Diego Chango-Azanza, Mónica Chapa, Sandra Rosales-Uvera
National Institute of Medical Sciences and Nutrition ¨Salvador Zubirán¨, Mexico City, Mexico
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Clinical History:
A 29-year-old woman was admitted for palpitations and fatigue. One month prior to admission she had an upper respiratory infection characterized by cough, fever, and muscular pain. At that time she did not seek medical attention and only took pain relievers. One week after the initial onset of symptoms she developed mild diffuse chest pain and palpitations that persisted for two weeks. The 12 lead electrocardiogram showed sinus rhythm without any ST and T wave abnormalities and the presence of frequent monofocal premature ventricular contractions (PVCs) (Figure 1). Labs on admission were notable for mild elevated type B natriuretic peptide 144 (Ref 0-100 pg/ml) and normal troponin I US 0.1 pg/ml (Ref 0-15pg/ml), CK-MB 0.5 ng/ml (Ref 0-3,4ng/ml) and D-dimer 191 ng/ml (Ref 0-250ng/ml). SARS-CoV-2 PCR from nasopharyngeal swab was negative. In addition, she was with IgM-negative and IgG-positive for SARS-CoV-2 related prior infection.

Figure 1: Twelve lead electrocardiogram with sinus rhythm without ST–T abnormalities and frequent premature ventricular contractions.
CMR Findings:
CMR at 1.5 T was performed one month after the onset of symptoms. There were no specific pulmonary abnormalities with no pleural or pericardial effusion (Movie 1). Image quality was affected due to the presence of frequent ventricular arrhythmia throughout the study. Long axis views of both ventricles showed normal ventricular volumes, wall thickness, ventricular mass, and ejection fraction. (Movies 2,3). The left and right ventricular volumes were as follows: LVEDVi 40.1 ml/m2, LVESVi 14.6 ml/m2, LVEF 63%, RVEDVi 38.2 ml/m2, RVESVi 17.2 ml/m2, RVEF 55%. Myocardial edema was absent on T2 short tau inversion recovery images (Figure 2) with the ratio between myocardial/body muscle normal at 1.8 (Normal value <2). Late gadolinium sequences showed extensive, patchy intramyocardial enhancement affecting the mid anterior and mid to apical anteroseptal walls. (Figure 3, Movie 4).

