Arun Dahiya, MBBS, FRACP 1,2,3; Carly Jenkins, PhD 1; Colin Jeffries, DDM 1; Desmund Hardman, BA App Sci.1; Prasad Challa, MBBS, FRACP 1.
1. Department of Cardiology, Logan Hospital, Brisbane QLD Australia
2. Griffith University School of Medicine, Gold Coast QLD Australia
3. Royal Brisbane and Women’s Hospital, Brisbane QLD Australia
Clinical Presentation
A 57-year-old female presented with atypical chest pain. Her past medical history was unremarkable. Initial ECG (Figure 1) revealed inferolateral T wave inversion without evidence of left ventricle hypertrophy by voltage criteria; however, serial cardiac enzymes were negative.
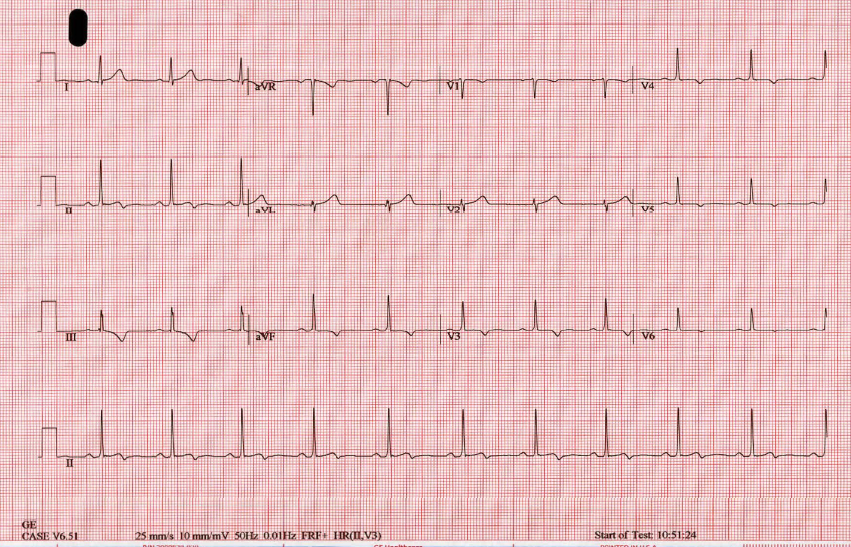
Figure 1: 12 lead EKG revealing inferolateral T wave inversion without evidence of left ventricle hypertrophy.
Acute coronary syndrome was ruled out and the patient was referred for stress echocardiography. The stress echocardiogram revealed normal LV size and systolic function with no resting or inducible regional wall motion abnormality. However there was an incidental finding of asymmetric thickening of the distal inter-ventricular septum raising suspicion for atypical hypertrophic cardiomyopathy (HCM) (Video 1,2).
Video 1: Transthoracic echocardiogram apical 4 chamber view revealing asymmetric thickening of the distal inter-ventricular septum.
Video 2: Transthoracic echocardiogram short axis view revealing asymmetric thickening of the distal inter-ventricular septum.
CMR Findings
Cardiac Magnetic Resonance Imaging (CMR) was performed for further evaluation. Cine images confirmed asymmetric thickening of the inter-ventricular septum and adjacent inferior wall with no resting regional wall motion abnormality. However, the asymmetric thickening appeared to be from a well-circumscribed intra-myocardial mass, which appeared to be hyper-intense relative to the remote myocardium (Video 3,4).
Video 3: Cine 4 chambered view revealing an asymmetric mass in the distal interventricular septum.
Video 4: Cine short axis view revealing an asymmetric mass in the distal interventricular septum.
The mass also appeared to be hyper-intense on fat suppressed T2 (Figure 2). T1 and T2 mapping images revealed elevated T1 and T2 values in the mass consistent with a vascular tumor (Figure 3). Furthermore, the mass perfused avidly on first pass perfusion imaging (video 5) and hyper-enhanced on post gadolinium delayed enhancement imaging (Figure 2).
