Marc Lee MD, Jason Williams MD, Simon Lee MD
Nationwide Children’s Hospital, Columbus, OH
Clinical History
An 8-year-old healthy male with a past medical history of mild persistent asthma, unvaccinated against coronavirus disease 2019 (COVID-19), was admitted with abdominal pain, emesis, and bilateral hip and thigh pain. He was diagnosed with acute COVID-19 by initial rapid molecular test which was subsequently confirmed by PCR testing with negative antibody testing. He had no preceding fevers. Exam was notable for poor peripheral perfusion. Initial inflammatory markers were normal, and an ECG demonstrated low voltages (Image 1). He required fluid resuscitation both in the emergency department and pediatric intensive care unit but eventually required inotropic support with epinephrine and milrinone. Chest computed tomography showed extensive bilateral lung opacities and atelectasis, consistent with COVID pneumonia (Image 2). Cardiac workup showed elevated troponin (ref <0.029 ng/mL) and BNP (ref <60 pg/mL), with a peak of 2.47 ng/mL and 2,379 pg/mL, respectively. Initial transthoracic echocardiogram showed severe left ventricular systolic dysfunction (LVEF 31%) without left ventricular dilation (LVEDD 3.57 cm, z-score -1.8) with a moderate-sized pericardial effusion (Movie 1). The effusion was globally distributed with a maximum dimension of 1 cm from subcostal imaging.
He was treated with intravenous immunoglobulin, remdesivir, and methylprednisolone. Due to increased air hunger, emesis, and aspiration, he suffered an in-hospital cardiac arrest requiring chest compressions with return of spontaneous circulation. For tenuous hemodynamics and persistent hypoxia, he was ultimately placed on venovenous extracorporeal membrane oxygenation (ECMO) support on hospital day (HD) 5 with concomitant percutaneous drainage of the pericardial effusion. He was decannulated on HD 8 without incident, transferred to the ward on HD 11, and discharged home in stable condition on HD 16. His troponin and BNP levels peaked while on ECMO support, then trended down and normalized prior to discharge. Cardiac MRI was performed within 2 weeks of discharge, but 7 weeks from onset of symptoms.
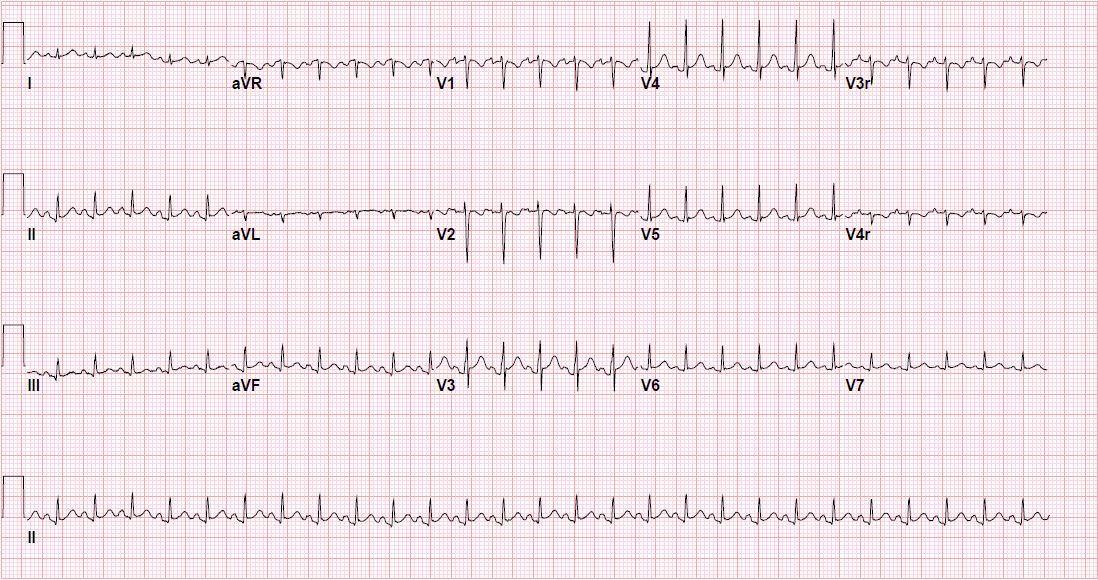
Image 1. Admission ECG showing sinus tachycardia with diffuse low voltages.
