Alexander L. Bowers, DO; M. Jay Campbell, MD
Duke University Medical Center, Durham, NC, USA
Clinical History:
A 13-year-old male with a history of an anomalous aortic origin of the right coronary artery (RCA) from the left sinus of Valsalva had a history of chest pain with exertion (Figure 1). Because of these symptoms he was referred for surgical repair. Direct inspection in the operating room revealed that the RCA origin had a very short intramural segment and this passed immediately underneath the intracoronary commissure. Unroofing of the RCA was not felt to be appropriate so coronary artery translocation of the RCA to the right supra-sinotubular junction was performed. His post-operative course was uneventful and he was discharged home on post-operative day three. One week later he had an acute episode of chest pain with elevated high sensitivity troponin peaking at 3,911 ng/L (Rule-out normal range <3 ng/L) and ST segment elevations on electrocardiogram (ECG) (Figure 2). There was moderate to severely reduced right ventricular (RV) function on echocardiogram with hypokinesis of the basolateral and mid-lateral segments. He underwent cardiac catheterization which revealed severe proximal narrowing of the RCA. At that time, a drug eluting stent was placed in the proximal RCA. ECG changes, troponin levels, and RV function ultimately normalized. Six months later, he was doing well and underwent exercise stress test that was normal. Cardiac magnetic resonance imaging (CMR) was also obtained for myocardial viability assessment.
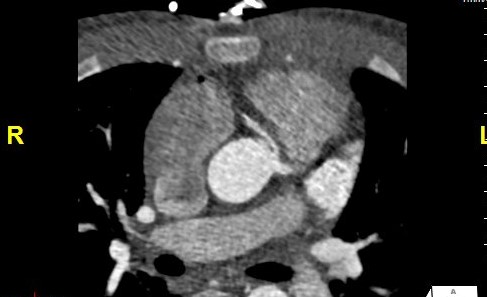
Figure 1. Axial slice of CTA demonstrating the RCA originates from the left sinus of Valsalva adjacent to the intracoronary commissure and origin of the left main coronary artery. The RCA demonstrates acute angle takeoff and narrowing with suggestion of intramural segment.
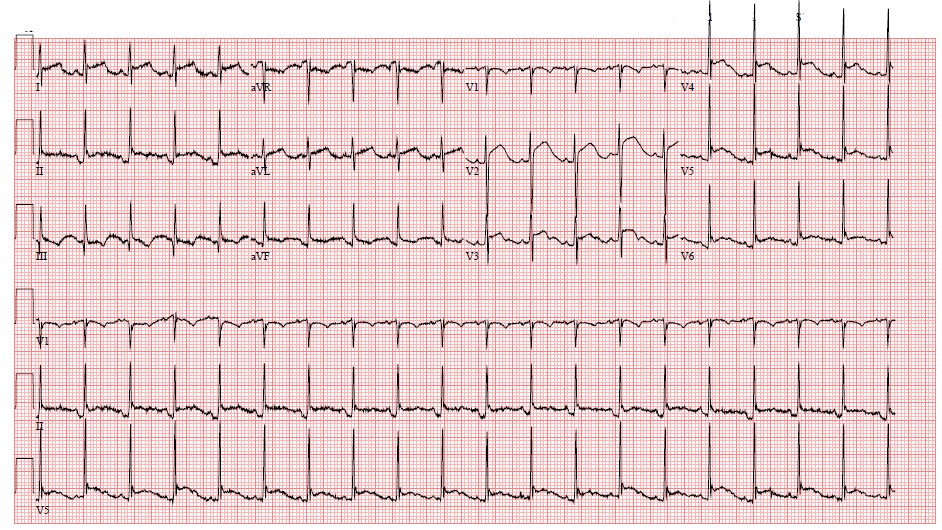
Figure 2. Electrocardiogram from admission demonstrating ST segment elevation in inferoseptal leads.
