Jason G. Mandell, MD, MS; Adam Christopher, MD; Laura J. Olivieri, MD; Yue-Hin Loke, MD
Division of cardiology, Children’s National Hospital, Washington, DC, USA.
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Click here for PubMed Reference to Cite this Case
Clinical history
A 15 year old asymptomatic girl was followed by cardiology for a small perimembranous ventricular septal defect (VSD). A routine echocardiogram demonstrated spontaneous closure of the VSD, as well as right atrial and ventricular enlargement. Significant volume loading from a VSD would cause left heart dilation which was not seen. The unexpected right heart dilation suggested a previously unnoticed atrial level shunt. She was referred for surgical closure of a presumed secundum atrial septal defect (ASD). However, on review of imaging prior to surgery, an enlarged coronary sinus was noted.
A pre-operative echocardiogram confirmed the atrial shunt and dilated coronary sinus with mild dilation of the right atrium, right ventricle, and pulmonary arteries. Additionally, the small perimembranous ventricular septal defect was closed by tricuspid valve tissue. There was no left superior vena cava (LSVC) seen on this study. The pulmonary venous return could not be confirmed by echocardiogram.
Figure 1: Transthoracic echocardiogram: 1) Subcostal coronal sweep showed a significant left to right atrial shunt at the inferior, posterior septum. 2) Apical view demonstrated a dilated coronary sinus.
CMR findings
Based on the concern for a dilated coronary sinus and inadequate confirmation of normal pulmonary venous return, a cardiac MRI was performed on a 1.5 T Siemens Aera (Siemens Healthcare, Erlangen, Germany). Cine imaging was technically limited by respiratory and metal artifact, but suggested a communication from the left atrium into the proximal coronary sinus with left to right shunt into the right atrium, consistent with a large unroofed coronary sinus. The metal artifact appeared to originate from a cranial source, likely from the patient’s dental braces. This artifact is typically accounted for with shimming. In this challenging case, the artifact was more pronounced, potentially as a result of her movement. Both the right atrium and right ventricle were qualitatively enlarged. A short axis stack was not performed as the study was done to delineate the atrial shunt and venous anatomy the day prior to surgery. On an axial cine stack, the right ventricular end-diastolic volume was severely enlarged at approximately 160 ml/m2 (z-score 5.2). However, as this was a free-breath sequence with significant artifact, the value was not reported. 4D flow imaging following contrast administration using Siemens WIP 785A (Venc 200 cm/sec) clearly demonstrated the shunt pathway from the left atrium into the coronary sinus and the right atrium. There was normal pulmonary venous drainage and no LSVC. The pulmonary to systemic flow ratio was calculated to be greater than 2:1 by 4D flow.
Figure 2: CMR Axial cine SSFP demonstrated a likely unroofed coronary sinus.
Figure 3: 2 chamber cine SSFP demonstrated a communication between the enlarged coronary sinus and the left atrium.
Figure 4: 4D flow imaging: Transverse (top right), left anterior oblique (top left), and sagittal (bottom left) views of the atrial level shunt which demonstrated flow from the left atrium into the enlarged coronary sinus and then into the right atrium through the os of the coronary sinus. A 3D rendering (bottom right) more clearly visualized the normal pulmonary venous return to the left atrium and the significant left to right shunt.
Figure 5: 4D flow imaging: A 3D rendering in a 4 chamber view showed the substantial flow from the left atrium across the inferior atrial septum into the right atrium.
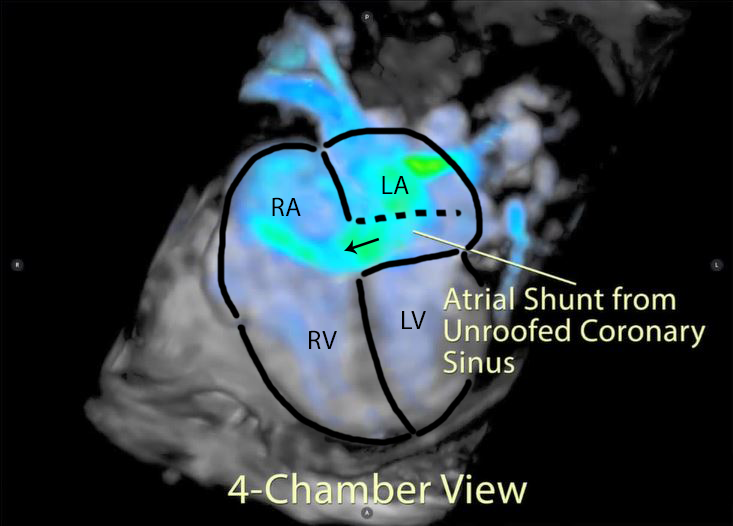
Figure 6: A labeled still-frame of the above outlining the right (RA) and left (LA) atria, and right (RV) and left (LV) ventricles. The location of the unroofed coronary sinus is shown as a dotted line with an arrow demonstrating the direction of the shunt flow near the os of the coronary sinus.
