Case from: L Lee, J Scales, D Pauly, R Shifrin, G Cooper.
Institute: University of Florida. Cardiac Imaging Group. Gainesville, Florida
Clinical history: A 46-year-old man with history of Hodgkin’s lymphoma treated with radiation 20 years ago. Four years previously he had undergone pleurodesis for recurrent pleural effusions. He recently developed worsening dyspnea, lower extremity edema, and ascites. At another facility, he was treated initially for interstitial lung disease with bronchodilators without improvement of his symptoms. He was referred to our center for further evaluation.
Physical Examination: VS: BP 120/82, HR 91. He was a thin, ill appearing male with nonicteric sclerae. His jugulovenous pressure15 cm water. Lungs were clear bilaterally.
His heart rhythm was regular. There was an early diastolic sound, likely a pericardial knock. His liver edge was palpable at the costal margin. There was no peripheral edema
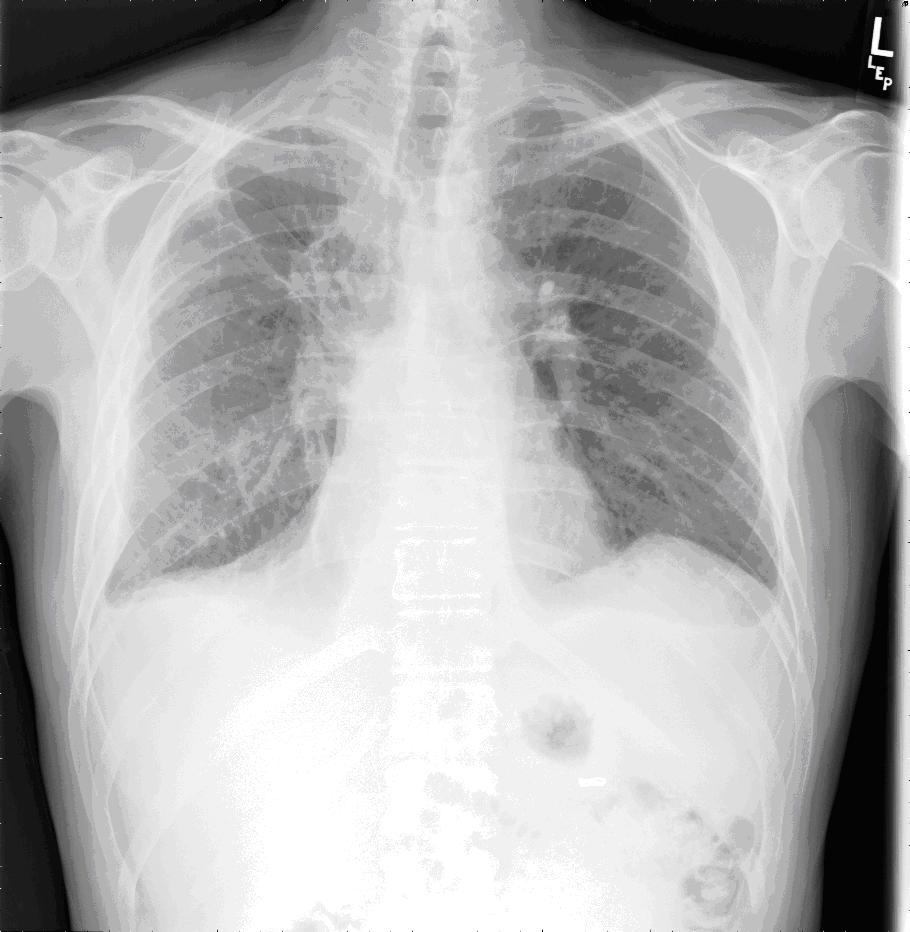
Chest x-ray: Changes in the perihilar and paramediastinal region consistent with prior mantle irradiation for Hodgkin’s lymphoma. There is bilateral pleural scarring versus small pleural effusions.

