Chaitanya Madamanchi MD, Michael Steigner MD, Raymond Kwong MD, MPH
Brigham and Women’s Hospital
Boston, Massachusetts, USA
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Clinical History: A 41-year-old man with nonischemic cardiomyopathy (Exercise Single Photon Emission Computed Tomography thirteen years prior revealed no perfusion abnormalities and LVEF 44%) presented with fever, myalgias, abdominal pain, and shortness of breath. CT Abdomen/Pelvis with Contrast was performed revealing no acute abnormalities in the abdomen but was notable for focal peripheral consolidation in the lungs (Image 1). The patient was treated for community-acquired pneumonia with ceftriaxone and prescribed a course of azithromycin upon discharge. He presented again one week later after having two syncopal episodes. Labs on admission were notable for leukopenia (WBC 3.56 K/uL, Ref 4.0-11.0 K/uL), elevated CRP 44.2 mg/L (Ref 0-8 mg/L), high sensitivity Troponin T 100 ng/L (Ref 0-14 ng/L). SARS-COV 2 PCR from nasopharyngeal swab was positive. ECG revealed normal sinus rhythm with occasional premature ventricular contractions with Q waves and T wave inversions in inferior leads (Image 2). An ischemic evaluation was pursued with coronary CTA which revealed no coronary plaque or stenosis but was notable for myocardial thinning involving the basal and mid inferior wall of the left ventricle (Image 3).

Image 1: Chest CT scan showing bilateral pulmonary consolidations (red arrows)

Image 2: Electrocardiogram showing inverted T-waves in inferior leads and ventricular ectopy
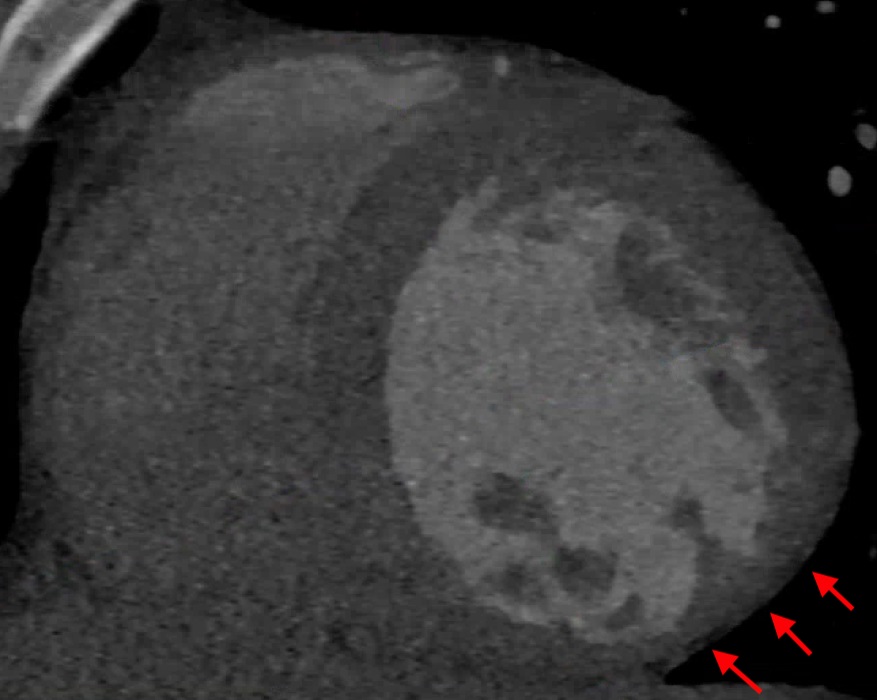
Image 3: CT Coronary angiogram demonstrating inferolateral myocardial wall thinning (red arrows)
CMR Findings: Cardiac MRI was obtained to evaluate for acute myocarditis. Steady State Free Procession cine images revealed mildly dilated LV with moderately decreased global systolic function with LVEF 33% and dyskinesis of the inferolateral wall (Movie 1). T2 weighted imaging and T2 mapping did not reveal any edema (Image 4). There was extensive, epicardial late gadolinium enhancement (LGE) involving the entire anterior, inferior, and lateral walls, and mid anteroseptal wall (Image 5).

Movie 1: SSFP cine images showing dilated left ventricle, dyskinesis of inferolateral wall and decreased global systolic function

Image 4: T2 weighted image with semiquantitative analysis showing a mean global myocardial T2 signal of 40 msec.

Image 5: Late enhancement imaging with epicardial enhancement involving the anterior, inferior, lateral and mid septal walls
Conclusion: Overall, these CMR findings are consistent with cardiomyopathy with a non-ischemic pattern of fibrosis. Genetic testing would be a helpful next step in the evaluation of this cardiomyopathy. There is no evidence of acute myocardial edema based on T2 weighted imaging or T2 mapping. This case illustrates a part of the spectrum of clinical scenarios for which CMR is requested during the COVID-19 pandemic. CMR can evaluate the acuteness and etiology of cardiomyopathy or suspected acute coronary syndromes in patients presenting with cardiac symptoms suspected to be related to COVID infection.
Goal-directed medical therapy for heart failure was initiated including beta-blocker and ACE inhibitor. The patient was discharged with a wearable external defibrillator and was then readmitted a few days later after presenting with multiple episodes of monomorphic ventricular tachycardia requiring electrical cardioversion. He subsequently underwent implantation of dual-chamber ICD for secondary prevention of sudden cardiac death and was discharged on amiodarone for ventricular tachycardia. ICD was interrogated 3 weeks later without any evidence of recurrent arrhythmias.
Case Prepared by:
Kevin Steel, DO, FACC, FSCMR
Editor, COVID-19 Case Collection





