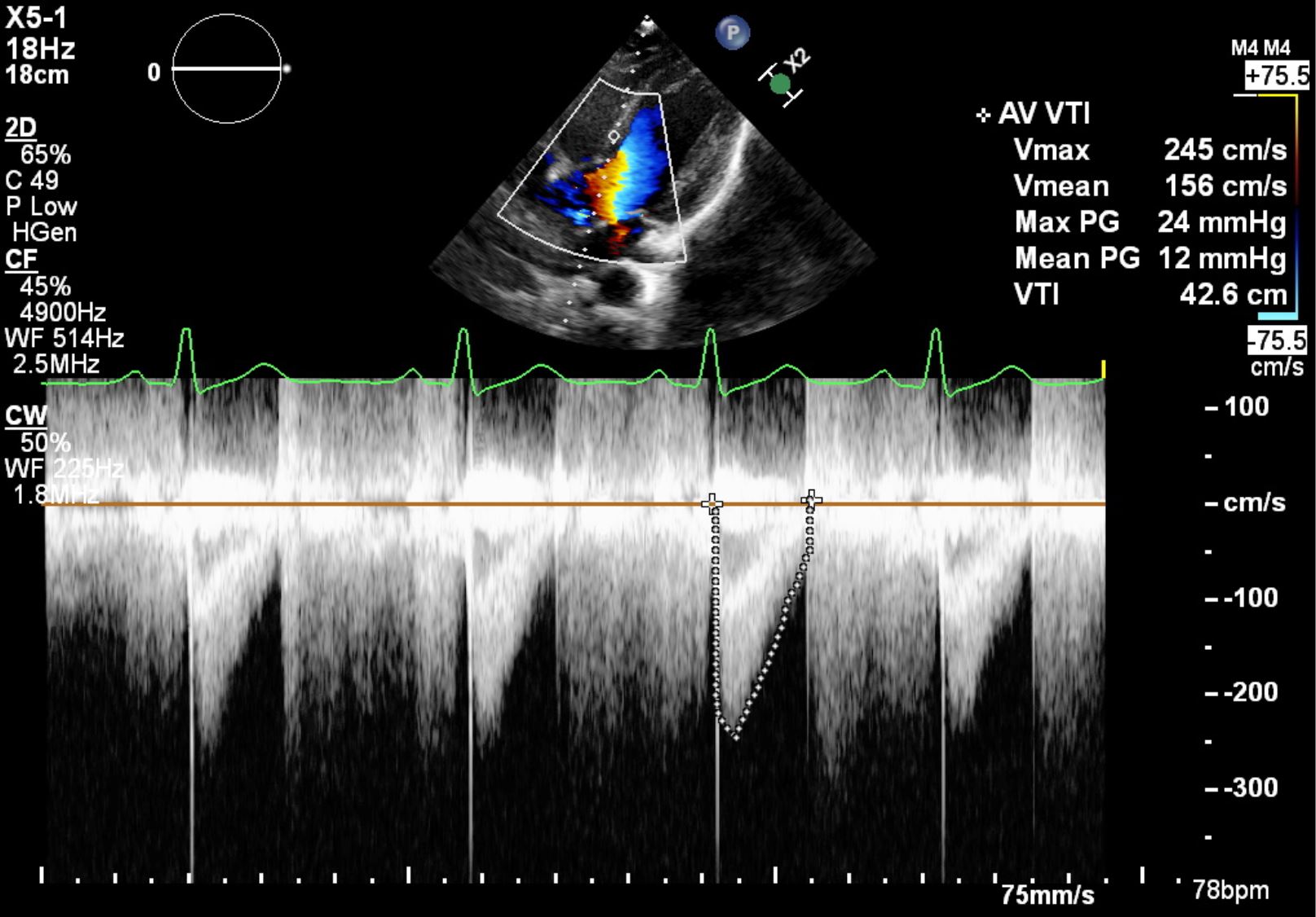
Transthoracic echocardiogram showed a bicuspid aortic valve with severe aortic regurgitation (50% regurgitant fraction) (Figure 2) and an eccentric jet directed toward the anterior mitral valve leaflet. Since aortic coarctation was not suspected no gradients in aorta were obtained.
