Anomalous Left Coronary Artery Arising from the Pulmonary Artery in an Adolescent
Namrita Mozumdar MD, Mark Cartoski MD, Shannon Nees MD
Nemours Children’s Health, Wilmington, Delaware, USA
Clinical History:
A 17-year-old female presented for evaluation of syncope and hypertension. Her history was consistent with vasovagal syncope, and she was normotensive. She had no chest pain or exercise intolerance. Physical exam was significant for a continuous murmur and an electrocardiogram demonstrated an abnormal Q wave in lead aVL (Figure 1). Transthoracic echocardiography was notable for an anomalous left coronary artery arising from the main pulmonary artery (ALCAPA) and severely dilated right coronary artery with suspected collateralization to the left ventricular (LV) myocardium (Figure 2). Color Doppler mapping demonstrated retrograde low velocity flow from anomalous left coronary artery to the pulmonary artery (Movie 1). There was no evidence of pulmonary hypertension on echocardiogram. There was normal left ventricular size and systolic function. A retrospective ECG-gated CT angiogram of the chest was then performed to confirm the coronary anatomy, which demonstrated the left main coronary artery originating from the main pulmonary artery (Figure 3). Cardiovascular magnetic resonance (CMR) was obtained to confirm LV size, cardiac function, and for tissue characterization.
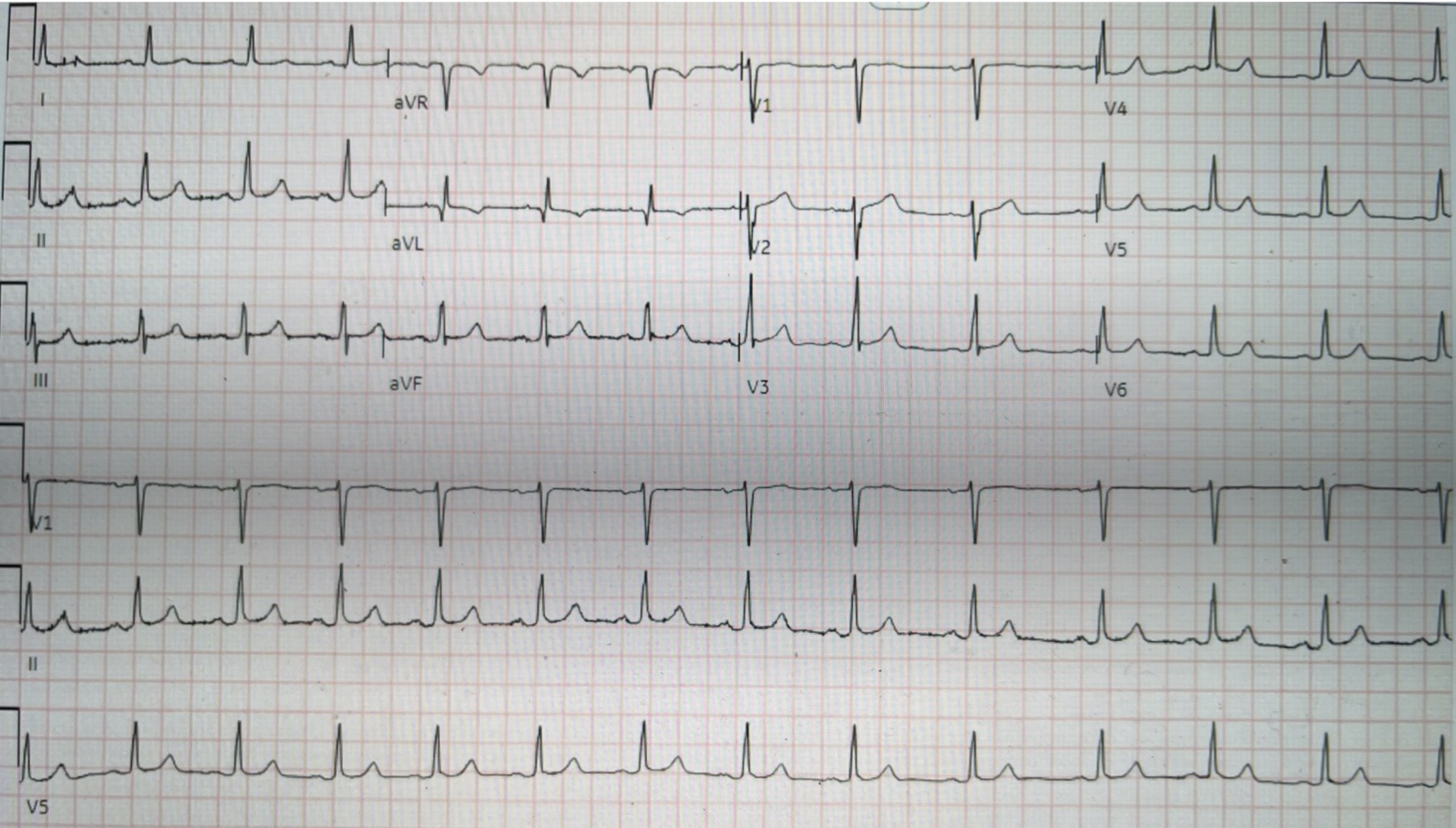
Figure 1. Twelve lead electrocardiogram showed normal sinus rhythm with a Q wave in lead aVL.

