Zachary Laste MD, Melissa Wein MD, Dhiraj Baruah MD, Kaushik Shahir MD, Jason Rubenstein MD
Medical College of Wisconsin, Milwaukee, Wisconsin
Clinical History
A 64-year-old male with history of Acute Myelogenous Leukemia (AML) status post bone marrow transplant (BMT) in complete remission presented with dyspnea when laying on his right side which resolved when supine or in the left lateral decubitus position. He also reported occasional shortness of breath with mild exertion. Only tachycardia was noted on clinical examination. There were no clinical signs of SVC syndrome.
An echocardiogram demonstrated no pericardial effusion or tamponade, normal left ventricular size with mild systolic dysfunction, normal right ventricle size with normal systolic function, normal bi-atrial size, and trace mitral valve regurgitation. Chest radiograms were unremarkable. CT was ordered due to new tachycardia of 145 bpm, with clinical concern for PE or other pulmonary process. The initial contrast enhanced CT (Image 1) demonstrated a filling defect within the right atrium consistent with intra-atrial thrombus or mass and MRI was recommend for further characterization.
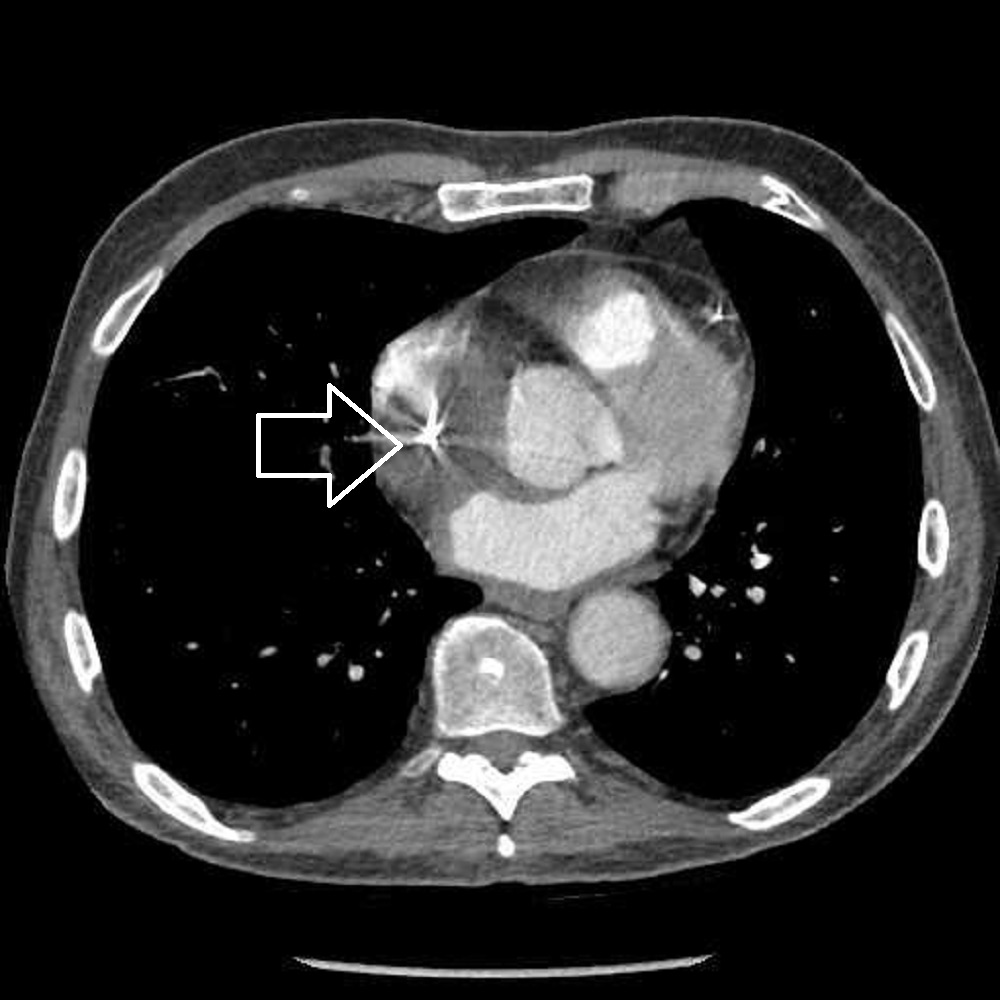
Image 1. CT chest with contrast shows a filling defect in the right atrium (white arrow).
