Madhusudan Ganigara MD, Arushi Dhar MD, Nilanjana Misra MD
Division of Pediatric Cardiology, Cohen Children’s Medical Center of New York – Hofstra Northwell School of Medicine, New York.
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Click here for PubMed Reference to Cite this Case
Clinical History
A 30 year old gravida 2 para 1 female was referred for evaluation of a fetal intracardiac mass noted on routine obstetric ultrasound. Fetal echocardiogram at 26-weeks’ gestation revealed a single, large, homogenous, hyperechoic cardiac mass occupying bi-atrial cavities with unobstructed intra-cardiac flows. There was normal biventricular systolic function and no pericardial effusion. Serial fetal echocardiograms showed the size of the mass increasing in proportion to the rest of the cardiac size.

Postnatally, the infant was clinically well. Transthoracic echocardiogram confirmed a large mass measuring 11 x 13 mm, arising from the Eustachian valve and predominantly occupying the right atrial cavity, with unobstructed intra-cardiac flows. There was a patent foramen ovale with left to right shunt.
Low dose Aspirin was started for thromboprophylaxis. Tuberous sclerosis work-up including a brain MRI, renal ultrasound and genetic testing were negative. Patient was discharged home with plan for outpatient cardiac MRI. The infant continued to thrive well with no complications related to the mass.
CMR Findings
A cardiac MRI was performed to characterize the tumor. In view of patient age, the procedure was performed under general anesthesia with breath-holding. On cine SSFP sequences, there was an irregular dumbbell-shaped mass attached to the Eustachian valve on the right side of the atrial septum measuring 5×11 cm (axial plane) and 8 x 12 mm (sagittal plane). There was no obstruction to intracardiac flows.
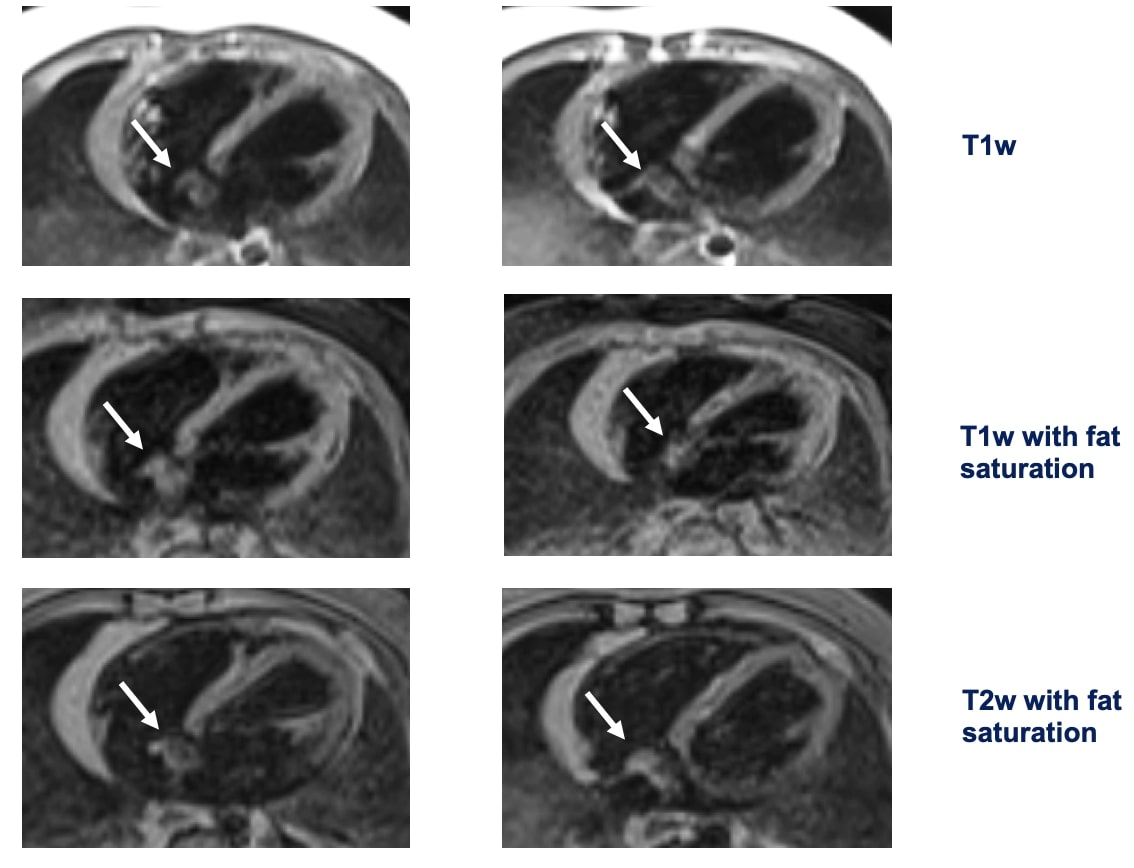
The mass was isointense on T1w sequences with and without fat saturation, suggesting a non-fatty mass. On T2w sequence with fat suppression the mass was non-homogenously hyperintense.