Figure 2. Transthoracic echocardiogram parasternal short axis at aortic valve (A,B) and at main pulmonary artery (C). Dilated right coronary artery and an anomalous left coronary artery from the pulmonary artery. Ao = Aorta; AoR = aortic root; LMCA = left main coronary artery; MPA = main pulmonary artery; RCA = right coronary artery;
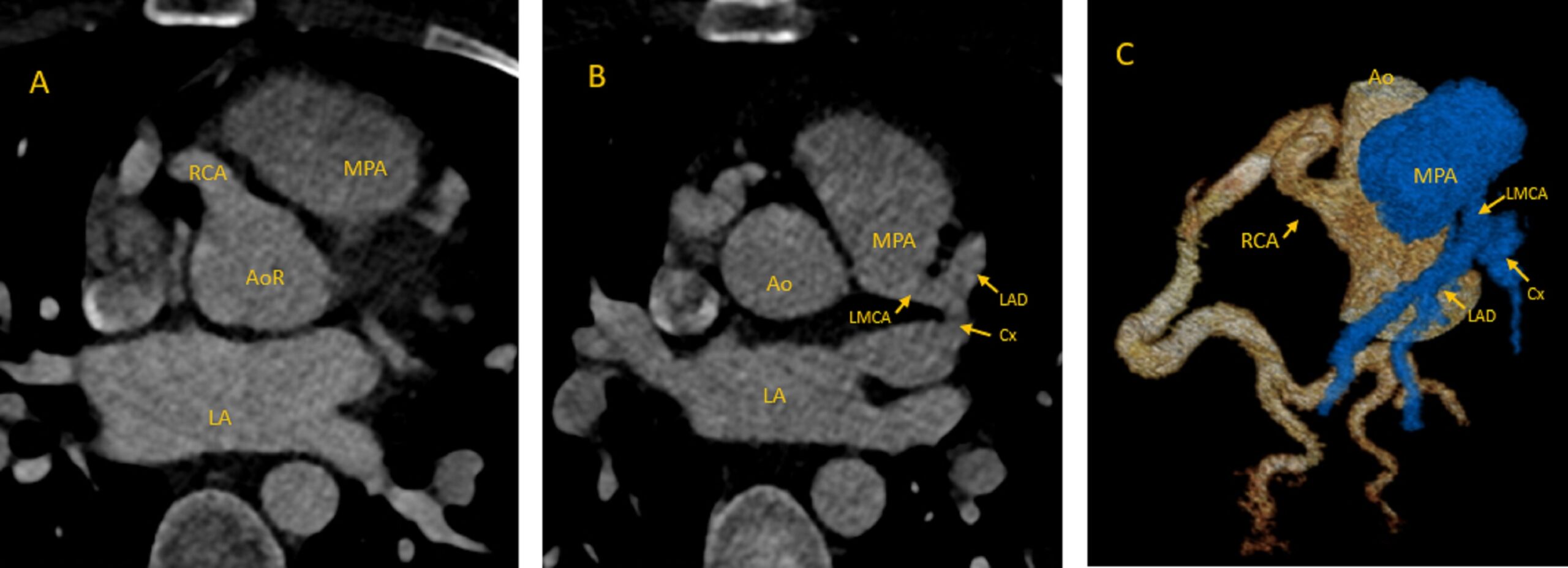
Figure 3. Retrospective ECG-gated CT angiogram of the chest in the axial projection at the aortic valve (A) and main pulmonary artery (B) and 3D reconstruction (C). The left main coronary artery originated from the main pulmonary artery and the right coronary artery was dilated. Ao = Aorta; AoR = aortic root; Cx = circumflex coronary artery; LA = left atrium; LAD = left anterior descending coronary artery; LMCA = left main coronary artery; MPA = main pulmonary artery; RCA = right coronary artery;
Movie 1. Transthoracic echocardiogram high parasternal short axis color compare. The color Doppler mapping demonstrated retrograde low velocity flow from anomalous left coronary artery to the pulmonary artery.
