Jason Craft MD1, George Jojo Punnakudiyil MD1; Viraj Jayam1, Farah Shams MD2
St Francis Hospital, Dematteis Research Center1, Greenvale, NY
Infectious Diseases2, St Francis Hospital; Roslyn, NY
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Click here for PubMed Reference to Cite this Case
Clinical History:
A 52 year old male with no significant past medical history had been having intermittent fevers, chills, dry cough, left scapular and pleuritic chest pain associated with exertional dyspnea for more than one month. He had three prior hospitalizations since his symptoms began. He was initially diagnosed with right middle lobe pneumonia when hospitalized at an outside facility, treated with antibiotics and had subsequent mild symptom relief on discharge. He was hospitalized twice again for the same complaints at the outside institution. CT angiography of the chest was done on both admissions and showed no pulmonary embolism or pneumonia, but revealed a pericardial effusion and small left pleural effusion. His severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) PCR test was negative but his SARS-CoV-2 antibody was positive. He was given a short course of antibiotics during one of those hospitalizations without benefit.
Despite previous treatments he again had a relapse of symptoms and was admitted to our facility. Social history revealed his mother had contracted SARS-CoV-2 and died from coronavirus disease 2019 (COVID-19) pneumonia about 2 months prior to his presentation. He was febrile to 102.7F on admission with a mildly elevated white blood cell count of 11.5K. Initial blood work showed elevated inflammatory markers (CRP 143 mg/L, ESR 40 mm/hr) and mild elevation of troponins to 0.1 ng/mL. Chest X ray showed clear lungs and CT scan of chest did not show pneumonia. Blood cultures remained without growth. ECG showed sinus tachycardia with non-specific ST abnormalities in leads V4-V6 (Figure 1). SARS-CoV-2 PCR was negative, however SARS-CoV-2 antibody was positive again.
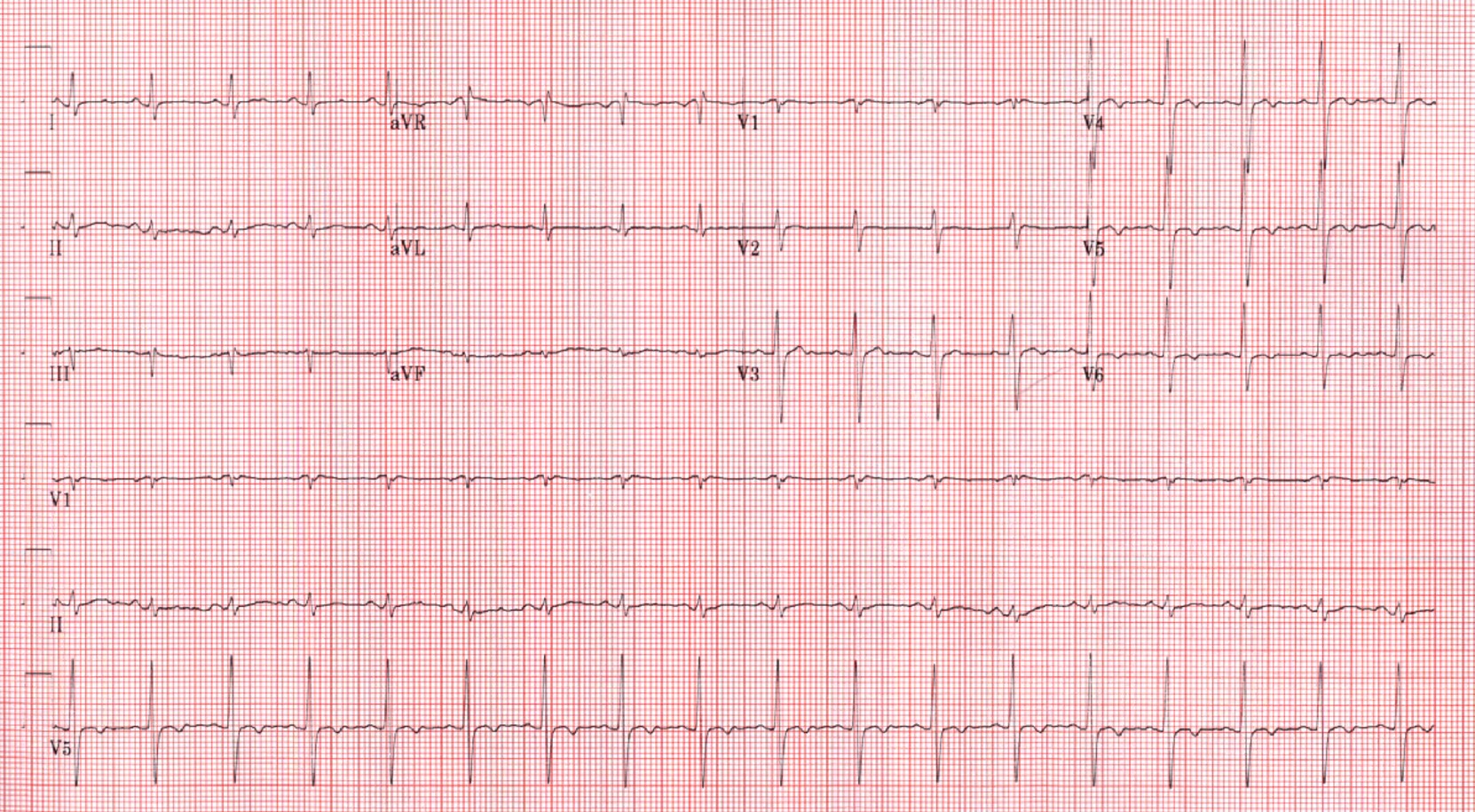