CMR Findings:
A CMR scan was performed on a 3T Sola (Siemens Healthineers AG, Erlangen, Germany). The scan was performed 6 months after RCA occlusion and stent placement. There was normal preserved right and left global systolic function with hypokinesia of the basal to mid inferoseptal wall (Movie 1). Late gadolinium enhancement (LGE) revealed a subendocardial infarction in the basal inferoseptal wall consistent with a RCA distribution (Figures 3,4).
Movie 1. A cine short axis image at the base of the heart revealing reduced inferoseptal wall motion. The remaining wall segments have normal wall motion. Global left ventricular (LV) systolic function was normal with a quantitative LVEF of 61.3%. Global RV systolic function was also normal with a quantitative RVEF of 50.2%.

Figure 3. Single shot phase sensitive inversion recovery delayed enhancement short axis image revealing subendocardial hyperenhancement of the inferoseptal wall from the base to the mid-ventricular level.
Figure 4. Segmented black blood delayed enhancement image (Flow-Independent Dark-Blood Delayed enhancement (FIDDLE)) revealing subendocardial hyper-enhancement of the basal inferoseptal wall.
Conclusion
This patient had an area of LV scar on CMR in an area of the distribution of the RCA consistent with an infarct secondary to the ischemic event following the occlusion of his implanted RCA. Initially, there was RV dysfunction that improved on echo follow up. CMR was performed approximately 6 months post the ischemic event and demonstrated continued improved function with region of scar, as above. A nuclear medicine stress test was performed about 1 year after event and demonstrated evidence of prior infarction but no inducible ischemia. He currently is monitored clinically without significant sports restrictions and continues to have normal function.
Perspective:
Anomalous aortic origin of a coronary artery (AAOCA) exists in 0.1 to 1% of the general population with the majority of cases involving the origin of right coronary artery (67%).[1] There is often an intramural segment of the coronary artery with the anomalous origin.[1] AAOCA is considered the second most common cause of sudden cardiac death in young athletes. [2] Patients are often diagnosed incidentally, but at times can be associated with evaluations for chest pain especially with exertion.
Late gadolinium enhancement [LGE] in cardiac MRI is a standard imaging method for evaluation of infarcted myocardium showing high signal intensity compared to the intensity in normal myocardium.[3,4] Infarcted myocardium appears bright and, in the setting of subendocardial infarctions, can be difficult to distinguish from the bright blood pool. Black blood LGE techniques such as Flow-Independent Dark-Blood Delayed enhancement [FIDDLE] are beneficial tools to better visualize subendocardial infarction.[5,6] Additionally, scar size has been shown to decrease but not completely resolve over time on follow up CMR. [7] Cardiac MR continues to be the gold standard for evaluation of myocardial scar post myocardial ischemic event.
Treatment of AAOCA remains controversial and can range from observation to surgical repair, especially in the setting of an anomalous right coronary artery.[1] Signs or symptoms of myocardial ischemia are considered as an indication for surgical repair. In patients who are 30 years-old or less, this only accounts for about 15% of patient who are surgically repaired.[7] Asymptomatic patients with an incidental diagnosis, who are the majority of cases, require further evaluation to determine candidacy for surgical intervention. These would include provocative ischemia testing with a treadmill test. Those patients with an anomalous origin of the left coronary artery are often offered surgical repair, regardless if perfusion defects are seen, as these patients have higher incidence of sudden cardiac death [up to 85% of all AAOCA sudden death cases].[2,8,9] Patients with anomalous origin of the right coronary artery make up a much smaller, yet not completely insignificant percentage of patients with sudden cardiac death. Because of the risk of post-operative complications, surgical repair is primarily offered if there is clear evidence of ischemia, whether that is clinically or through proactive testing.[2,8,9] Additionally, evaluation of length of intramural course and age of the patient, have been proposed as considerations for repair. [2]
Historically, surgical care has been postulated as a way to prevent myocardial ischemia and sudden cardiac death, although true benefit is controversial. Techniques can include coronary unroofing, neo-ostium creation, and transection with reimplantation, as in our case.[2] Post-operative outcomes are often excellent. Complications most commonly include acute pericarditis, pericardial effusions, aortic valve insufficiency, and rarely, cardiac ischemia/infarction and sudden cardiac arrest.[8,10] This case illustrates an example of one of these complications and its subsequent CMR findings.