CMR Findings:
CMR was performed on a 1.5 Tesla GE Signa HDxt (General Electric HealthCare, Chicago, Illinois, USA) scanner. 3D steady state free precession images confirmed the anomalous origin of the left main coronary artery from the main pulmonary artery (Figure 4). Short axis cine imaging demonstrated normal LV size (LV end-diastolic volume index: 104.9 ml/m2) and normal LV systolic function (LV ejection fraction 57%). There were no segmental wall motion abnormalities (Movie 2). On late gadolinium enhancement imaging, there was no evidence of myocardial fibrosis by delayed myocardial enhancement (Figure 5).

Figure 4. 3D steady state free precession images at axial projection. Anomalous origin of the left main coronary artery from the main pulmonary artery and dilated right coronary artery present. LMCA = left main coronary artery; RCA = right coronary artery.
Movie 2. Short axis stack cine steady state free precession. There is normal left ventricular size and systolic function with no segmental wall motion abnormalities. The anomalous left main coronary artery from the pulmonary artery (yellow arrow) and dilated right coronary artery (white arrow) is seen.
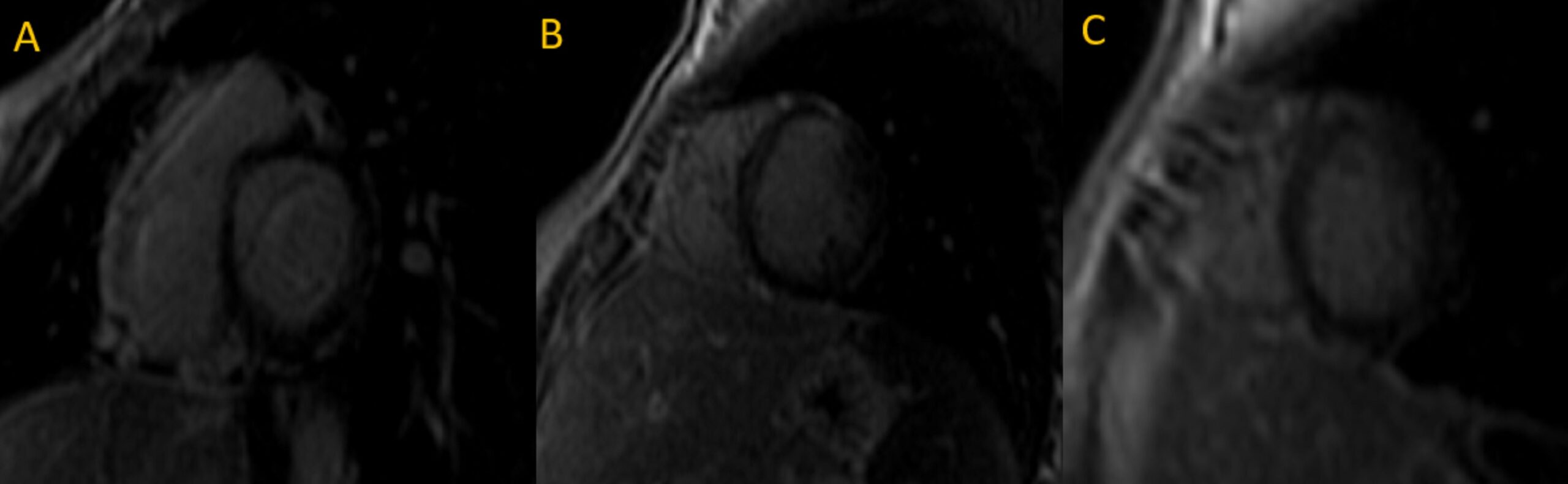
Figure 5. Short axis base (A), mid (B), apical (C) late gadolinium enhancement imaging. There was no evidence of myocardial fibrosis or scar present.
Conclusion:
CT angiography and MRI findings confirmed the diagnosis of ALCAPA without evidence of myocardial ischemia, wall motion abnormalities, or left ventricular dilation. Since there is a lifetime risk of ischemia, sudden cardiac death, and ventricular arrhythmias with this coronary anomaly, surgical intervention was recommended. Patient underwent surgical repair with bovine pericardial patch closure of the pulmonary artery origin of the left main coronary artery and has been clinically doing well post repair.
