Andrew Andreae, MD; Michael Campbell, MD; Han Kim, MD
Division of Cardiology, Duke University Medical Center, Durham, North Carolina, USA
Division of Pediatric Cardiology, Duke University Medical Center, Durham, North Carolina, USA
Clinical History:
A 68-year-old female with history of premature ventricular contractions (PVC) and longstanding murmur since teenage years presented for outpatient evaluation of palpitations. On history, she reported three months of “irregular heartbeats” after eating, exercise, and with stress. She denied associated dizziness, presyncope, chest pain, or shortness of breath. Physical examination revealed a 3/6 systolic murmur best heard over the right upper sternal border. Electrocardiograph revealed left atrial enlargement, left ventricular hypertrophy (LVH), and PVCs (Figure 1). Initial labs were normal including thyroid stimulating hormone, chemistries, and blood counts. For the above, she was referred for echocardiography.
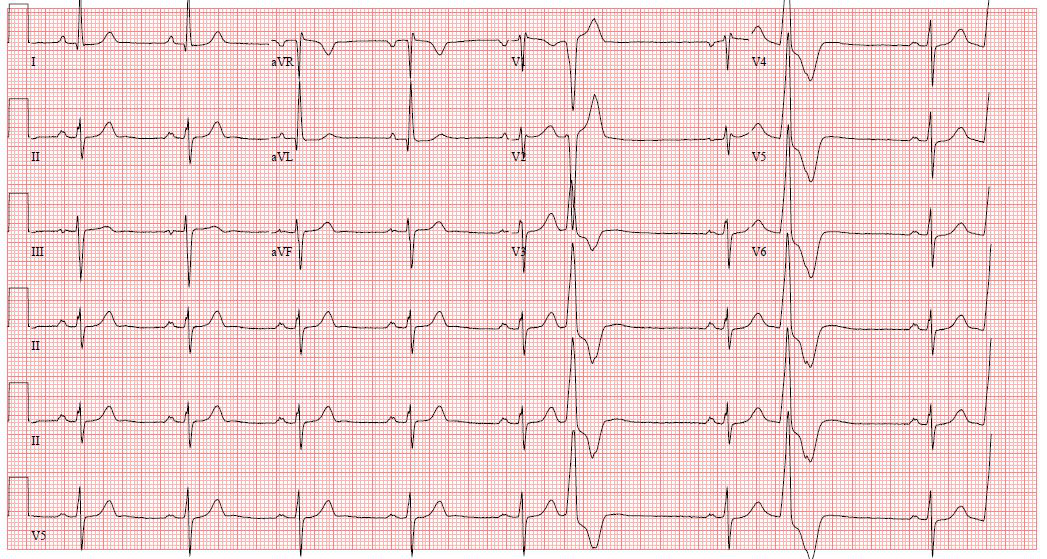
Figure 1: Electrocardiogram revealing left atrial enlargement, left ventricular hypertrophy, and PVCs.
Initial transthoracic echocardiogram noted normal biventricular function (Movie 1), mild left ventricular (LV) hypertrophy (septal wall thickness 1.3 cm), systolic anterior motion of the mitral valve with mild mitral regurgitation (MR), moderate left ventricular outflow tract (LVOT) gradient, moderate tricuspid regurgitation, biatrial enlargement, and flow from the left atrium (LA) to right atrium (RA) presumably from an intra-atrial septal defect (Movie 2). Given unclear anatomy on echocardiogram, the patient was referred for cardiac MRI (CMR).
Movie 1: Echocardiography apical four chamber revealing normal LV function and frequent PVCs in bigeminy pattern.
Movie 2: Echocardiography subcostal showing possible left to right intra-atrial septal defect.
CMR Findings (3T):
CMR was performed on a 3T Siemens MAGNETOM Vida scanner. Cine imaging demonstrated normal LV cavity size and systolic function with ejection fraction 79% (Movie 3). The patient had a basal sigmoid septum with maximal thickness 1.4 cm. There were no regional wall motion abnormalities. The right ventricle (RV) was normal in cavity size, wall thickness, and systolic function. LV outflow obstruction was present due to chordal systolic anterior motion and had a peak velocity of at least 2.8m/s. Additional findings included small bilateral pleural effusions, tubular ascending aorta dilated to maximum 4.2 cm, and mild dilation of the main and proximal branch pulmonary arteries.


Movie 3: Long and short axis cine images showing mild LVH, normal LV and RV function, and no segmental wall motion abnormalities. Sigmoid septum is present with associated subaortic obstruction visible on long axis 3 chamber view. The cleft left AV valve is visible on the parasternal short axis basal view.
