Hypertrophic cardiomyopathy (HCM) is the most commonly inherited cardiac condition, occurring in one in every 500 people within the general population. Hypertrophic cardiomyopathy occurs if heart muscle cells enlarge and cause the walls of the ventricles-usually the left ventricle-to thicken. The thickened heart muscle can make it harder for the heart to pump blood. The Society for Cardiovascular Magnetic Resonance (SCMR), a Society dedicated to improving cardiovascular health by advancing the field of cardiovascular magnetic resonance (CMR), brings education and awareness to HCM and how the use of cardiovascular magnetic resonance (CMR) can help to identify and treat the condition. The week of May 27 is recognized as Hypertrophic Cardiomyopathy Awareness Week.
“Hypertrophic cardiomyopathy is usually caused by abnormal genes that cause the heart muscle to grow thicker than normal,” said Dr. Mahi L. Ashwath, FACC, FASE, FSCMR, SCMR Committee Member. “Patients with hypertrophic cardiomyopathy also have an irregular arrangement of heart muscle cells-myofiber disarray- that can contribute to fatal arrhythmias in some people. The clinical expression of HCM is a spectrum. Most who have HCM have no signs or symptoms, and the disease doesn’t affect their lives, whereas others experience severe symptoms and complications including shortness of breath, chest tightness, an inability to exercise or serious arrhythmias. While prognosis is usually good, serious arrhythmias resulting in sudden cardiac death can occur. Accurate assessment of maximal wall thickness and scar detection by CMR can play an important role in the risk stratification of these patients. Regular check-ups with your physician can help quickly identify any cardiac related issues and also provide a recommendation of Cardiac MRI if and when it is needed.”
The main feature of hypertrophic cardiomyopathy is an excessive thickening of the heart muscle-hypertrophy literally means to thicken. The ventricle size often remains normal, but the thickening may block blood flow into and out of the left ventricle. If this happens, the condition is called obstructive hypertrophic cardiomyopathy.
Heart muscle may also thicken in individuals with prolonged high blood pressure, Fabry cardiomyopathy or prolonged athletic training. CMR is very useful in determining the cause of a patient’s hypertrophy and can confirm the diagnosis of HCM. It can correctly distinguish acquired hypertrophy from hypertension, athlete’s heart, or Fabry Cardiomyopathy from HCM, enabling appropriate requests for family screening.
Most HCM experts recommend Cardiac MRI in every patient with HCM for accurate diagnosis, assessment of wall thickness, exclusion of other etiologies for the hypertrophy, scar quantification and for prognostic assessment in HCM.
CMR is therefore indicated:
- To confirm the diagnosis, when suspected from family history, medical history, ECG and other imaging modalities
- To distinguish between HCM and other forms of hypertrophy and to confirm the diagnosis of HCM
- To evaluate for obstructive and non-obstructive hypertrophic cardiomyopathy
- For initial or subsequent evaluation of left/ right ventricular function, maximal wall thickness, and myocardial mass
- To assess extent and severity of late gadolinium enhancement (LGE), which corresponds to the scar in the heart
- To evaluate ‘burned out” HCM and subsequent heart failure
- For prognostic evaluation (maximal wall thickness, T1 relaxation times, scar quantification)
Major advantages of Cardiac MRI include the ability to image in any plane without body habitus limitations, excellent delineation of anatomic structures resulting from inherent high levels of contrast resolution and the ability to characterize and discriminate among tissues using their physical and biochemical properties. All these properties give Cardiac MRI an ability to image cardiac anatomy, cardiac function, high –resolution perfusion, viability, advanced blood flow analysis and inflammation/edema in 30-45 minutes. Cardiac MRI has been called as the “Noninvasive biopsy of the heart” in short.