Movie 1: Axial single-shot SSFP images without evident pulmonary consolidations neither pleural nor pericardial effusion.
Movie 2: Cine SSFP left ventricle four-chamber and three-chamber view showing normal LV volumes, wall thickness, and ejection fraction without wall motion abnormalities.
Movie 3: Cine SSFP short-axis stack and left ventricle two-chamber views showing normal LV volumes, wall thickness, and ejection fraction without wall motion abnormalities.
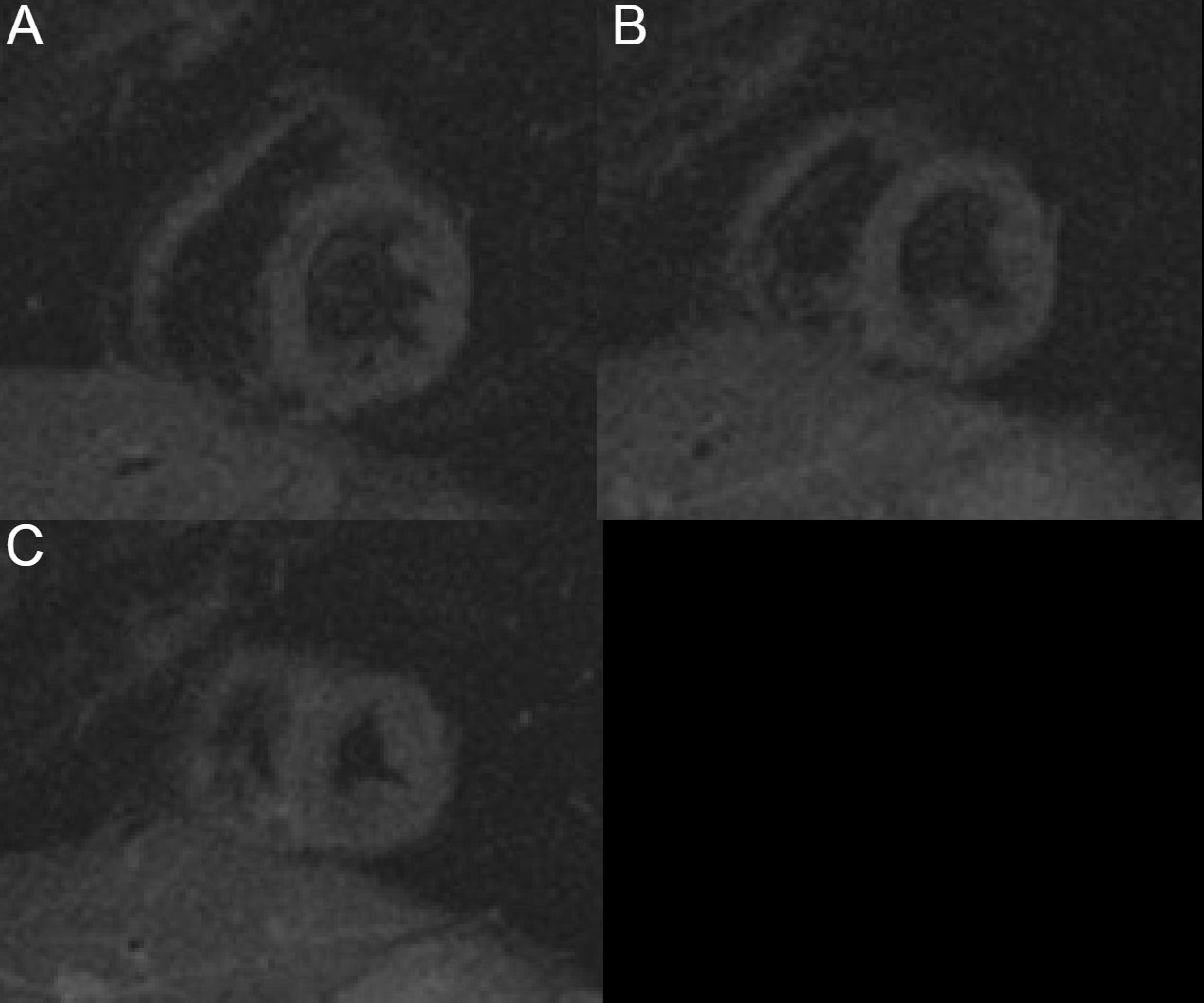
Figure 2: Short tau inversion recovery (STIR) basal to apex short-axis images without any hyperintensity regions indicating absent myocardial edema.

Figure 3: Four chamber, two-chamber, three-chamber, and middle short-axis myocardial late gadolinium enhancement images show likely, patchy mid-late gadolinium enhancement affecting the mid anterior and mid to apical anteroseptal walls. No pericardial enhancement present.

Movie 4: Late gadolinium enhancement short-axis images from basal to the apex. Showing likely, patchy intramyocardial enhancement affecting the mid anterior and mid to apical anteroseptal walls.
Conclusion:
The patient was discharged five days after hospital admission with antiarrhythmic medication and close follow-up. A future CMR is planned in 6 weeks for surveillance of myocardial fibrosis and its relationship with ventricular arrhythmia. This case provides evidence of CMR sequelae of likely prior myocardial inflammatory involvement possibly secondary to SARS-CoV-2 infection that has been described in some patients. The absence of edema with the persistence of LGE may not be reversible. LGE images could have some difficulties during acquisition and a low inversion time can suggest hyperenhancement even in the absence of fibrosis and need it to be confirmed in imaging surveillance. Additionally, further investigations are required to clarify these findings and clinical relevance in future arrhythmic events of these patients.
Case Prepared by:
Jason N. Johnson, MD MHS
Editor, COVID-19 Case Collection
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center