Figure 1. Admission 12 lead ECG demonstrating sinus tachycardia and non-specific ST abnormalities.
Transthoracic echocardiography (TTE) demonstrated moderately reduced left ventricular EF of 35-40% with diffuse moderate hypokinesis, trivial circumferential pericardial effusion, and small left sided pleural effusion. CT coronary angiography was done to exclude obstructive coronary artery disease and revealed no significant coronary artery stenosis. However, there was notable pericardial thickening measuring about 0.6cm but absent pericardial calcification. The patient was referred for CMR for further evaluation.
CMR Findings:
Biventricular systolic function was low normal with a LVEF of 52% and RVEF of 50% (Movies 1-3). There was no evidence of myocardial inflammation or edema as manifested by normal myocardial T2 mapping values (Figure 2). Native T1 values were within reference range for our institution, measuring 988 ms, averaged over 8 SAX segments (Figure 3). Furthermore, the myocardial extracellular volume was 24%. However, on T2 weighted STIR, high signal intensity and marked thickening (measuring 0.5 cm) of the pericardium was present (Figure 4). There was also extensive pericardial late gadolinium enhancement (Figure 5). There was no mid wall or epicardial myocardial delayed enhancement to suggest sequelae of previous myocarditis. A trivial pericardial effusion was present with no evidence of interventricular dependence by free-breathing real time cardiac cine (Movies 4-5).
Movie 1: Four chamber bSSFP cine demonstrating low normal biventricular systolic function and marked pericardial thickening with moderate left pleural effusion.
Movie 2: Short axis bSSFP cine demonstrating low normal biventricular systolic function and marked pericardial thickening.
Movie 3: Three chamber bSSFP cine demonstrating low normal biventricular systolic function and marked pericardial thickening and moderate left pleural effusion.
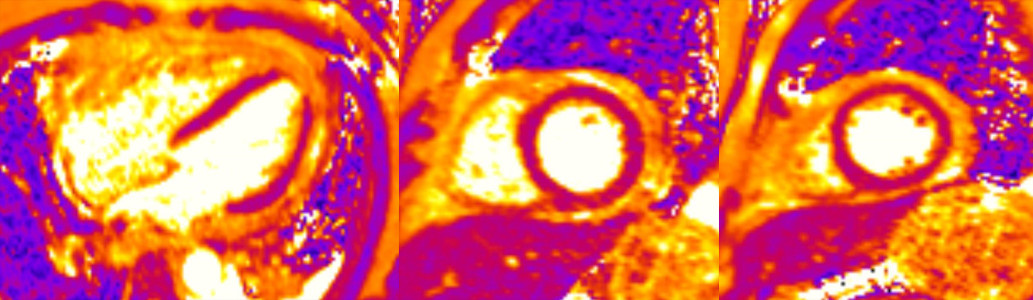
Figure 2. Four chamber and basal and mid short axis T2 maps demonstrating no evidence of myocardial inflammation or edema.
