Izabela Warchoł, Marcin Książczyk, Andrzej Lubiński
Department of Interventional Cardiology and Cardiac Arrhythmias, Medical University of Lodz, Lodz, Poland
Clinical History: A 74 year old man with a recent history of normal left ventricular ejection fraction of 55% was admitted to the hospital due to hemodynamically unstable new onset ventricular tachycardia (VT) lasting 12 hours (Figure 1). After unsuccessful self administration of metoprolol, 200 mg orally, arrhythmia was managed with electrical cardioversion. Subsequently, symptomatic bradycardia and hypotension were observed.
The patient did not present with fever or any symptoms of respiratory infection. The patient had a previous history of atrial fibrillation, catheter ablation performed 3 times, arterial hypertension, type 2 diabetes, and hypothyroidism. As a medical professional, the patient might have been exposed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The patient underwent coronary angiography, which revealed no obstructive coronary artery disease. Due to third degree atrioventricular block, a temporary transvenous pacemaker was inserted successfully.
On the following day, the next episodes of VT occurred. Serum electrolytes and thyroid hormone levels were within normal limits. Overdrive pacing with a rate of 95 pulses per minute, magnesium infusion, and intravenous amiodarone stabilized the rhythm. On the third day of hospitalization, the temporary pacemaker was removed, and follow up examination did not reveal any VT recurrence.
Laboratory findings were as follows: neutrophil-lymphocyte-ratio (NLR) higher than 3 (normal range 1-3), elevated levels of high-sensitivity cardiac troponin T, from 72 to 102 ng/l (reference range: <14 ng/l), dynamically evolving C‑reactive protein levels, from 1.2 mg/l to 1.8 mg/l and 94 mg/l (reference range <6 mg/l), elevated levels of N‑terminal fragment of the prohormone brain natriuretic peptide, 2451 ng/l (reference range <125 ng/l), lactic acid dehydrogenase, 369 U/l (reference range, 80–240 U/l), D‑dimers, 1.39 mg/l (reference range <0.5 mg/l), but procalcitonin levels (reference range <0.05 ng/ml) were normal.