Conclusion
Transthoracic echocardiography demonstrated evidence of a left to right shunt and a dilated coronary sinus. The differential diagnosis included a coronary sinus atrial septal defect, LSVC to the coronary sinus, and anomalous pulmonary veins to the coronary sinus. CMR cine stacks demonstrated no LSVC, normal pulmonary venous drainage, and a likely unroofed coronary sinus, suggesting the diagnosis of a coronary sinus atrial septal defect. The 4D flow imaging clearly visualized the atrial shunt and normal pulmonary venous return. The CMR findings allowed for appropriate surgical planning and counseling. The intraoperative transesophageal echocardiogram confirmed the intracardiac anatomy. The surgeon noted that the coronary sinus was almost completely unroofed and repaired the defect with a pericardial patch over the mouth of the coronary sinus. The post-operative transesophageal echocardiogram demonstrated no residual shunt and normal systolic function. The patient recovered quickly and was discharged home on post-operative day 2.
Figure 7: Intraoperative transesophageal echocardiogram: A pre-operative, mid-esophageal view of the atrial septum demonstrated the large coronary sinus atrial septal defect and left to right shunt.
Figure 8: Post-operative, mid-esophageal view showed the patch over the os of the coronary sinus. It was placed deeper into the os to avoid damage to the conduction system.
Perspective
ASDs are relatively common, with a reported prevalence of 1 to 2 per 1000 live births, accounting for 10 to 15 percent of congenital heart disease1. However, coronary sinus type ASDs are much less frequent. From an anatomical standpoint, coronary sinus type ASDs are a misnomer; while their physiology is consistent with an ASD, there is no true deficiency of the atrial septum. Instead, there is a defect in the common wall between the coronary sinus and the left atrium which can vary from a few millimeters to complete absence of the wall of the coronary sinus. The usual method of repair is to place an autologous pericardial patch over the mouth of the coronary sinus. This results in a trivial right to left shunt due to coronary venous return entering the left atrium2. In cases of a coronary sinus ASD, it is common to have an associated LSVC entering the coronary sinus3. If the ostium of the coronary sinus is then closed, there would be a more significant right to left shunt leading to cyanosis and an alternative surgical approach is needed.
Diagnosis of coronary sinus type ASDs is challenging and often missed by echocardiography4. Additionally, a complete evaluation of systemic and venous anatomy is necessary for appropriate surgical planning and can be difficult to prove by echocardiography5. Transesophageal echocardiography can show excellent visualization of the atrial septum, though extracardiac anatomy can be difficult to see and it is an invasive test. CMR can demonstrate rare intracardiac defects such as coronary sinus ASDs and quantify the hemodynamic effect of the shunt. To our knowledge, this is the first reported case of a coronary sinus atrial septal defect visualized with 4D flow MRI. 4D flow was able to clearly visualize the location of the shunt in the wall of the coronary sinus and demonstrate normal systemic and pulmonary venous drainage. 4D flow has the potential to significantly increase diagnostic utility of detecting atrial shunts by CMR.
Please click here to view the case on CloudCMR.
References:
3. Allen HD, Shaddy RE, Penny DJ, Feltes TF, Cetta F. (2016). Moss and Adams heart disease in infants, children, and adolescents: including the fetus and young adult (9th ed., Vol. 1). Philadelphia: Wolters Kluwer.
Case Prepared by:
Madhusudan Ganigara, MD
Associate Editor SCMR Case of the Week.
Cohen Children’s Medical Center of New York, Hofstra-Northwell School of Medicine.