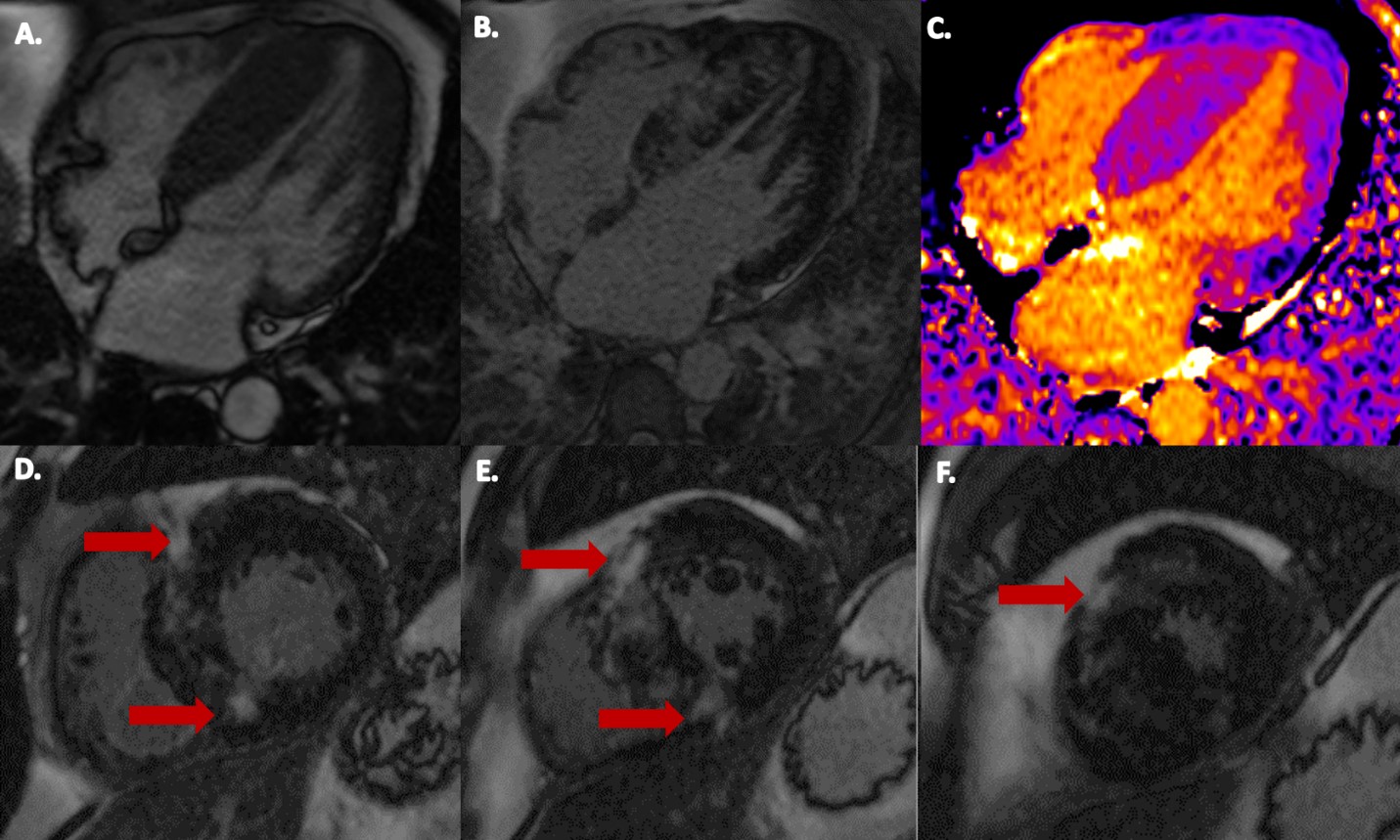
A. Steady state free precession (SSFP) imaging of 4-Chamber view of hypertrophic cardiomyopathy (HCM) measuring 27 mm (Normal <12 mm) in the mid septum. B. Late gadolinium enhancement (LGE) imaging of 4-Chamber view of HCM with basal to apical inferoseptal LGE. C. Native myocardial T1 map of 4-Chamber view of HCM. D. Basal short-axis (SAX) view with septal LGE including superior and inferior right ventricular insertion LGE (red arrows). E. Mid SAX view with septal LGE including superior and inferior right ventricular insertion LGE (red arrows). F. Apical SAX view with superior right ventricular insertion LGE (red arrow).