Due to suggestive laboratory results, particularly in the light of the coronavirus disease 2019 (COVID‑19) outbreak, a reverse transcription–polymerase chain reaction (RT-PCR) test for SARS‑CoV‑2 was performed on the sixth day of hospitalization and yielded a positive result. Consequently, the patient received a single 500‑mg dose of azithromycin and a single 75‑mg dose of oseltamivir. On day 7, he was transferred in good general condition to a COVID‑19 specialized hospital for further treatment. On day 17, the patient’s pharyngeal swab specimen was still positive for SARS‑CoV‑2 after a repeat RT-PCR test, and the patient still had no respiratory symptoms.
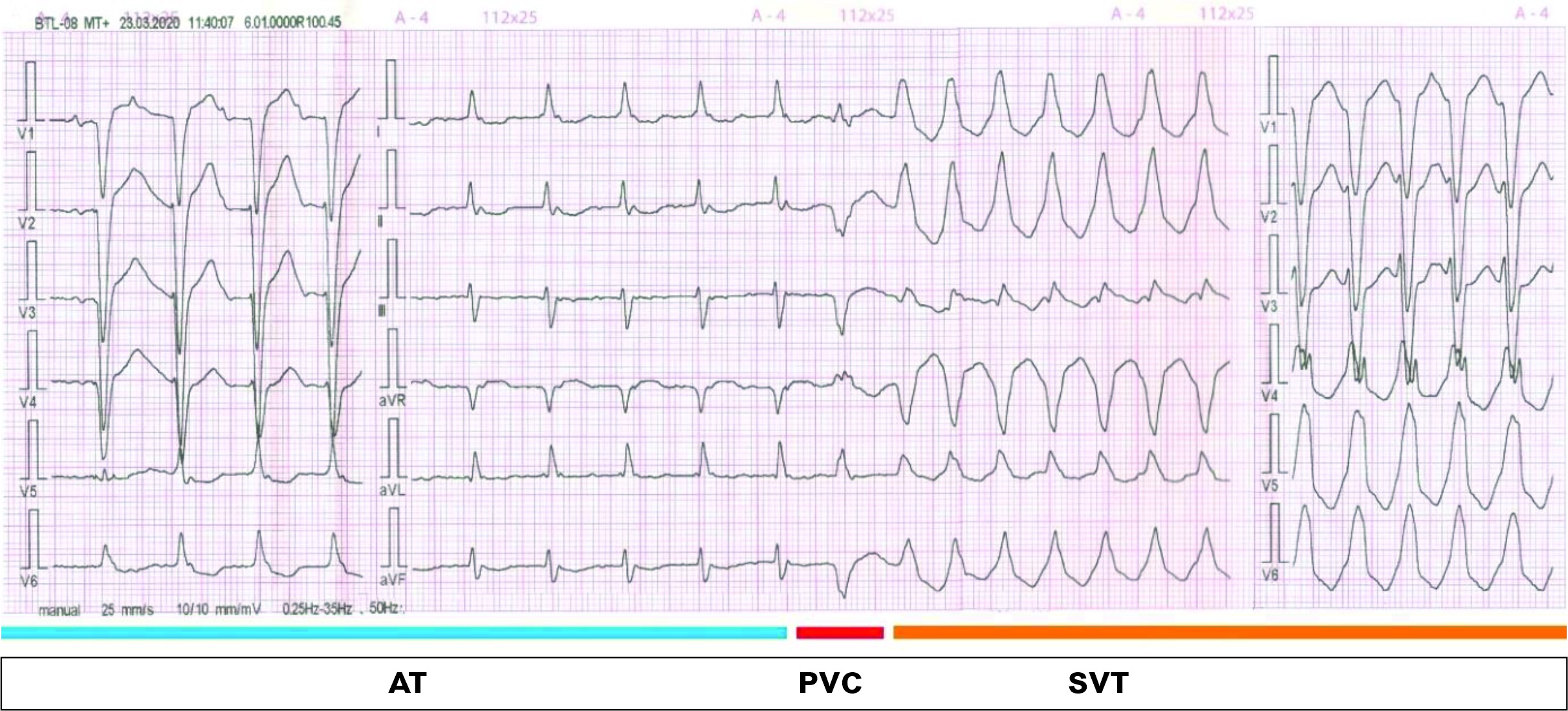
Figure 1. Twelve lead electrocardiogram with development of sustained ventricular tachycardia.
CMR Findings: Cardiac magnetic resonance imaging, performed with a 1.5 Tesla scanner, revealed left atrial enlargement and global left ventricular hypokinesia with ejection fraction of 20% (Movie 1 – 2). The T2‑weighted sequence did not show myocardial edema (Figure 2A – 1C). In contrast, imaging with the use of late gadolinium enhancement demonstrated a large, patchy, and linear nonischemic pattern of fibrosis localized subepicardially and intramurally in the basal and mid‑cavity segments of the inferior and inferolateral wall and in the apical segments of the inferior wall (Figure 2D – 1F, 3). T1 and T2 mapping were not available.
Movie 1. Two and four chamber cine SSFP with left atrial dilation and severely decreased left ventricular systolic function
Movie 2. Short axis stack cine SSFP with severely decreased left ventricular systolic function.

Figure 2. A-C: T2 weighted short axis stack reveals no evidence of myocardial edema. D-F: Myocardial delayed enhancement short axis stack reveals mid myocardial and epicardial late gadolinium enhancement of the basal and mid segments of the inferior and inferolateral wall and apical segments of the inferior wall (white arrows).