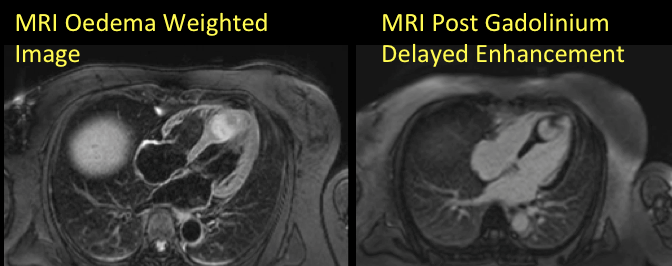
Figure 2: T2 fat suppressed image (left) and post gadolinium delayed enhancement (right)
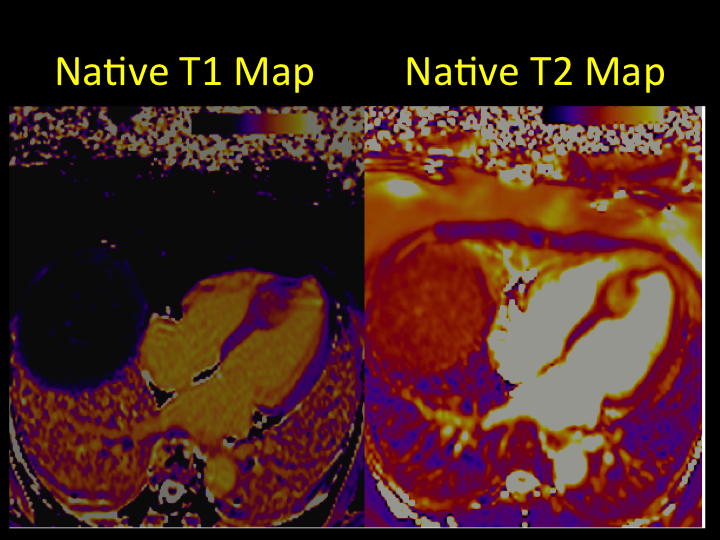
Figure 3: T1 (left) and T2 (right) mapping images
Video 5: 1st pass perfusion imaging reveals rapid uptake of contrast by the mass.
Conclusion
Overall CMR findings were most consistent with a benign, well circumscribed, intramyocardial, highly vascular mass such as haemangioma.
Subsequent computer tomography (CT) coronary angiogram ruled out significant obstructive coronary artery disease and also revealed a coronary branch vessel feeding the vascular mass and tumor blush (Figure 4).
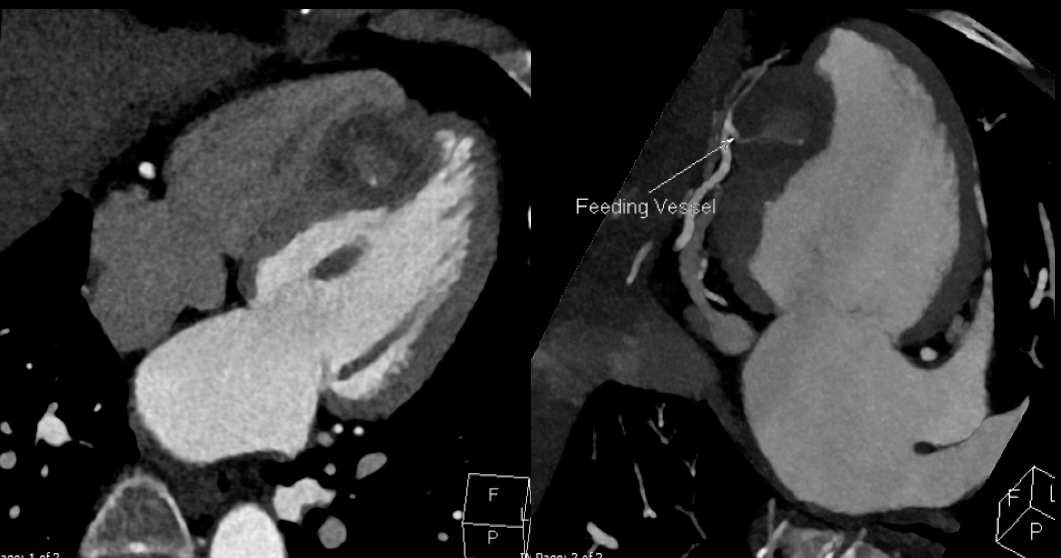
Figure 4: CT coronary angiogram
CT scans of her head, chest, abdomen and pelvis ruled out any extra-cardiac malignancy or haemangioma. The patient was managed conservatively because of her asymptomatic status and the benign appearance of the cardiac mass on CMR.