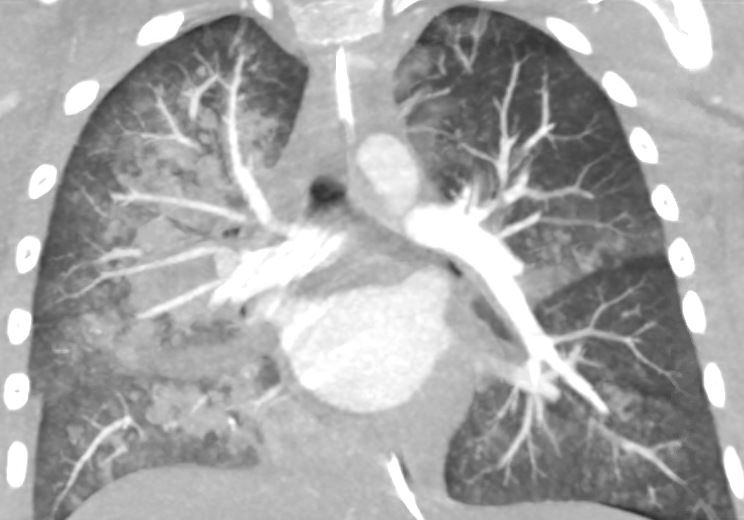
Image 2. Chest computed tomography, coronal plane demonstrating extensive bilateral lung opacities and atelectasis.
Movie 1: Echocardiogram demonstrates severe LV systolic dysfunction and moderate pericardial effusion.
CMR Findings
CMR was performed at 3T without sedation to evaluate cardiac function and for tissue characterization. There was normal bi-ventricular size and systolic function (LVEDV 72 mL (LVEDV/BSA 72 mL/m2) with an LVEF of 61%, RVEDV 81 mL (RVEDV/BSA 81 mL/m2)) without significant residual pericardial effusion (Movie 2-3). T2-weighted imaging showed increased signal intensity in the mid-LV inferior wall, extensive pericardial late gadolinium enhancement (LGE), and elevated extracellular volume fraction (ECV) (Images 3-8). Findings were consistent with myopericarditis.
Movie 2: Two-chamber cine demonstrates normal LV size and function without significant mitral regurgitation. Cine images were obtained free-breathing.
Movie 3: Four-chamber cine demonstrates normal biventricular size and systolic function. There was no significant residual pericardial effusion.