A transitional atrioventricular canal defect (AVCD) comprised of three parts was seen on sequential four chamber stack cine images (Movies 4-6). First there was a primum atrial septal defect (ASD) with left-to-right flow consistent with what was seen on echocardiogram. Second, there was an anatomically small inlet ventricular septal defect (VSD) partially covered by accessory AV valve tissue. Third, the left AV valve was found to be cleft with associated mild regurgitation and LVOT obstruction (Movie 3). Finally, there was systolic flow from the LV to RA, consistent with a Gerbode defect. Together, these defects led to a Qp:Qs = 1.3, which was calculated by comparison of RV stroke volume to LV stroke volume in cine CMR.
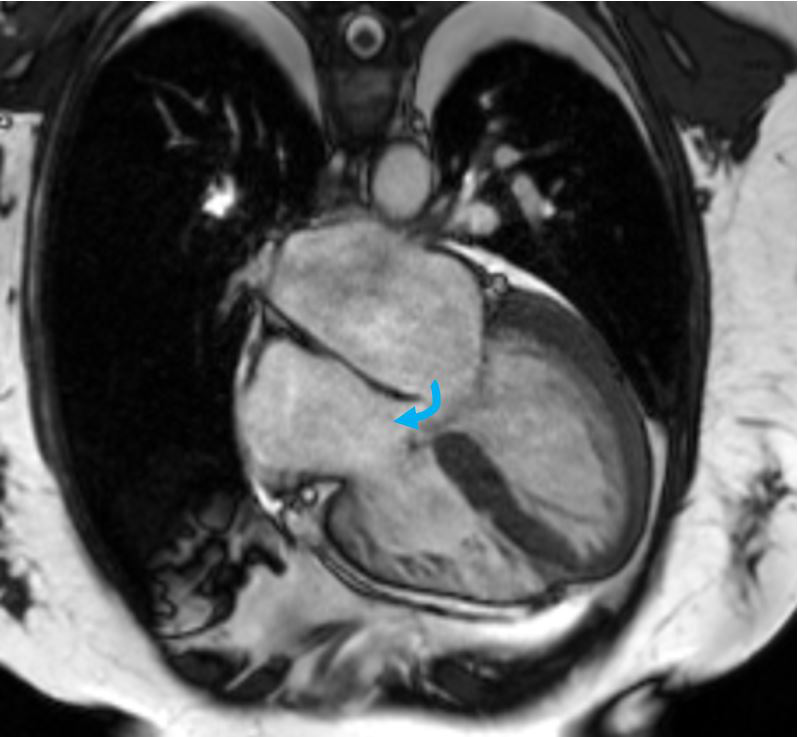
Movie 4: Most superior four chamber stack cine image showing ASD with flow from the LA to RA (blue arrow).
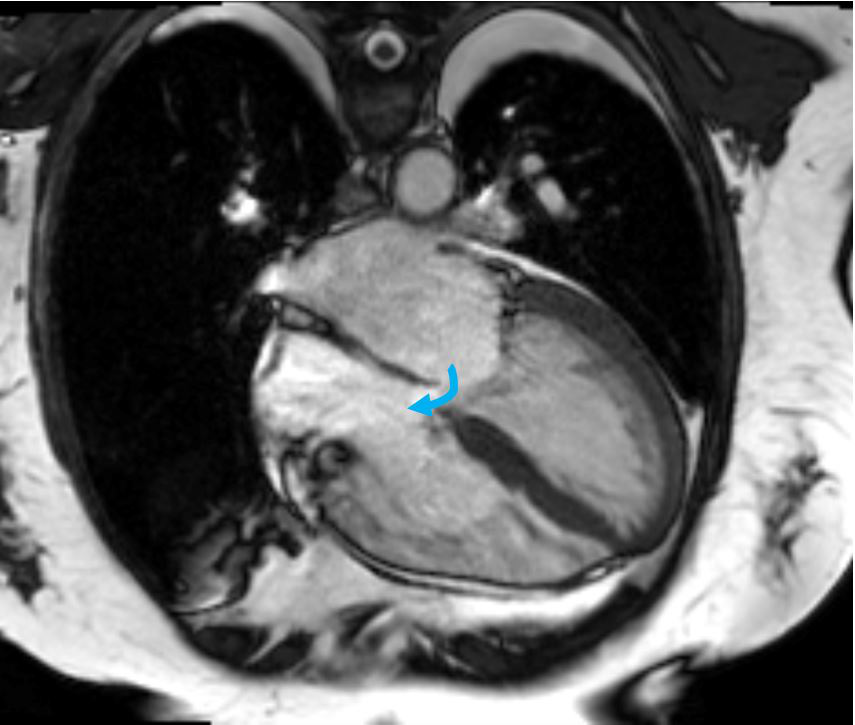
Movie 5: Stepdown four chamber stack cine image showing ASD with flow from the LA to RA (blue arrow).