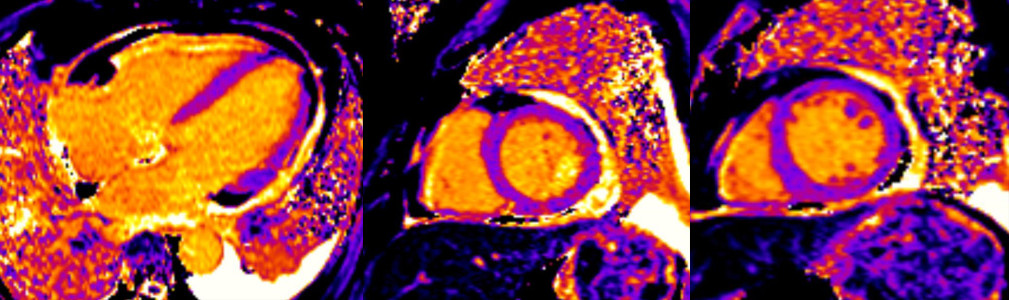
Figure 3. Four chamber and basal and mid short axis native T1 maps with values within reference institutional ranges.
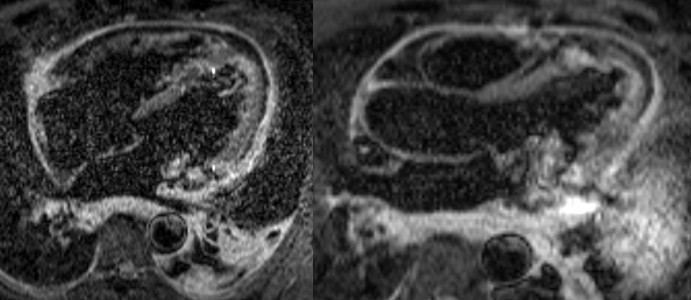
Figure 4: Four and three chamber T2 weighted STIR demonstrating pericardial thickening and inflammation/edema.
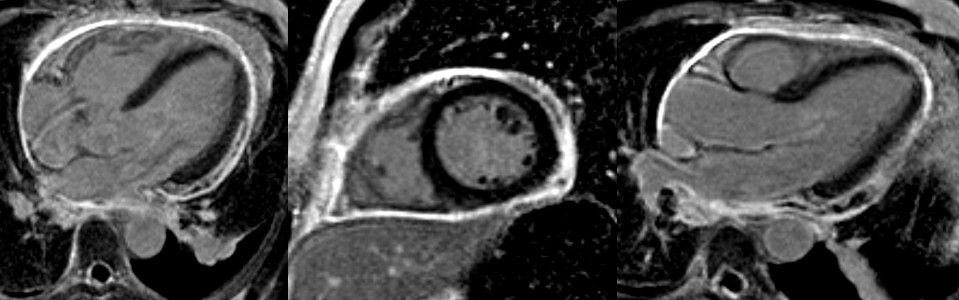
Figure 5: Four chamber, short axis, and three chamber post contrast IR-GRE demonstrating marked delayed enhancement of the pericardium.
Movie 4. Real time four chamber cine demonstrating no evidence of interventricular dependence.
Movie 5. Real time mid short axis cine demonstrating no evidence of interventricular dependence.
Conclusion:
With suspected COVID-19 related pericarditis identified, the patient was treated with colchicine. He was not treated with high dose NSAIDS or aspirin. He had no further fever while admitted and symptomatically improved at the time of discharge. SARS-CoV-2 antibody being positive and social history of his mother having suffered from COVID-19 supports exposure to COVID-19. A negative SARS-CoV-2 PCR supports no active infection. The patient’s symptoms were isolated, which excluded the diagnosis of multisystem inflammatory syndrome in adults (MIS-A). The patient had full recovery after treatment with Colchicine and upon follow up 6 months later, he has remained asymptomatic and active.
Perspective:
The importance of using CMR despite TTE findings in this population is highlighted by our case. The patient’s TTE mistakenly demonstrated a LVEF of 35-40%, leading to inappropriate therapy with metoprolol and losartan for “acute systolic CHF”. Of note, the patient’s brain natriuretic peptide was 48 pg/mL with a non-obese BMI (26 kg/m2). The patient possibly had recurrent post infectious COVID-19 pericarditis as manifested by his symptom course and persistently positive SARS–CoV-2 antibody. He is also at high risk for further recurrence as manifested by pericardial late gadolinium enhancement (1). In the above ways, CMR drastically altered patient management.
References:
Case Prepared by:
Jason N. Johnson, MD MHS
Editor, COVID-19 Case Collection
Le Bonheur Children’s Hospital, University of Tennessee Health Science Center