Brain CT scan showed a subarachnoid hemorrhage due to a ruptured basilar tip aneurysm. Patient underwent coil embolization, and a right frontal ventricular drain was placed.
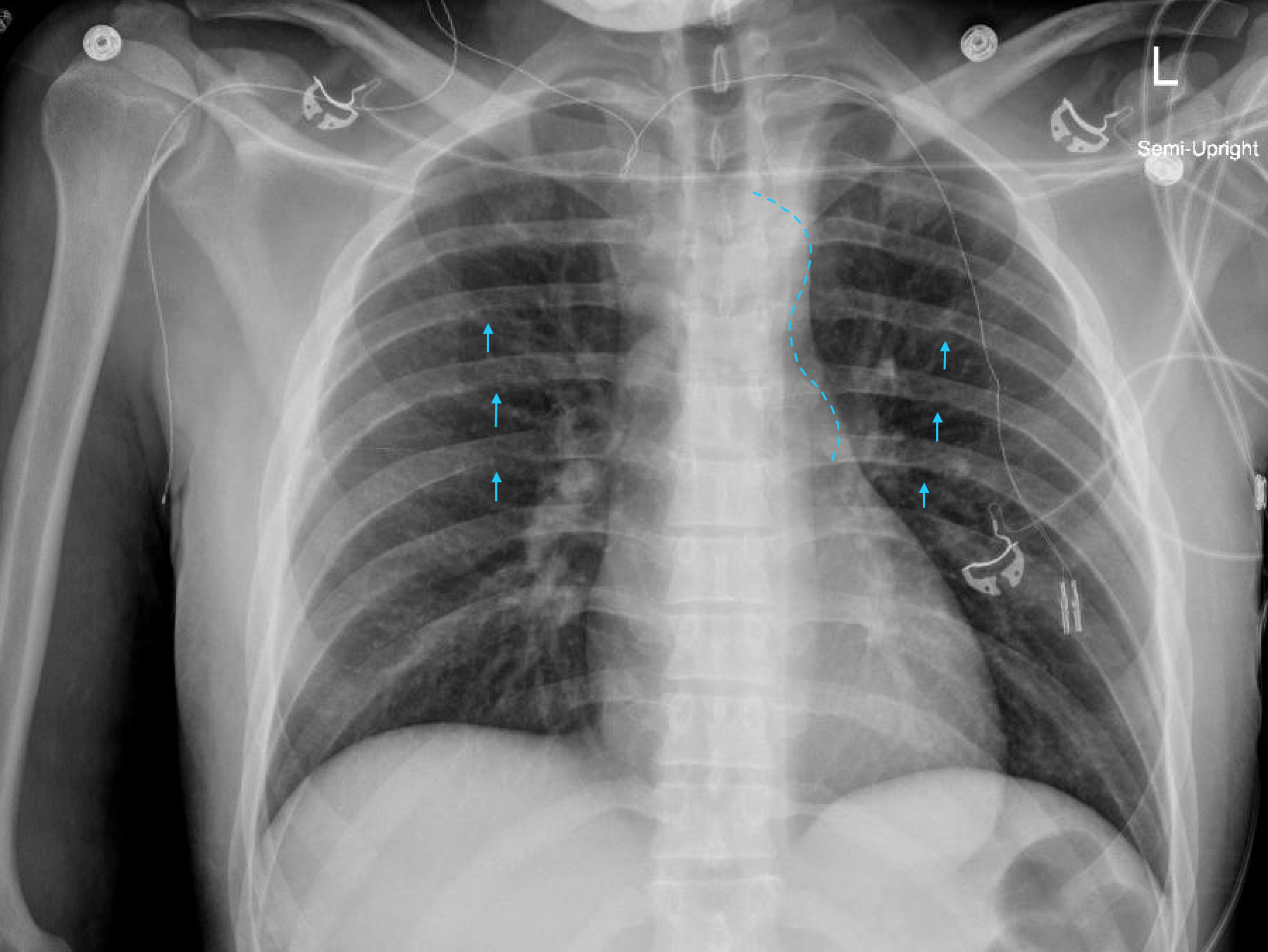
The chest x-ray showed the figure “3 sign” as well as rib notching (Figure 3).
