Author: Ibrahim M. Saeed, MD, FACC, FSCMR

As a physician who has seen a presentation of nephrogenic systemic fibrosis (NSF) in clinic, I am especially sensitive to the risks associated with gadolinium-based contrast agents (GBCAs) in the setting of kidney disease. And yet as clinicians, we are all too familiar with the need to balance that with the definitive diagnostic testing that MRI provides. How do we educate our patients and our referring colleagues given the paucity of recent data with newer Group II agents and the fear of a future life-threatening event?
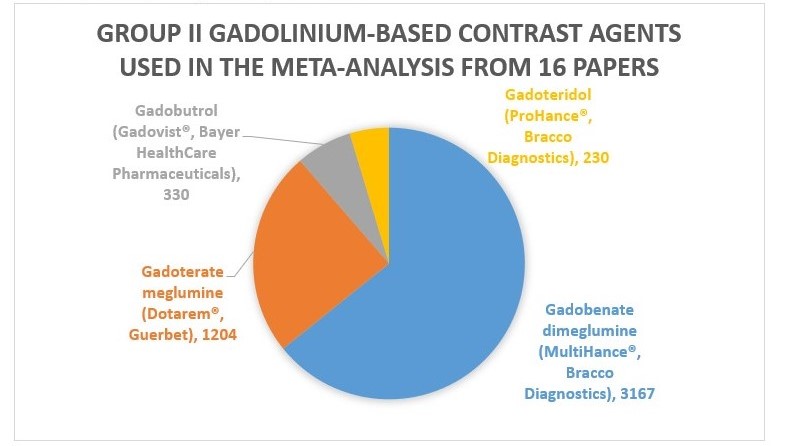
A recent meta-analysis by Woolen and colleagues in the December 9, 2019 issue of JAMA Internal Medicine attempts to provide us with that data. After pooling data from 4931 patients from sixteen studies, they concluded that the risk of developing NSF is likely less than 0.07% (upper bound 95% CI risk estimate). The agents specifically used were:
The authors compare this risk to an allergic reaction to modern low-osmolality iodinated contrast (0.04%); and also bring up the risk of withholding the potential benefit of diagnostic testing.
While there remains a black box warning by the US Food and Drug Administration indicating that all GBCAs are contraindicated if the estimated glomerular filtration rate is less than 30 mL/min/1.73m²; several societies support the use of indicated low-risk GBCAs in this setting, including the American College of Radiology. Furthermore, it is their opinion and that of the invited commentary supporting this paper, that a written consent is not necessary but rather informed counseling.
Further caveats by the commentators include using the lowest possible dose, avoiding repeated exposures, and those on hemodialysis receive this treatment shortly after GBCA exposure.
The commentary also argues that when contrast-enhanced MRI is the superior imaging modality to pursue it without diagnostic delay. Given the not-uncommon frequency of cardiovascular disease and renal disease, as practitioners of cardiovascular magnetic resonance, we would do well to continue to advocate for our patients by educating our referral sources and patients. The authors should be commended for rigorous analysis.