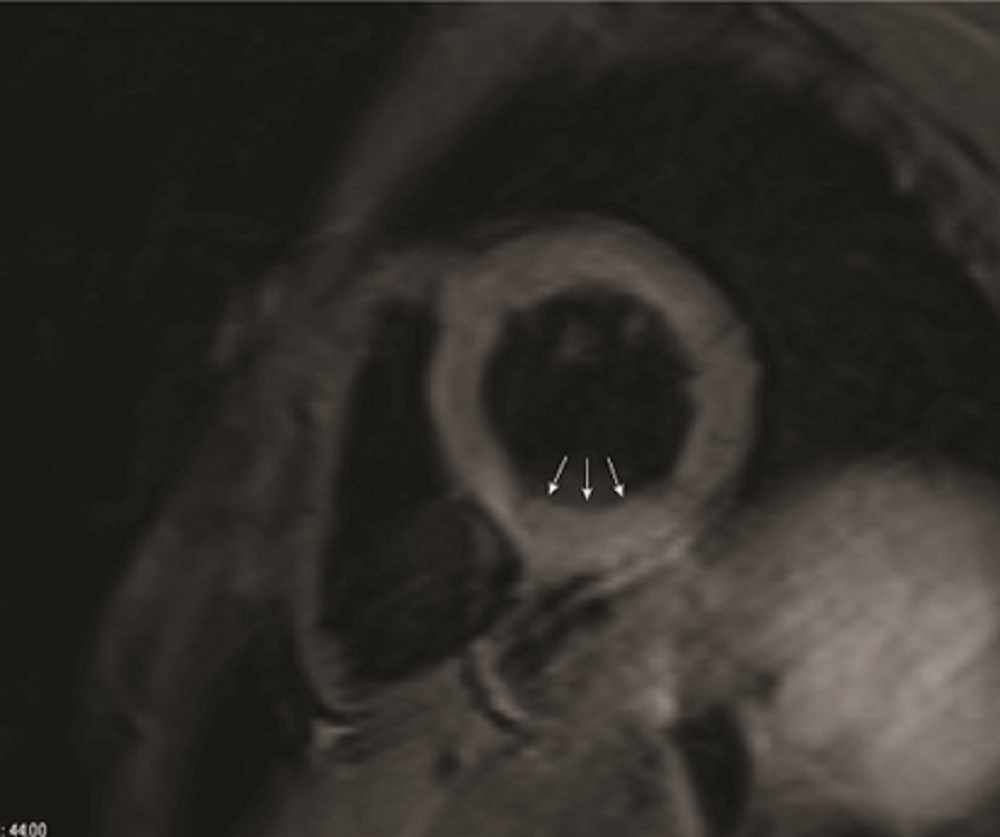
Image 3: T2-weighted triple inversion recovery sequence shows increased signal intensity in the inferior wall of the mid-LV (arrows).

Image 4: On delayed myocardial enhancement imaging in short axis, there is enhancement/LGE of the pericardium (arrows) consistent with pericarditis.

Image 5: Delayed myocardial enhancement 4 chamber with pericardial enhancement is also evident (arrows).
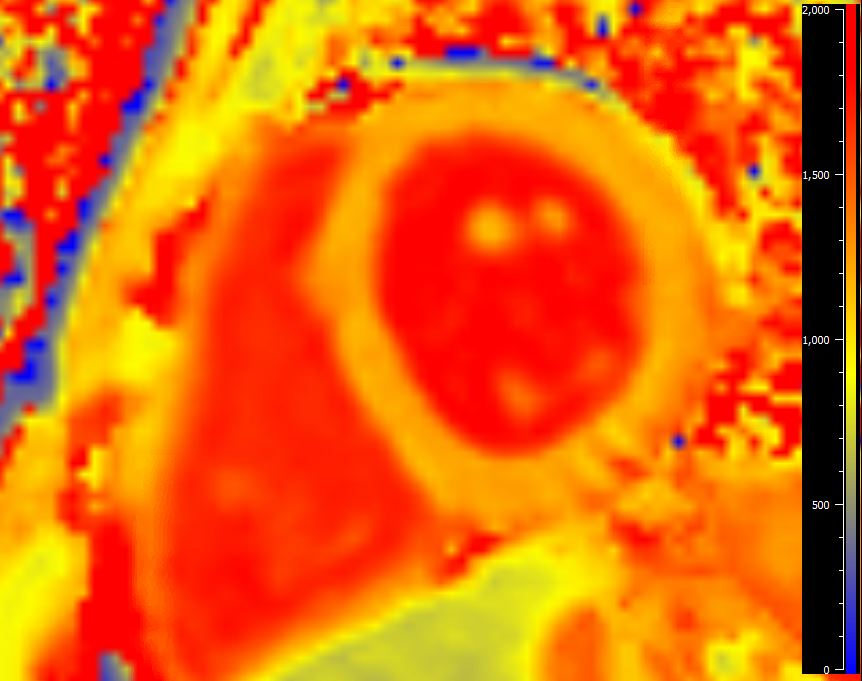
Image 6. Native T1 mapping at basal slice. Global native T1 value of 1210 ms (institutional normal < 1270 ms).