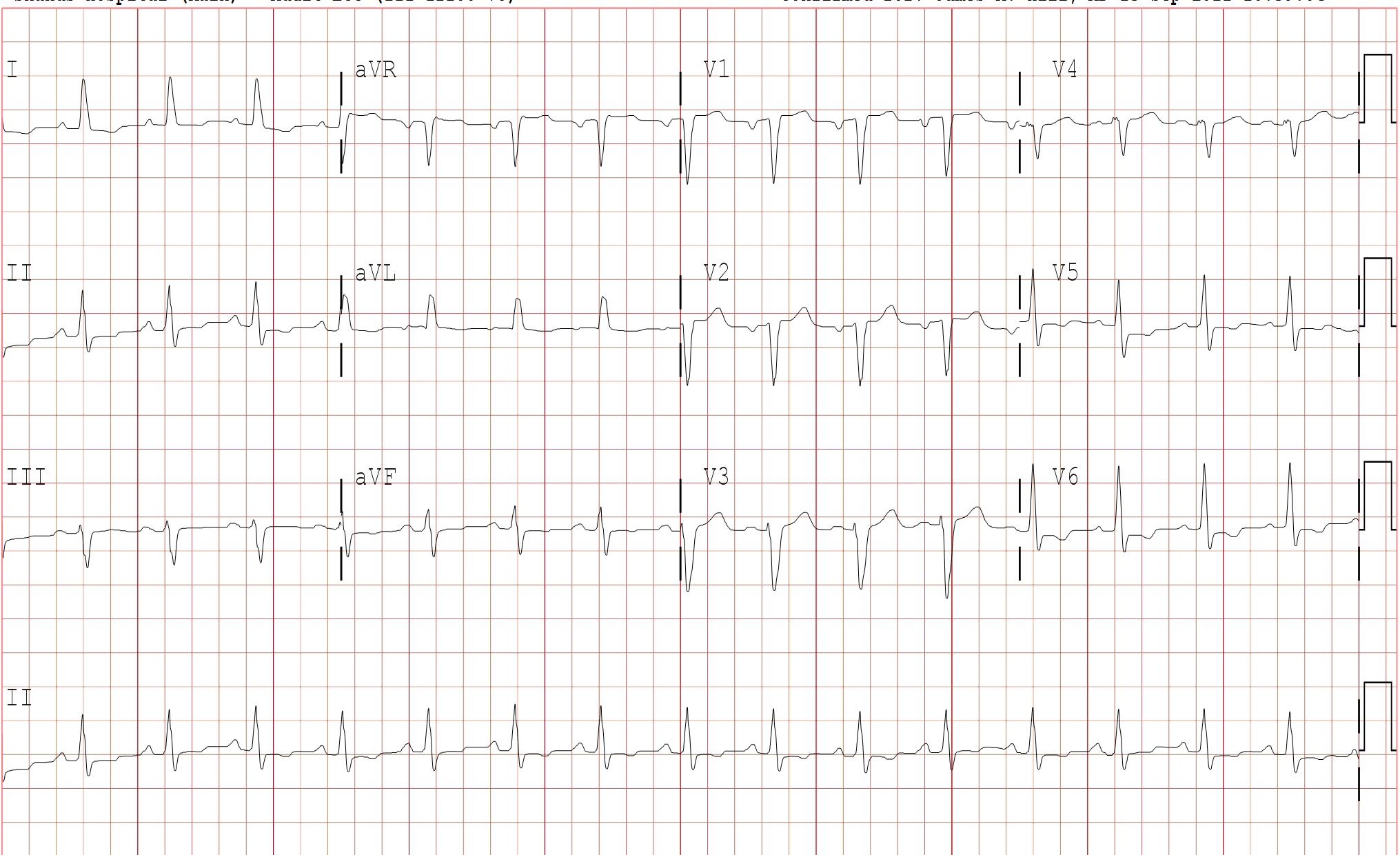
EKG: NSR, probable left atrial abnormality, non-specific IVCD, abnormal R wave progression, & ST-T wave changes
TTE: Done at another institution is said to have shown a normal EF (50%), mild mitral regurgitation, and mild pulmonary hypertension but no evidence of constriction.
CT: There is a ground-glass opacities within the right lower lobe which may represent an infectious or inflammatory process. In addition, there is a large left pleural effusion.. There are bilateral perihilar changes from radiation therapy, not significantly changed from the prior study. A moderate amount of ascites is present. There is no pericardial thickening or calcification. A small pericardial effusion is present
Cardiac Cath: Hemodynamic findings demonstrate: equalization of diastolic pressures with RA = 20 mmHg; RVEDP = 20 mmHg; LVEDP/PCWP = 25 mmHg
There was evidence of square-root sign on ventricular end-diastolic hemodynamics
Though not unequivocal, the simultaneous LV/RV hemodynamics are more consistent with constrictive physiology. While there is not classic respiro- phasic discordance of ventricular pressures, there was notable reduced RV pressure variation in the setting of marked LV pressure variation. Mild pulmonary hypertension – mean PA pressure 27 mmHg
Simultaneous LV and RV pressures are presented below.