Perspective
Echocardiography raised the possibility of HCM based on the asymmetric thickening of normally contracting myocardium. However, the managing physician was astute enough to realize the limitations of echocardiography and avoided misdiagnosis of HCM by referring this patient for CMR. CMR, because of its superior special resolution and its unique ability to tissue characterize, provided further delineation and was instrumental in providing the most likely diagnosis in this case. The confidence in this diagnosis allowed the patient to avoid a surgical biopsy.
Cardiac hemangioma is a rare, benign tumor and accounts for approximately 2.8% of all primary resected heart tumors [1]. Our case likely represent capillary haemangioma, an ill-defined aggregate of closely packed, thin-walled capillaries filled with blood cells thereby accounting for avid first pass perfusion on CMR perfusion imaging.
Cardiac haemangioma can occur at any age and may be located in any cardiac chamber or involving the endocardium, myocardium or the pericardium [1]. These tumors are occasionally associated with similar tumors in the gastrointestinal tract or skin; however, this was not the case with our patient with no evidence of extra-cardiac haemangioma on CT scan evaluation. In our patient, the tumor was located in the myocardium involving distal inferior and infero-septum. The clinical symptoms vary and are mostly dependent on the location and size of the tumor. Often cardiac haemangioma are asymptomatic and discovered incidentally during cardiac surgery or on autopsy. However cardiac haemangiomas can also result in cardiac arrhythmia (which may result in sudden cardiac death), congestive cardiac failure, outflow tract obstruction and myocardial ischemia from coronary insufficiency [2]. CT Coronary angiography or invasive coronary angiogram is useful in revealing feeding vessels and tumor blush [3].
The natural history of cardiac haemangioma is unpredictable. Patients with a resectable tumor usually have a good prognosis, but prognosis of the asymptomatic patient with an unresectable tumor is unpredictable and may have a poor prognosis because of ventricular tachycardia, sudden death, or local progression [4]. The surgical outcome is generally favorable however both patient and surgeon were not keen on surgery in this patient. Therefore the strategy of close surveillance with serial imaging, Holter monitoring and exercise stress testing was preferred.
Intramyocardial haemangioma is extremely rare and can mimic HCM on echocardiography, although unlike HCM, intramyocardial haemangioma appears more hyperechogenic and well demarcated. Through this case report we highlight the advantages of complimentary multimodality imaging in non-invasive diagnoses and management of intramyocardial haemangioma.
Click here to view the entire case on CloudCMR
Case was prepared by Editor: M. Jay Campbell; Duke University
References
1. Burke A, Virmani R. Vascular tumors and tumor-like conditions. In: Atlas of tumor pathology. Tumors of the heart and great vessels. Burke A, Virmani R, editors. Washington, DC:Published by the Armed Forces Institute of Pathology; Bethesda,MD; 1996. p. 79-90.
2. Kojima S, Sumiyoshi M, Suwa S, et al. Cardiac hemangioma: a report of two cases and review of the literature. Heart Vessels 2003;18:153-6.