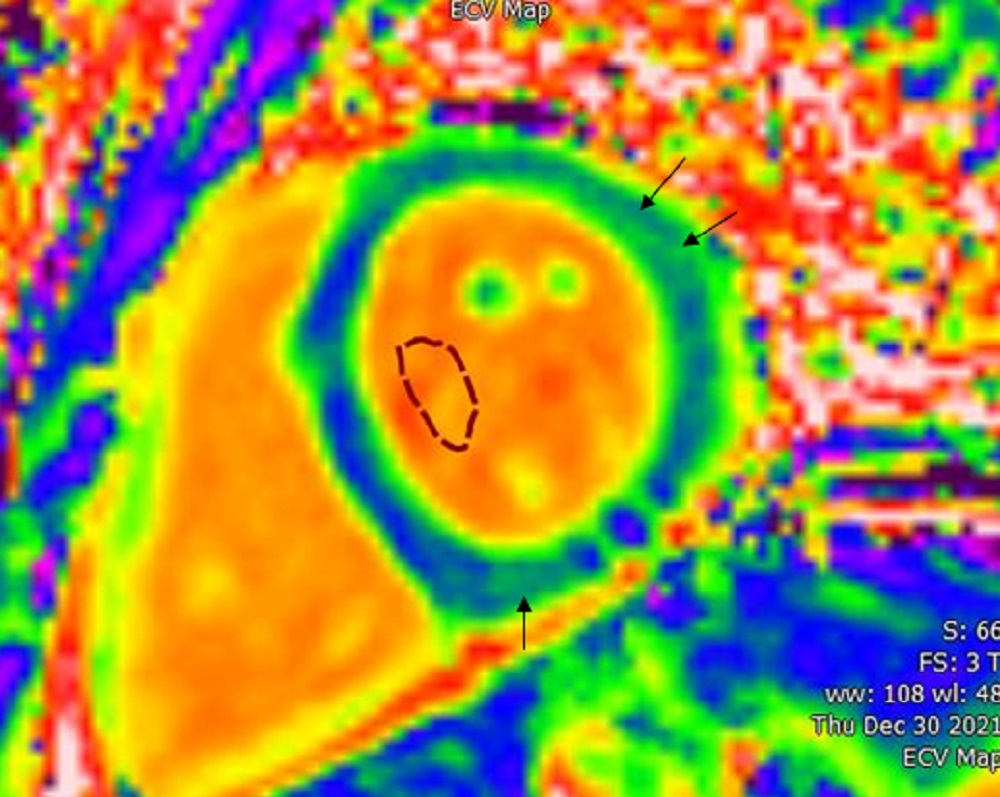
Image 7: On ECV mapping, increased global ECV fraction of 32.7% (institutional normal < 29%) with patchy areas of further hyperintensity is seen at the mid-inferoseptal (33.9%) and lateral wall (34.8%, arrows). With the patient’s clinical context, this was interpreted to represent residual myocardial inflammation/edema.
