Ritu Agarwal MD1, Rengarajan Rajagopal MD2
Eternal Hospital1, Jaipur, India
All India Institute of Medical Sciences2, Jodhpur, India
Clinical History:
A 54-year-old Indian male, presented to the cardiology clinic with progressive increasing shortness of breath over the last 4 months (NYHA class III). He did not complain of chest pain or palpitations. No systemic symptoms like fever or weight loss were present. The rest of his past medical history was negative.
A chest X-ray was concerning for a pericardial effusion (Figure 1). Transthoracic echocardiogram was done, that confirmed the presence of pericardial effusion, however, additionally raised the possibility of a cystic lesion in the pericardium with possible coronary involvement. The ventricular function was normal (reported LVEF 55%).

Figure 1. Chest x-ray with mediastinal widening concerning for a pericardial effusion.
CT coronary angiography with larger field of view was done to evaluate the cystic lesion, possible coronary artery involvement that showed a large pericardial effusion (Figure 2) and mild pericardial calcification (Figure 4). A multiloculated cystic lesion with enhancing septations within it was noted in close proximity to basal to mid lateral left ventricular (LV) wall, however no intramyocardial extension was seen. The lesion was encasing the left main coronary artery and proximal portions of left anterior descending (LAD), and left circumflex (LCX) coronary arteries with mild narrowing of the LCX (Figure 3 and 4). Possibility of Hydatid cyst was suggested based on this honeycomb pattern, and CMR was ordered for further evaluation and to better characterize the cystic mass.
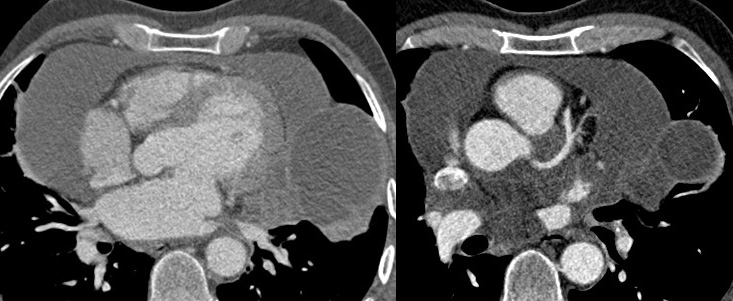
Figures 2 & 3: Chest CT Angiogram with contrast in axial projection showing a multiloculated cystic lesion with enhanced septations encasing the left main coronary artery system.
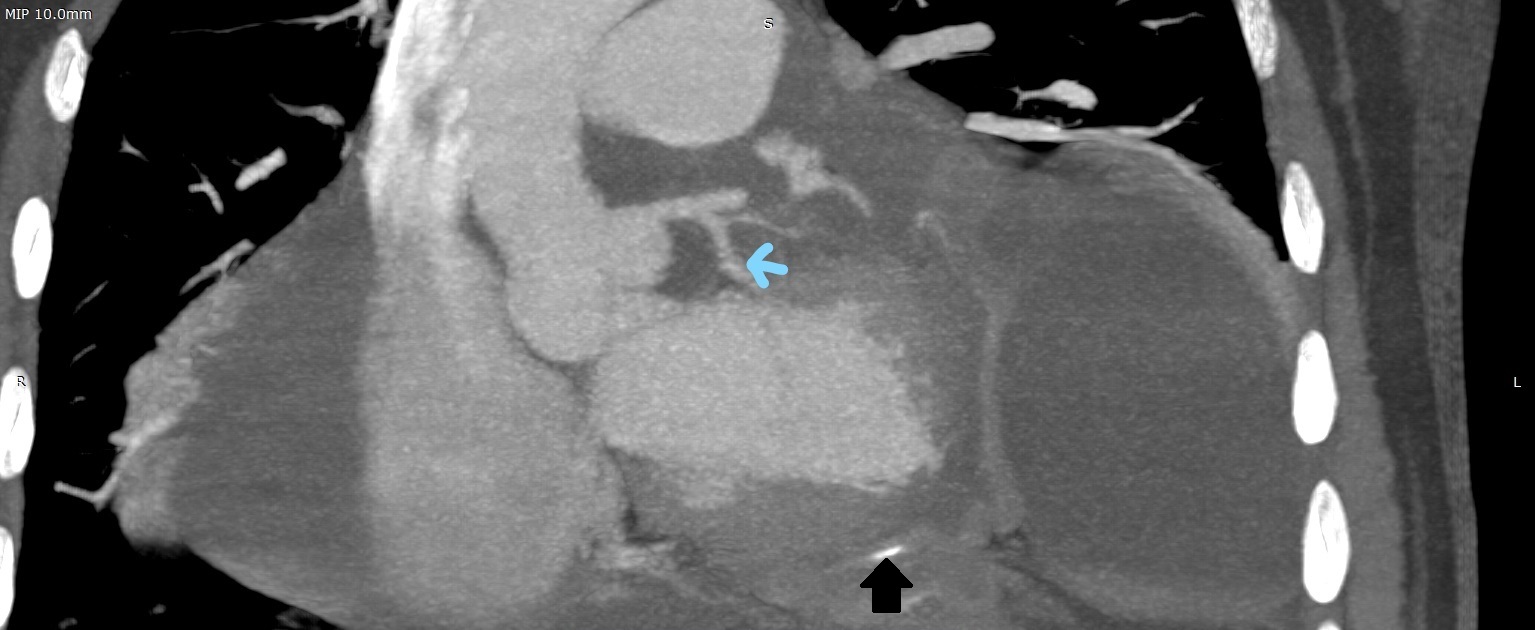
Figure 4. Chest CT Angiogram with contrast in coronal projection showing a multiloculated cystic lesion encasing the left circumflex coronary artery (blue arrow) with subsequent narrowing, and mild pericardial calcification (black arrow).