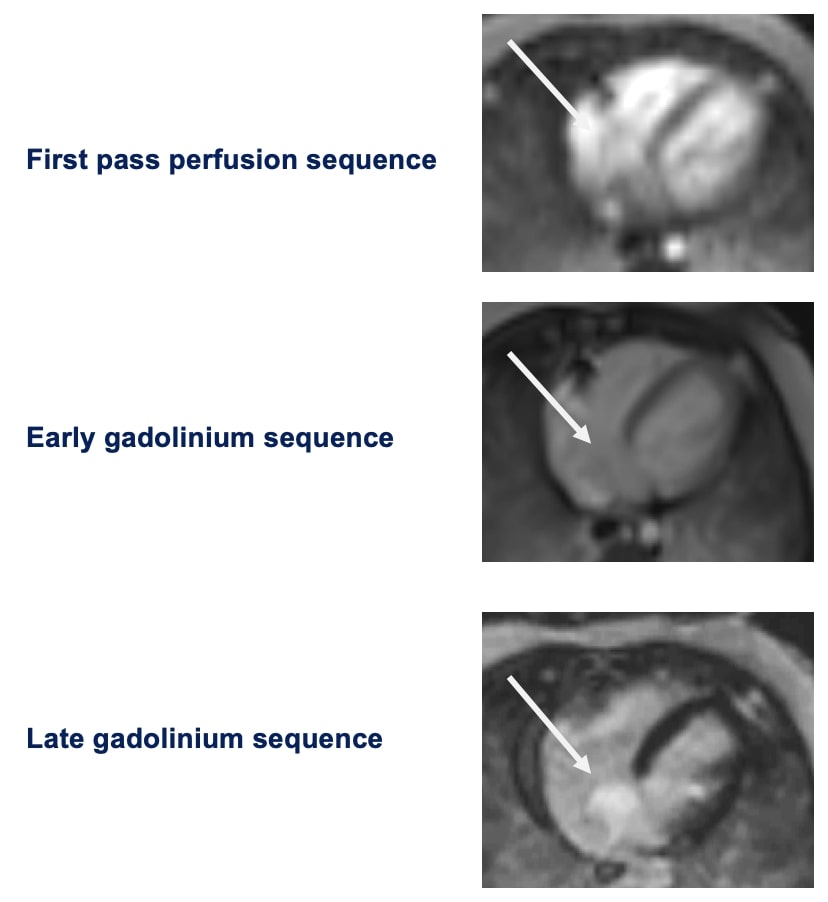
There was early uptake of contrast to the center of the mass on first pass perfusion suggesting a vascular tumor.
The mass was not visualized on early gadolinium sequences (TI 600ms) while there was intense enhancement on delayed gadolinium enhancement imaging.
Conclusion
In view of the patient’s age, tumor location, and clinical presentation, a benign hemangioma was considered the most likely diagnosis based upon the current CMR knowledge (see table below). [1] With a mass that was not growing in size and no clinical complications in the form of arrhythmia, heart failure or obstruction, there was no indication to obtain a tissue diagnosis. The infant was conservatively managed with low dose Aspirin and was closely monitored with serial echocardiograms that revealed decreasing tumor size.

Table key: − = iso- or hypointense; +/- = variable intensity; + = hyperintense; Fat sat = fat saturation; FPP = first pass myocardial perfusion; MDE = myocardial delayed enhancement; SSFP = steady state free precession.
Perspective
Imaging sequences currently available by cardiac MRI do not allow distinction among benign vascular tumors (e.g., hemangioma), malignant vascular tumors (e.g., angiosarcoma), vascular malformations, and tumors with ample vascular supply (e.g., paraganglioma). Primary vascular cardiac tumors such as hemangiomas are extremely rare (<10% of all primary cardiac tumors in children). Congenital cardiac hemangiomas can present as fetal arrhythmia, hydrops fetalis and intrauterine fetal demise. Neonates can be asymptomatic, but can also present with cardiac tamponade, arrhythmias, congestive heart failure or sudden death. [2]
Asymptomatic children are best managed conservatively by closely monitoring for development of complications. The role of medical therapy is limited; there is no proven role for beta blockers, while steroids have mixed results. Surgery is only offered for rapidly growing or symptomatic tumors and, steroid therapy is reserved for patients with unresectable tumors. [3] The present case highlights the role of cardiac MRI in non-invasive diagnosis of vascular cardiac tumors by a combination of imaging sequences for tissue characterization. [4]
Please click here to view the case on CloudCMR.
References
Case Prepared by:
Madhusudan Ganigara, MD
Associate Editor SCMR Case of the Week.
Cohen Children’s Medical Center of New York, Hofstra-Northwell School of Medicine.