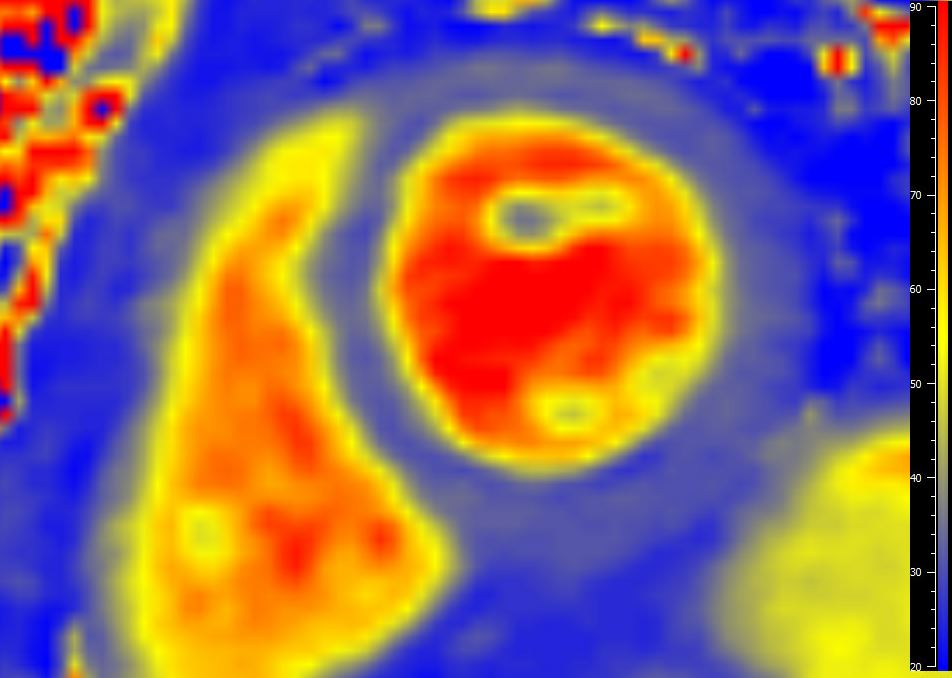
Image 8: T2 mapping at basal slice. Global T2 value 33 ms (institutional normal < 39 ms). The basal slice for T2 mapping was below the area of hyperintensity seen on T2-STIR, which covers the entire LV.

Movie 4. Strain ENCoded (SENC) imaging of the 4-chamber view measuring circumferential strain. The patient’s LV global longitudinal (LVGLS) and circumferential strain (LVGCS) were -18.3% and -19%, respectively (institutional control data with normal values of LVGLS < -17% and LVGCS < -18%).
Conclusion
Clinical course was consistent with COVID-19 pneumonia with fulminant myopericarditis. CMR findings were consistent with pericarditis with evidence of residual myocardial inflammation/edema, but otherwise recovered cardiac function. Positive prognostic indicators were the paucity of delayed myocardial enhancement and normal strain values in the setting of normal LVEF. This case highlights the tumultuous course and cardiac involvement that can be seen, even in pediatric patients with severe COVID-19 illness, the recovery of cardiac function that can be seen during the convalescent phase of illness, and the spectrum of CMR findings in pediatric patients including pericardial involvement and myocardial inflammation/edema.
Perspective
One of the key findings is that acute COVID-19 can result in critical illness, even in children. Our 8-year-old patient unfortunately had fulminant myopericarditis with COVID-19, without evidence of Multisystem Inflammatory Syndrome in Children (MIS-C). CMR has two important roles in the management of this patient. First, results of parametric mapping, LGE imaging, and strain imaging have all been shown to be strong prognostic indicators in myocarditis (1). Second, there is a clear association between mRNA vaccination against SARS-CoV-2 and the rare complication of myocarditis/pericarditis, particularly in young males (2). Current United States Centers for Disease Control and Prevention recommendations state that mRNA vaccination should be deferred until the episode of myocarditis or pericarditis has completely resolved (3). Given the excellent tissue characterization offered by CMR, even in young children, a follow-up CMR to ensure resolution of active myocardial and pericardial inflammation, particularly in this case with significant myocardial and pericardial abnormalities, may be prudent prior to vaccination.