CMR Findings: Localizers demonstrate a large left pleural effusion and ascites particularly notable surrounding the liver.

SSFP Cine: Numerous areas of adherent, thickened pericardium are demonstrated. The pericardial space is not seen and normal pericardial slippage is absent
Three Chamber SSFP Cine. In this view the pericardium thickness measures 5.4 mm.
Although septal bounce is evident in the breath hold sequences is accentuated by free breathing. (Top-BH, Bottom FB)
Myocardial tagging study: The tags persist with cardiac contraction. These changes are most evident in the inferior and posterior wall
Conclusions:
His Echocardiogram was not suggestive of constriction. The CT did not demonstrate pericardial calcification or thickening. Catheterization was felt to be suggestive for the diagnosis. The cardiac catheterization was the most convincing of the studies done prior to CMR with equalization of diastolic pressures but lacked respiro-phasic discordance. CMR in this case offered additional information and complimented the preliminary studies by confirming the clinical suspicion of constrictive physiology.
Key CMR features included abnormal pericardial slippage, reduced to absent pericardial space, an abnormal myocardial tagging study, septal “bounce”, and an immobile, adherent, thickened interface between the myocardium and pericardium.
Distinguishing constrictive physiology from restrictive physiology can be difficult. This is particularly true in patients with a history of radiation therapy, as both restrictive cardiomyopathy and constrictive pericarditis may occur concurrently.1 Furthermore, differentiating these two entities is important clinically as surgical pericardiectomy can provide relief of symptoms in many patients with constrictive pericarditis, while restrictive cardiomyopathy is managed medically.2
Pericardial thickening by CT without constriction may occur after acute pericarditis or cardiac surgery3,which have become more frequent causes of pericarditis than tuberculosis.1 Pericardial calcification in non-tuberculous pericarditis can be less prominent as well.1
The ratio of right ventricular to left ventricular systolic area during inspiration and expiration by cardiac catheterization has been found to be more reliable than traditional hemodynamic criteria. This was found to have a higher predictive accuracy (100% vs. <75%) in identifying patients with surgically proven constrictive pericarditis compared to conventional hemodynamic criteria.4
Echocardiography studies may also show evidence of respiro-phasic discordance but these studies may be limited by echocardiographic windows and narrow field of view, have limited tissue characterization, and are operator dependent.3
CMR evaluation permits both anatomic and physiologic assessment for constriction. Pericardial thickening (> 4 mm) is supportive of a diagnosis of constriction.3,5 Diastolic interventricular septal flattening or bounce on free breathing sequences may reveal the presence of ventricular interdependence characteristic of this disease. Similarly, tagged cine CMR may elegantly show tethering and adhesion of the thickened pericardium to the myocardium.6
CMR is a versatile and comprehensive modality for differentiating constriction from restriction and should not be considered the study of last resort.
References:
1. Bogaert J, Francone M. Cardiovascular magnetic resonance in pericardial diseases. J Cardiovasc Magn Reson 2009: 11:14.
2. Nishimura RA. Constrictive pericarditis in the modern era: a diagnostic dilemma. Heart 2001;86:619-623.
3.Rajiah P. Cardiac MRI: Part 2, pericardial diseases. Am J Roentgenol. 2011 Oct;197(4):W621-34..
4. Talreja DR, Nishimura RA, Oh JK, Holmes DR. Constrictive pericarditis in the modern era: novel criteria for diagnosis in the cardiac catheterization laboratory. J Am Coll Cardiol 2008;51:315-319.
5. Ariyarajah V, Jassal DS, Kirkpatrick I, Kwong RY. The utility of cardiovascular magnetic resonance in constrictive pericardial disease. Cardiol Rev 2009;17:77-82.
6. Kojima S, Yamada N, Goto Y. Diagnosis of constrictive pericarditis by tagged cine magnetic resonance imaging. N Engl J Med 1999;341-373-374.