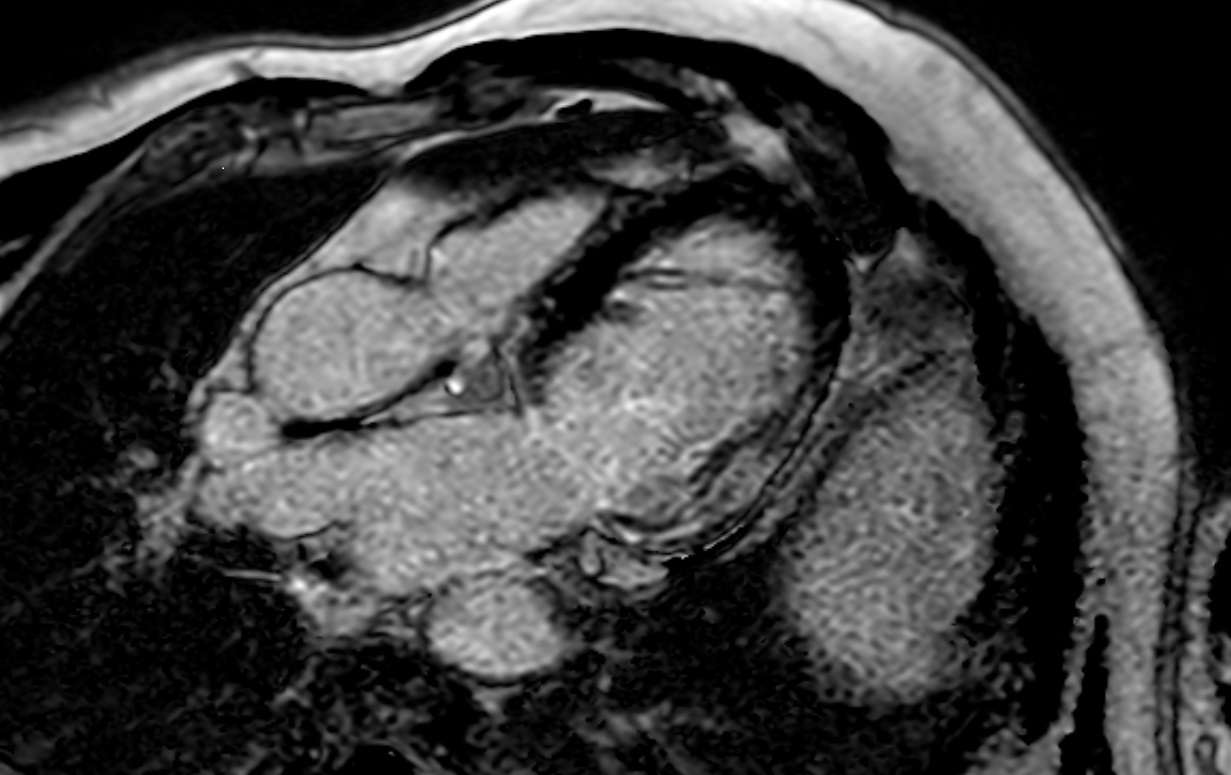
Figure 3. Off axis four chamber myocardial delayed enhancement image with mid to epicardial late gadolinium enhancement of the basal to mid inferolateral wall.
Conclusion: As shown in this case, SARS‑CoV‑2 may cause, apart from COVID‑19 related pneumonia, acute myocardial injury meeting diagnostic criteria for clinically suspected myocarditis. The emerging outbreak of COVID 19 was declared a pandemic by the World Health Organization on March 11, 2020. Even though respiratory tract signs mostly characterize the clinical course of SARS CoV 2 infection, cardiac complications, such as myocarditis, may also occur alone.
An ICD was considered for this patient, but a decision was postponed in the acute phase of myocarditis to allow left ventricular systolic function recovery. A LifeVest wearable defibrillator was not available. Follow-up echocardiogram after discharge showed improvement in left ventricular systolic function with an LVEF of 37%.
Published with permission from Polish Archives of Internal Medicine.
Case Prepared by:
Jason N. Johnson, MD MHS
Editor, COVID-19 Case Collection
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center