Perspective:
ALCAPA is a rare congenital heart defect. This coronary anomaly is associated with a high risk of mortality in infancy and sudden death in adults [1]. In fetal life, when pulmonary vascular resistance is high, blood flows from pulmonary artery to the anomalous left coronary artery perfusing the left ventricle. After birth, when pulmonary vascular resistance falls, blood flow in the left coronary artery is reversed with flow going from the left coronary into the pulmonary artery resulting in a left to right shunt and coronary artery steal. This can lead to a mismatch in myocardial demand and coronary blood flow causing myocardial ischemia. Collateral vessels can form between the right and left coronary arteries perfusing the myocardium, which can lead to prominent dilation of the right coronary artery. The degree of ischemia is dependent on the extent of collateralization [2, 3]. Most patients present in infancy with cardiomegaly and symptoms of congestive heart failure. Rarely, ALCAPA can present later in life, known as adult type, due to significant collateral vessel formation which prevents symptoms in infancy. Because collateral vessels may not be adequate to supply the entire left ventricular myocardium, these patients can present with myocardial ischemia, mitral insufficiency, ventricular arrhythmia, and left ventricular dysfunction [2]. Those presenting later in life may have symptoms of chest pain, palpitations, or shortness of breath. Rarely, patients may be asymptomatic as our patient was. A continuous murmur at the upper left sternal border can be heard on physical exam due to continuous flow from collateral vessels.
Management differs depending on the age and severity of presentation. In infancy, there is high mortality in first year of life if left unrepaired so surgical repair is indicated at the time of diagnosis. Survival to adulthood depends on the degree of collateral vessel formation. ALCAPA can also be life-threatening in adults leading to ventricular arrhythmias and sudden death. Stress echocardiogram can be performed to assess for regional wall motion abnormalities as evidence of focal ischemia. Additional advanced imaging can be helpful in older patients prior to surgical intervention. Coronary computed tomography angiography can help confirm coronary anatomy in adults with suboptimal echocardiographic images, and may also determine the extent of collateral vessels. CMR is used primarily to evaluate for left ventricular dysfunction and myocardial fibrosis [3] as was done in this case, which may help assess risk of recurrent ventricular arrhythmias due to myocardial fibrosis.
Given the risk of life-threatening arrhythmias and sudden death, surgical correction is usually recommended. The goal of surgical treatment is to prevent coronary artery steal and ensure that all areas of the myocardium are adequately perfused. In infancy, the left main coronary artery can typically be directly reimplanted to the aorta. An alternative approach is the Takeuchi technique, where an intrapulmonary tunnel is created from left coronary ostia to aorta. In adults, the left coronary artery can be ligated and revascularized with coronary artery bypass graft [3]. Gouda et al. support a conservative surgical approach in elderly patients over age 65 with extensive collateralization by performing only suture ligation of left coronary artery and avoiding the need for cardiac bypass [3]. In these cases, blood flow to the left coronary artery territory is provided solely through collaterals but the risk of coronary steal is alleviated and the left to right shunt is removed. In our patient, there was a significant network of collaterals found in the operating room arising at the base of the pulmonary artery and anomalous left coronary. Reimplantation of the left coronary artery to the aorta could have interrupted significant blood flow to the myocardium, and so patch closure of the pulmonary artery origin of the left coronary was performed. Implantable cardioverter-defibrillator (ICD) can also be considered as secondary prevention in those patients noted to have myocardial fibrosis on MRI [4]. In this case, CMR showed no LV dysfunction or myocardial fibrosis.
Click here to view the images on CloudCMR.
References:
- Yau JM, Singh R, Halpern EJ, Fischman D. Anomalous origin of the left coronary artery from the pulmonary artery in adults: a comprehensive review of 151 adult cases and a new diagnosis in a 53-year-old woman. Clin Cardiol. 2011 Apr;34(4):204-10.
- Trevizan LLB, Nussbacher A, da Silva MCB, Ishikawa WY, de Oliveira SA, Sitta MDCzarf G. Anomalous origin of the left coronary artery from the pulmonary artery as a rare cause of left ventricular dysfunction. Circ Cardiovasc Imaging. 2019 Dec;12(12):e009724.
- Gouda P, Gouda J, Butler C, Welsh RC. Late presentation of an anomalous left coronary artery from the pulmonary artery treated with conservative surgical management with long-term cardiac magnetic resonance imaging follow-up. SAGE Open Med Case Rep. 2017 Feb 23:5:2050313X17695719.
- Prandi FR, Zaidi AN, LaRocca G, Hadley M, Riasat M, Anastasius MO, Moreno PR, Sharma S, Kini A, Murthy R, et al. Sudden cardiac arrest in an adult with anomalous origin of the left coronary artery from the pulmonary artery (ALCAPA): Case Report. International Journal of Environmental Research and Public Health. 2022; 19(3):1554.
Case prepared by:
Jason N. Johnson, MD MHS
Associate Editor, Cases of SCMR
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center, St. Jude Children’s Research Hospital