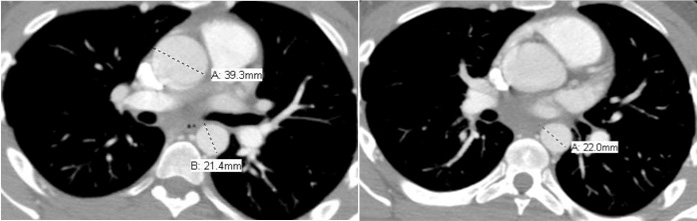
Chest CT revealed coarctation of the aorta, the narrowest portion measuring 7.9 mm in diameter at the proximal descending aorta (Figures 4 (left) and 5 (right)).
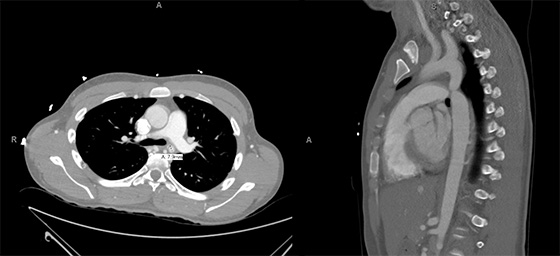
The ascending thoracic aorta measures 39 mm in diameter (Figure 6 (left)), and the descending aorta distal to the stenosis measures 22 mm in diameter (Figure 7 (right)).
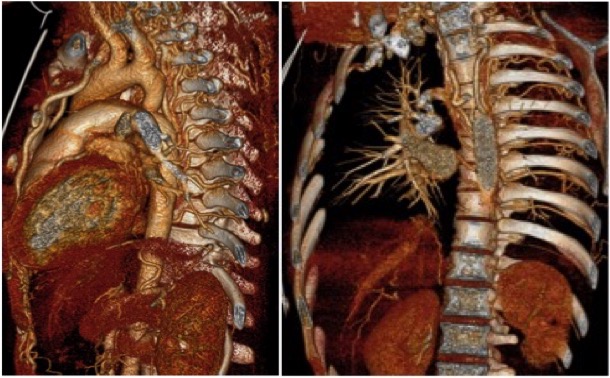
Volume-rendered images demonstrate prominent internal thoracic and intercostal arteries (Figures 8 (left) and 9 (right)).
A 3T MRI scanner was used to obtain the following results.
CE-MRA: Numerous collateral intercostal arteries associated with ribs 4 – 9. Large anastomotic collateral between the left subclavian and the T8 intercostal artery. Volume-rendered images demonstrate prominent internal thoracic and intercostal arteries along with a moderate-sized spinal artery originating immediately distal to the coarctation (Figure 10).
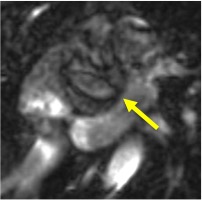
Balanced steady-state free precession imaging: The aortic valve appears like a true bicuspid valve, with fusion of the right coronary and left-coronary aortic cusps and a small rudimentary raphae (Figure 11). Normal right and left ventricular function. Normal left ventricular ejection fraction. There was no evidence of delayed myocardial enhancement to suggest a myocardial scar. The ejection fraction was 55% (borderline low), left ventricular end diastolic volume was 85.4 ml/m2 (normal), and the left ventricular end systolic volume was 38.1 ml/m2 (high). The end diastolic left ventricle wall mass was 91.5 gr/m2 (high).
Velocity-encoded cine MR imaging:There was a pressure gradient across the coarctation relative to the aortic arch that was not accurately quantified due to technical difficulties. There was moderate aortic regurgitation of 44%.
Case follow-up
The patient underwent cardiac catheterization with stent placement in the coarcted segment. Pressure measurements during catheterization were 85/40 in the ascending aorta and 65/50 in the descending aorta with a 20 mmHg peak gradient between the two.
EKG (Figure 12) and echo were performed after the procedure. Echo now demonstrates only mild to moderate aortic regurgitation.