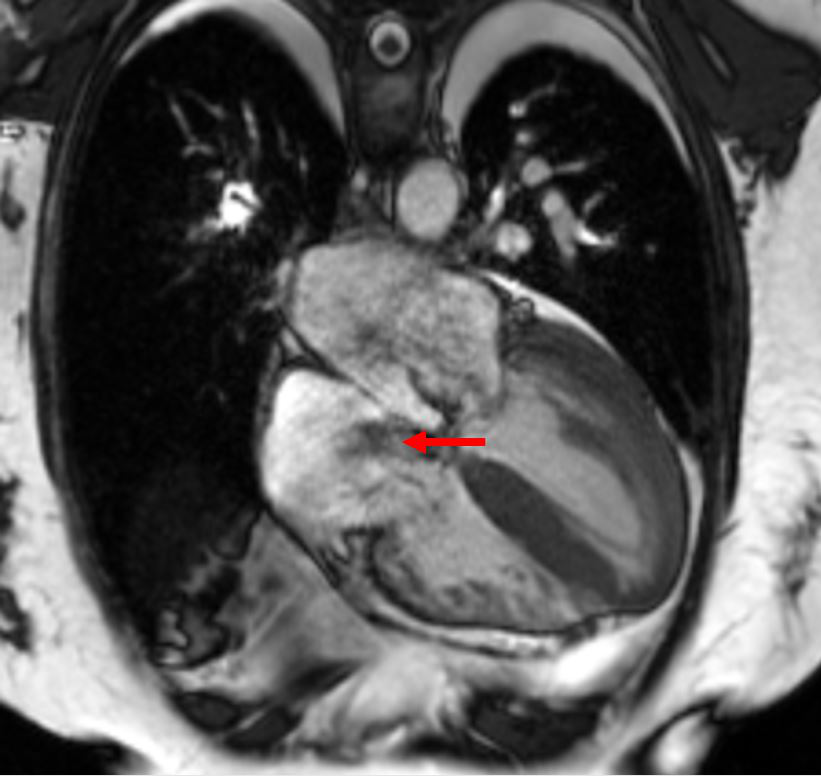
Movie 6: Most inferior four chamber stack cine image showing Gerbode ventriculo-atrial defect with systolic flow from the LV to RA (red arrow).
Short axis stack cine images also reveals the partial AVSD and Gerbode defect in sequential images (Figures 2, 3).
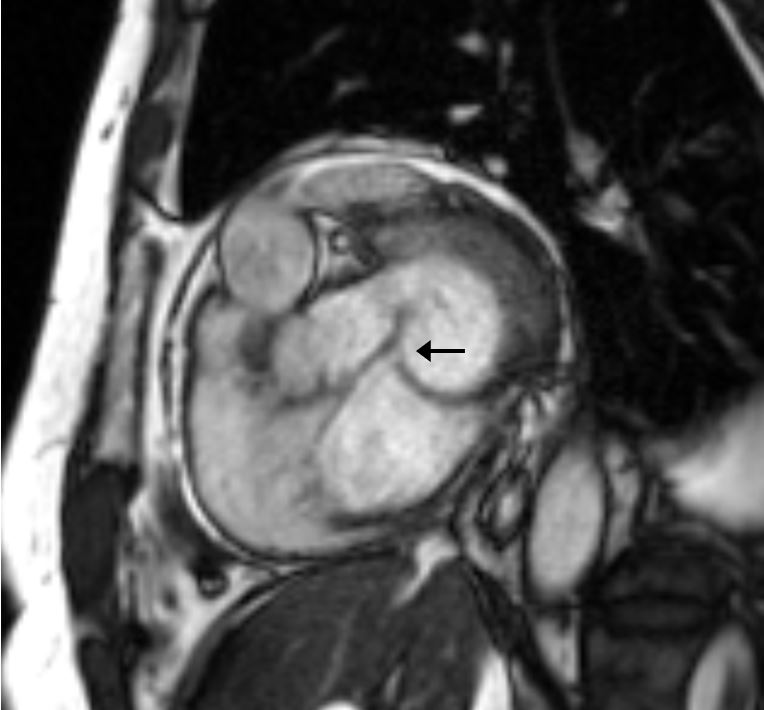
Figure 2: AVCD in short axis (black arrow) between the left atrium and right atrium.

Figure 3: Gerbode Defect in short axis (white arrow) between the left ventricle and the right atrium.