CMR Findings
A large right atrial mass was identified extending from the superior vena cava to the inferior vena cava ostia. This mass was isointense on SSFP (Movie 1,2 and Image 2,3), intermediate signal on T1 (Image 4), and hyperintense on T2 weighted images (Image 5) with heterogenous postcontrast enhancement (Image 6) and uniform perfusion (slower than normal myocardium, Movie 3). Several small adherent laminar thrombi were noted (Image 7). The SVC was partially obstructed with narrowing down to 4 mm (peak SVC velocity was 1.3 m/s, Movie 4 and Image 8).
Movie 1, Image 2: Four chamber SSFP with an isointense mass in the right atrium (white arrow).

Movie 2 and Image 3: Short axis SSFP with an isointense mass in the right atrium (white arrow) causing narrowing of the superior vena cava.
Image 4: T1 weighted axial stiff frame with an intermediate signal right atrial mass (white arrow).
Image 5: Four chamber T2 weighted image with fat saturation with a hyperintense right atrial mass (white arrow).
Image 6. Four chamber phase sensitive inversion recovery post contrast image with null inversion time with heterogenous postcontrast enhancement in the right atrial mass (white arrow).
Movie 3. Four chamber perfusion with a right atrial mass with uniform perfusion slower than normal myocardium.
Image 7: Short axis phase sensitive inversion recovery with long inversion time with several small adherent laminar thrombi present (white arrow).
Movie 4 and Image 8: Phase contrast image of the superior vena cava en face (white arrow) with partial obstruction from the right atrial mass.
Conclusion
The mass was subsequently biopsied via intracardiac echo-guidance via right femoral approach with 9 samples taken, and the histopathology demonstrated myeloid sarcoma (Image 9). Imaging features were typical for this entity with T2 hyperintense, T1 intermediate signal. Uniform perfusion and delayed enhancement is common. Small adherent laminar thrombi are also frequently noted, as in this case. These imaging characteristics are non-specific, however, and diagnosis is reliant on histopathology, clinical history, and/or time course of the lesion. The patient underwent multiple rounds of chemoradiation with initial treatment response. However, disease progression followed with eventual multi-organ failure and death.