Conclusion
Clinicians should maintain a certain degree of suspicion for coarctation of the aorta in young patients presenting with hypertension. Once clinical signs are identified, imaging can be used to diagnose aortic coarctation evaluate for other associated anatomic abnormalities that put the patient at risk for development of chronic conditions such as heart failure or acute conditions such as intracranial hemorrhage. The baseline degree of stenosis associated with the coarctation can be documented, and patients can then be appropriately managed to prevent future morbidity and mortality. MRI is very useful in such patients as it allows one to non-invasively assess the anatomic and functional integrity of the heart and great vessels, without any risk of radiation exposure. MRA can be used to visualize and measure the severity of the coarctation as well as to map out any compensatory collateral pathways that have formed. Velocity-encoded cine MR imaging allows us to measure peak flow velocities at different points along the aorta to assess the maximum gradient. We can then use these measurements to derive the pressure gradient across the coarctation. Using a fully refocused steady-state sequence, we can visualize the heart at different phases of the cycle with very little motion artifact, allowing us to identify other associated anatomic abnormalities or compromises to cardiac function. It is also a useful tool for evaluating left ventricular ejection fraction and left ventricular mass.
Perspective
The presence of hypertension in children can often be attributed to an underlying cause, such as renal parenchymal disease or coarctation of the aorta. An identifiable cause is less often found in adolescents and even less so in young adults. Common etiologies of secondary hypertension in the young adult age group include thyroid dysfunction, fibromuscular dysplasia, and renal parenchymal disease (1). If present, coarctation of the aorta is frequently discovered during childhood. It is less common for it to be left undiagnosed until adulthood.
Coarctation of the aorta may be associated with a number of other cardiac and non-cardiac findings such as bicuspid aortic valve, ventricular septal defect, or intracranial aneurysms. The clinical signs for coarctation of the aorta include the presence of a heart murmur, weak femoral pulses, and an elevated blood pressure in the upper extremities. Radiographic features of aortic coarctation may include the figure of 3 sign, rib notching, and left ventricular hypertrophy on plain film. CT and MR angiography can be used to visualize the severity of coarctation and the pattern of collateral vessels.
CMR is of particular importance in such patients as it allows assessment of anatomic and functional abnormalities including maximum gradient across the coarctation. With phase-contract velocity-encoded cine MR, peak flow velocities can be measured non-invasively in the narrowest portion of the stenosis, and the pressure gradient across the coarctation can be calculated using the modified Bernoulli equation, ΔP = 4(v22¬-v12) (2). The value obtained for the pressure gradient can be used to determine whether or not intervention is necessary to correct the coarctation. Of note, there are numerous pitfalls to this technique of calculating gradients with phase contrast MR due to interuser variability and placement of measurement planes (3). A pressure gradient during catheterization greater than 15-20 mmHg indicates a need for intervention (4). Assessing the heart for valvular abnormalities, cardiac function, and septal wall defects was accomplished using fully refocused steady-state sequencing, which is superior to other steady-state sequencing methods in that it is the least sensitive to motion artifacts and produces a high signal to noise ratio (5). Cine true FISP was used to visualize the heart at various stages of the cardiac cycle and further characterize any abnormalities.
References:
- Viera AJ, Neutze DM. Diagnosis of secondary hypertension: an age-based approach. American Family Physician. 2010;82(12);1471-1478.
- Oshinski JN et al. Improved measurement of pressure gradients in aortic coarctation by magnetic resonance imaging. Journal of the American College of Cardiology. 1996;28(7):1818-1826.
- Wetzel SG et al. Real-Time Interactive Duplex MR Measurements Application in Neurovascular Imaging. American Journal of Roentgenology. 2001;177(3): 703-707.
- Hom JJ, Ordovas K, Reddy GP. Velocity-encoded cine MR imaging in aortic coarctation: functional assessment of hemodynamic events. RadioGraphics. 2007;8(2).
- Chavhan GB, Babyn PS, Jankharia BG, Cheng HM, Shroff MM. Steady-state MR imaging sequences: physics, classification, and clinical applications. RadioGraphics. 2008;28(4).
Case prepared by Associate Editor: Lilia M. Sierra Galan, MD