Our patient met the diagnostic criteria for fulminant myocarditis based on the history of acute illness (presentation with COVID pneumonia, negative SARS-CoV-2 antibodies) and cardiogenic shock requiring inotropic support (4). While long-term outcome after survival from fulminant myocarditis is favorable in adults, these findings may not be applicable to pediatric patients (5). After recovery and discharge from the hospital, the patient’s CMR demonstrated normalization of ventricular function (Movies 2-3) and no myocardial delayed enhancement (Images 4-5). However, he was noted to have residual myocardial edema (Image 3) and ECV elevation (Image 7) 7 weeks from the onset of his symptoms. This may represent lingering subacute myocarditis, with the ECV elevation representing myocardial hyperemia/inflammation, especially in the setting of the persistent T2-STIR abnormality. Residual T1 and T2 abnormalities have been reported past 8 weeks in some patients (6). However, continued elevation on follow-up may represent chronic indolent myocarditis, or possibly development of diffuse interstitial fibrosis, which is associated with worse outcomes over time (7). Persistent myocardial abnormalities after acute COVID-19 infection have also been shown in several studies, and the true mechanism of myocardial injury after COVID-19 remains unknown (8,9). Fortunately, his myocardial deformation by Strain ENCoded (SENC) imaging appears normal, with recent studies showing the additive value of strain assessment to predict prognosis, particularly in those with normal LVEF (10). Both left ventricular global longitudinal (-18.3%) and global circumferential (-19%) strain were normal based on our institutional and published normative data (11).
The finding of pericardial delayed enhancement (Images 4-5) is an interesting finding given the association between mRNA COVID-19 vaccines and the development of myopericarditis. Although his ventricular function, cardiac biomarkers, and clinical symptoms have improved, he continued to demonstrate abnormalities on CMR, demonstrating its exceptional capabilities in myocardial tissue characterization. We will plan to repeat CMR at 6 months to re-evaluate his myocardium and pericardium prior to clearing him to receive his COVID-19 vaccinations. The family has continued to express support for vaccinating our patient, in part due to his severe illness.
Click here to view the entire study on CloudCMR
References:
1. Eichhorn C, Greulich S, Bucciarelli-Ducci C, Sznitman R, Kwong RY, Gräni C. Multiparametric Cardiovascular Magnetic Resonance Approach in Diagnosing, Monitoring, and Prognostication of Myocarditis. JACC: Cardiovascular Imaging 2022.
2. Oster ME, Shay DK, Su JR et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA 2022;327:331-340.
3. CDC/ACIP. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2022-02-04/12-COVID-Oliver-508.pdf.
4. Veronese G, Ammirati E, Cipriani M, Frigerio M. Fulminant myocarditis: Characteristics, treatment, and outcomes. Anatol J Cardiol 2018;19:279-286.
5. Amabile N, Fraisse A, Bouvenot J, Chetaille P, Ovaert C. Outcome of acute fulminant myocarditis in children. Heart 2006;92:1269-73.
6. Luetkens JA, Homsi R, Dabir D et al. Comprehensive Cardiac Magnetic Resonance for Short-Term Follow-Up in Acute Myocarditis. J Am Heart Assoc 2016;5.
7. Grani C, Biere L, Eichhorn C et al. Incremental value of extracellular volume assessment by cardiovascular magnetic resonance imaging in risk stratifying patients with suspected myocarditis. Int J Cardiovasc Imaging 2019;35:1067-1078.
8. Huang L, Zhao P, Tang D et al. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging 2020.
9. Bailey AL, Dmytrenko O, Greenberg L et al. SARS-CoV-2 Infects Human Engineered Heart Tissues and Models COVID-19 Myocarditis. JACC Basic Transl Sci 2021;6:331-345.
10. Chen Y, Sun Z, Xu L et al. Diagnostic and Prognostic Value of Cardiac Magnetic Resonance Strain in Suspected Myocarditis With Preserved LV-EF: A Comparison Between Patients With Negative and Positive Late Gadolinium Enhancement Findings. J Magn Reson Imaging 2021.
11. Korosoglou G, Giusca S, Hofmann NP et al. Strain-encoded magnetic resonance: a method for the assessment of myocardial deformation. ESC Heart Fail 2019;6:584-602.
Case prepared by:
Jason N. Johnson, MD MHS
Deputy Editor, Cases of SCMR
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center, St. Jude Children’s Research Hospital