CMR Findings:
Large pericardial effusion showing heterogeneous signals on cine SSFP images was noted (Movie 1). Mild pericardial thickening was also seen. No significant pericardial enhancement was noted.
Well defined multiloculated cystic lesion was noted in close proximity to mid lateral LV wall (Movie 1&2). The lesion was also extending posterior to the aortic root/ ascending aorta, inferior to the main pulmonary artery and antero-superior to the left atrial appendage. The lesion was multivesicular, with daughter cysts with honeycomb like appearance, suggesting CE-2 (WHO Classification Informal Working Group On Echinococcus) active stage (Movie 2). The cystic lesions were isointense on SSFP and T1 imaging, hyperintense on T2 imaging, and hypointense on perfusion with contrast and late gadolinium enhancement (Figure 5).
Left ventricle was normal in size with mildly reduced systolic function (LVEF 48%, Movie 3). Hypokinesis of the mid lateral LV with decreased perfusion and near transmural enhancement on delayed-enhancement images was noted suggesting scar in LCX distribution (Movie 3-4, Figure 6). Although this corresponds to the LCX distribution, the scar is more likely due to inflammation and scarring from hydatid cyst. The possibility of transmural ischemic scar is unlikely due to non-critical circumflex artery narrowing. The right ventricle was normal in size, systolic function, and no RV scar was seen.
Movie 1 & 2. Four chamber cine SSFP with a large pericardial effusion, multiloclulated cystic lesion along the lateral left ventricular wall, extending posterior to the aortic root, ascending aorta, inferior to the main pulmonary artery and anterior to the left atrial appendage.

Figure 5. Short axis cine SSFP (A), T1 (B), T2 (C), perfusion (D), and phase sensitive inversion recovery (E). The cyst (*) is isointense on SSFP, T1 weighted imaging, hyperintense on T2 weighted imaging, and hypointense on perfusion with contrast and late gadolinium enhancement imaging.