Conclusion:
The patient’s CMR findings of transitional AV canal defect and Gerbode defect were likely the source of the patients 3/6 systolic murmur heard along the left sternal border. Given the relatively low volume of her shunt with Qp:Qs = 1.3, she held relatively few other symptoms, other that frequent PVC’s, which may have been related to her underlying structural heart disease. Regarding her LVOT obstruction, she did not have any associated symptoms including presyncope, syncope, or chest pain.
Given the patients age at diagnosis & minimal symptoms, the patient has been managed conservatively without surgical intervention with aggressive afterload reduction via anti-hypertensive medications. She continues to do well with minimal symptoms.
Perspective:
The Gerbode defect is defined as an abnormal shunt from the LV to the RA during systole. It is a rare cause of intracardiac shunts, accounting for <1% of all congenital cardiac defects.[1] This lesion was first decreased in 1838 by Thurnam J., but was named after Frank Gerbode who first wrote a case series on the surgical repair of five cases in 1958.[2,3] The historical primary cause of Gerbode defects was congenital, however due to increasing number of invasive cardiac procedures, acquired Gerbode defects have now become the predominant etiology.[4] In about one-third of embryologic cases, additional malformations also occur such as patent foramen ovale or atrial septal defect (as present in this patient).[5] In this case, the presence of multiple defects are consistent with an AVCD, which have been further categorized and detailed in review.[6] It is suspected her defect was congenital in origin given the murmur since childhood and no prior intracardiac procedures.
Regarding diagnosis, symptoms of Gerbode defects range from asymptomatic to severe with heart failure symptoms based on size of the shunt.[7] Physical examination typically reveals a murmur similar to a VSD, with holosystolic grade 3-6 pansystolic murmur along the left sternal border.[7,8] Prior to invention of advanced imaging, the defect historically was diagnosed at time of cardiac surgery. In the present, it can be diagnosed via transthoracic echocardiography, transesophageal echocardiography, and CMR. CMR is of high utility in these cases due to its unique ability to enhance the shunt anatomy, quantify shunt flow and ratios, and identify other associated congenital defects.[9]
The need for surgical repair of Gerbode defects is decided based on patient comorbidities, severity of symptoms, presence of associated heart failure symptoms, and magnitude of shunt volume.[1] Small defects and asymptomatic patients can be managed conservatively, as done with this patient.[10]
This case illustrates the value of obtaining CMR in patients with suspected congenital heart defect, even when portions of abnormal anatomy are visualized on transthoracic echocardiography. CMR allows for detailed mapping of congenital defects, shunt size and volume quantifications, and discovery of associated cardiac defects. CMR findings can help determine whether congenital heart defects discovered in adulthood require surgical repair, thus minimizing burden of morbidity to patients.
Click here to view the entire CMR on CloudCMR.
References:
- Saker E, Bahri GN, Montalbano MJ, et al. Gerbode defect: A comprehensive review of its history, anatomy, embryology, pathophysiology, diagnosis, and treatment. J Saudi Heart Assoc. 2017;29(4):283-92.
- Thurnam J. On aneurisms of the heart with cases. Med Chir Trans. 1838;21:187-438.9.
- Gerbode F, Hultgren H, Melrose D, Osborn J. Syndrome of left ventricular-right atrial shunt: successful surgical repair of defect in five cases, with observation of bradycardia on closure. Annals of surgery. 1958 Sep;148(3):433.
- Yuan SM. A Systematic Review of Acquired Left Ventricle to Right Atrium Shunts (Gerbode Defects). Hellenic J Cardiol. 2015;56(5):357-72.
- Riemenschneider TA, Moss AJ. Left ventricular-right atrial communication. Am J Cardiol. 1967;19(5):710-8.
- Umapathi KK, Agasthi P. Atrioventricular Canal Defects. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557511/).
- Sinisalo JP, Sreeram N, Jokinen E, Qureshi SA. Acquired left ventricular-right atrium shunts. Eur J Cardiothorac Surg. 2011;39(4):500-6.
- Barclay RS, Reid JM, Coleman EN, Stevenson JG, Welsh TM, McSwan N. Communication between the left ventricle and right atrium. Thorax. 1967;22(5):473-7.
- Taskesen T, Prouse AF, Goldberg SL, Gill EA. Gerbode defect: Another nail for the 3D transesophagel echo hammer. Int J Cardiovasc Imaging. 2015;31(4):753-64.
- Kelle AM, Young L, Kaushal S, Duffy CE, Anderson RH, Backer CL. The Gerbode defect: the significance of a left ventricular to right atrial shunt. Cardiol Young. 2009;19
Case prepared by:
Madhusudan Ganigara, MD
Editor, Cases of SCMR
Division of Cardiology, Department of Pediatrics
The University of Chicago & Biological Sciences
5841 S. Maryland Avenue, Chicago, IL 60637