Click here to view the entire CMR on CloudCMR.
References:
- Poynter JA, Williams WG, McIntyre S, Brothers JA, Jacobs ML; Congenital Heart Surgeons Society AAOCA Working Group. Anomalous aortic origin of a coronary artery: a report from the Congenital Heart Surgeons Society Registry. World J Pediatr Congenit Heart Surg. 2014;5(1):22-30. doi:10.1177/2150135113516984
- Bonilla-Ramirez C, Molossi S, Caldarone CA, Binsalamah ZM. Anomalous Aortic Origin of the Coronary Arteries – State of the Art Management and Surgical Techniques. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2021;24:85-94. doi:10.1053/j.pcsu.2021.03.004
- Wu ZH, Sun LP, Liu YL, et al. Fully Automatic Scar Segmentation for Late Gadolinium Enhancement MRI Images in Left Ventricle with Myocardial Infarction. Curr Med Sci. 2021;41(2):398-404. doi:10.1007/s11596-021-2360-z
- Wu Y, Tang Z, Li B, Firmin D, Yang G. Recent Advances in Fibrosis and Scar Segmentation From Cardiac MRI: A State-of-the-Art Review and Future Perspectives. Front Physiol. 2021;12:709230. Published 2021 Aug 3. doi:10.3389/fphys.2021.709230
- Kim HW, Rehwald WG, Jenista ER, Wendell DC, Filev P, van Assche L, Jensen CJ, Parker MA, Chen EL, Crowley ALC, Klem I, Judd RM, Kim RJ. Dark-Blood Delayed Enhancement Cardiac Magnetic Resonance of Myocardial Infarction. JACC Cardiovasc Imaging. 2018 Dec;11(12):1758-1769. doi: 10.1016/j.jcmg.2017.09.021. Epub 2017 Dec 13. PMID: 29248655; PMCID: PMC5993564.
- Aboul Enein F, Allaaboun S, Khayyat S, et al. Association Between Myocardial Scar Burden and Left Ventricular Ejection Fraction in Ischemic Cardiomyopathy. Cureus. 2020;12(12):e12110. Published 2020 Dec 16. doi:10.7759/cureus.12110
- Jáuregui B, Soto-Iglesias D, Penela D, et al. Follow-Up After Myocardial Infarction to Explore the Stability of Arrhythmogenic Substrate: The Footprint Study. JACC Clin Electrophysiol. 2020;6(2):207-218. doi:10.1016/j.jacep.2019.10.002
- Jegatheeswaran A, Devlin PJ, Williams WG, Brothers JA, Jacobs ML, DeCampli WM, Fleishman CE, Kirklin JK, Mertens L, Mery CM, Molossi S, Caldarone CA, Aghaei N, Lorber RO, McCrindle BW. Outcomes after anomalous aortic origin of a coronary artery repair: A Congenital Heart Surgeons’ Society Study. J Thorac Cardiovasc Surg. 2020 Sep;160(3):757-771.e5. doi: 10.1016/j.jtcvs.2020.01.114. Epub 2020 Apr 13. PMID: 32800265.
- Molossi S, Agrawal H, Mery CM, Krishnamurthy R, Masand P, Sexson Tejtel SK, et. al.: Outcomes in anomalous aortic origin of a coronary artery following a prospective standardized approach. Circ Cardiovasc Interv 2020; 13: pp. e008445.
- Nees SN, Flyer JN, Chelliah A, et al. Patients with anomalous aortic origin of the coronary artery remain at risk after surgical repair. J Thorac Cardiovasc Surg. 2018;155(6):2554-2564.e3. doi:10.1016/j.jtcvs.2017.12.134
Case prepared by:
Madhusudan Ganigara, MD
Editorial Team, Cases of SCMR
Division of Cardiology, Department of Pediatrics
The University of Chicago & Biological Sciences
5841 S. Maryland Avenue, Chicago, IL 60637