Movie 3 & 4. Short axis cine SSFP and perfusion showing hypokinesia of the mid lateral left ventricular wall with decreased perfusion.

Figure 6. Short axis phase sensitive inversion recovery mid slice showing near transmural late gadolinium enhancement of the mid lateral left ventricular wall (arrow).
Conclusion:
CMR allowed for better characterization of the cyst, as well identified the associated LV wall motion abnormality and scar. Diagnosis of Pericardial hydatid cyst with pericoronary involvement (CE-2 W.H.O Classification Informal Working Group On Echinococcus suggestive of active stage) and large pericardial effusion was made. ELISA for Echinococcus (IgG antibodies) done after CMR examination was positive. Abdominal ultrasound was done for possible intraabdominal cysts that did not reveal any significant abnormality. The patient was advised to proceed with surgical resection due to the risk of cyst rupture, but he opted for medical treatment with albendazole. A follow up imaging was suggested, however patient was lost to follow up.
Perspective:
Cardiac hydatid disease is a rare manifestation of Echinococcus infection. It represents 0.5 to 2% of hydatic disease [1]. The most common location is the LV myocardium followed by the right ventricle, pericardium, pulmonary artery, interventricular septum, the left atrium, the right atrium, and interatrial septum. Hydatid disease in endemic in many parts of world, including India. The annual incidence in India varies from 1 to 200 per 100000 population [2]. Dogs and cats are primary carriers of this parasite. Humans can be infected as an intermediary carrier when they eat unwashed or uncooked vegetables or swallow the parasite eggs. The clinical presentation may vary from asymptomatic cases to fever, chest pain, dyspnea on exertion and anaphylactic shock due to cyst rupture. Less likely complications like systemic or pulmonary hydatid embolism, valve obstruction, papillary muscle involvement with secondary mitral regurgitation, and invasion into the conduction system with arrhythmias have also been described.
Diagnosis can be made using imaging and serology. The presence of a uni- or multivesicular cyst, with a honeycomb appearance is characteristic of the echinococcal cyst. The WHO-Informal Working Group on Echinococcosis (WHO-IWGE) developed an international ultrasound classification. According to this classification, cysts pass through CE1 (active) through CE5 (inactive) phases [3]. The hydatid serology was positive in our patient and often positive in the literature, but its negativity does not eliminate the diagnosis [4].
Surgery is the treatment of choice for cardiac hydatid cysts, however in some cases medical treatment is advocated. These include small or calcified cysts, in elderly patients, or when surgery is contraindicated or refused by the patient; as in our case. Pericardium is an unusual location of hydatid disease, and it needs to be considered in the differential diagnosis of pericardial effusion especially if there is a prior history of hydatid disease, a contact with animals, and in endemic countries.
Click here to view the entire CMR on CloudCMR.
Click here to view the entire CTA with contrast on CloudCMR.
1. Kosecik M, Karaoglanoglu M, Yamak B (2006) Pericardial hydatid cyst presenting with cardiac tamponade. Can J Cardiol 22(2). 10.1016/S0828-282X(06)70254-9.
2. International Surgery Journal Mathur PN et al. Int Surg J. 2016 Nov;3(4):1802-1805 http://www.ijsurgery.com
3. WHO-IWGE. Puncture, aspiration, injection, re-aspiration: an option for the treatment of cystic echinococcosis. Geneva: WHO; 2001. Available from: WHO/CDS/CSR/APH/2001.6 whqlibdoc.who.int/hq/2001/WHO_CDS_CSR_APH_2001.6.pdf
4. Firouzi A, Pir Borj MN, Ghavidel AA. Cardiac hydatid cyst: A rare presentation of echinococcal infection. J Cardiovasc Thorac Res
. 2019;11(1):75-77.
Case prepared by:
Jason N. Johnson, MD MHS
Deputy Editor, Cases of SCMR
Le Bonheur Children’s Hospital, University of Tennessee Health Science
Center, St. Jude Children’s Research Hospital