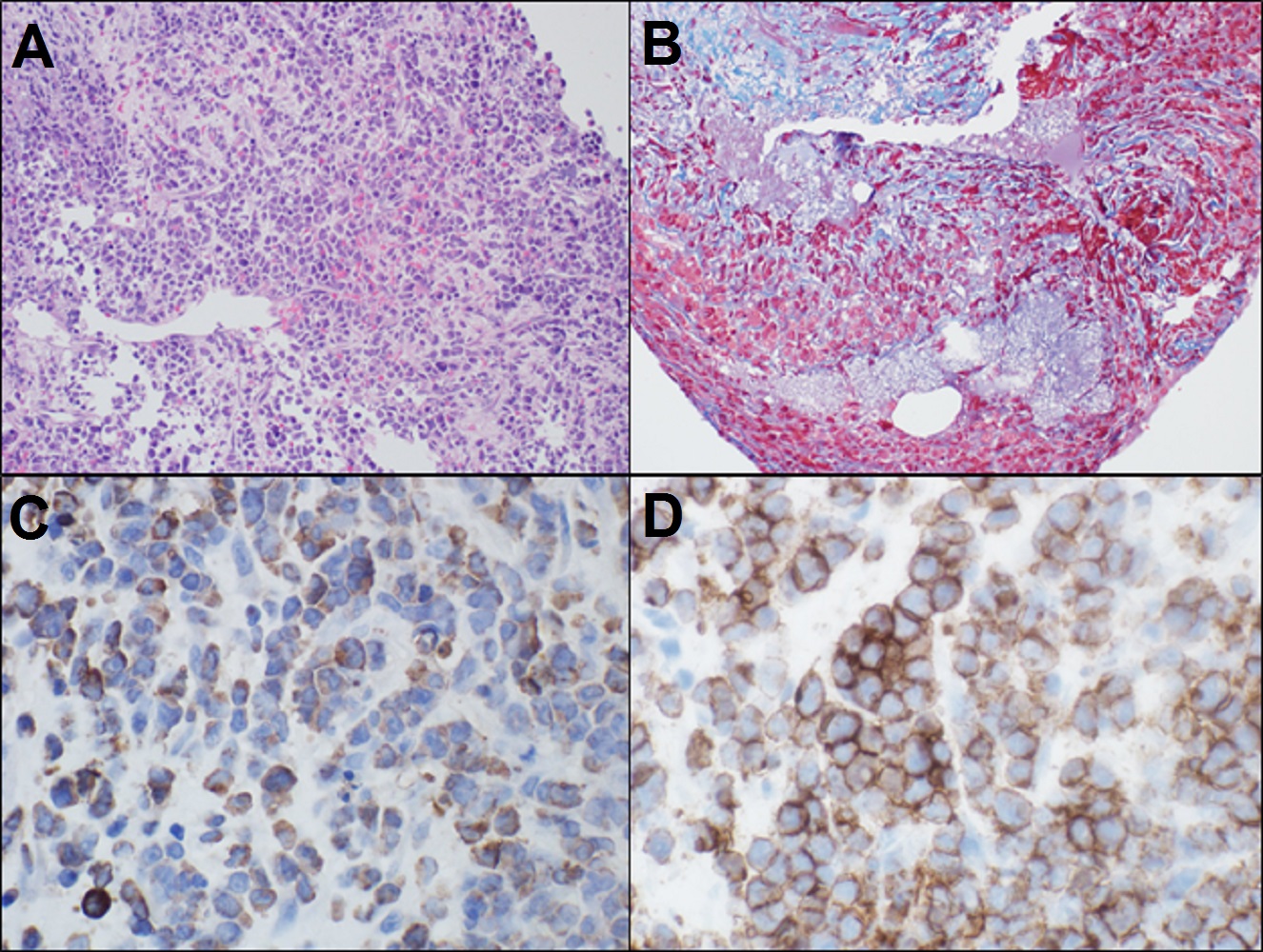
Image 9. Photomicrographs at medium and high power of the right atrial mass. Sections show cardiac muscle fibers with extensive fibrosis and an atypical infiltrate of small round blue cells with scant cytoplasm (A). The cells display a monotonous pattern, composed of large cells with irregular nuclear contours, immature chromatin, prominent eosinophilic nucleoli, and a moderate amount of variably granulated, eosinophilic cytoplasm. Mitoses can easily be identified. A trichrome stain (B) shows increased collagen associated with the neoplastic infiltrate. There is extensive necrosis. The blasts shows positivity in a subset for myeloperoxidase (C) and are positive for CD117 (D).
Perspective
Myeloid sarcoma is also known as chloroma or granulocytic sarcoma. They are solid tumors composed of immature WBCs (myeloblasts), and represent an extramedullary manifestation of AML. This is more commonly seen in patients less than 15 years old. Almost any tissue can be affected, with CNS, thyroid, lacrimal/salivary glands, and paranasal sinuses having been reported.
“Chloros” is an ancient Greek word for green. Chloromas usually present as reddish-blue (not green) thickenings in the skin. Compressing the skin lesions displaces blood and reveals a green color for a few seconds. The green coloration is attributed to the presence of myeloperoxidase which is produced in over 70% of lesions.
Myeloid sarcoma often presents with multifocal sites of disease. This patient also had involvement of the right globe and base of tongue. Both lesions were treated with radiation therapy and responded well. The cardiac involvement was less responsive to treatment.
Patients often experience palpitations, fatigue, and shortness of breath. High grade obstruction of the SVC flow can lead to SVC syndrome with venous distension and swelling of the neck, chest, and upper extremities, that was not present in this case. Other symptoms include headaches, lightheadedness, and difficulty breathing. High grade IVC obstruction can lead to swelling of the lower extremities and ascites.
Click here to view case on CloudCMR
References
Case Prepared by:
Jason Johnson MD MHS
Associate Editor, SCMR Case of the Week
LeBonheur Children’s Hospital
University of Tennessee Health Science Center





