Cristina Conca1; Lidia Squadroni1; Stefania Battaglia2; Paola Bognetti1; Maurizio Marzegalli1; Alberto Roghi3; Maurizio Cariati2
Institute: 1. Department of Cardiology, San Carlo Borromeo Hospital, Milan, Italy; 2. Department of Radiology, San Carlo Borromeo, Milan, Italy; 3. Department of Cardiology, ,Niguarda Ca’Granda Hospital, Milan, Italy
Clinical history: A 52 year old asymptomatic male affected by hypertension and without other remarkable past medical history presented to the outpatients clinic for check-up. Electrocardiography revealed sinus rhythm with incomplete right bundle-brunch block and poor R-wave progression as a result of the leftward displacement of the heart (Figure 1).
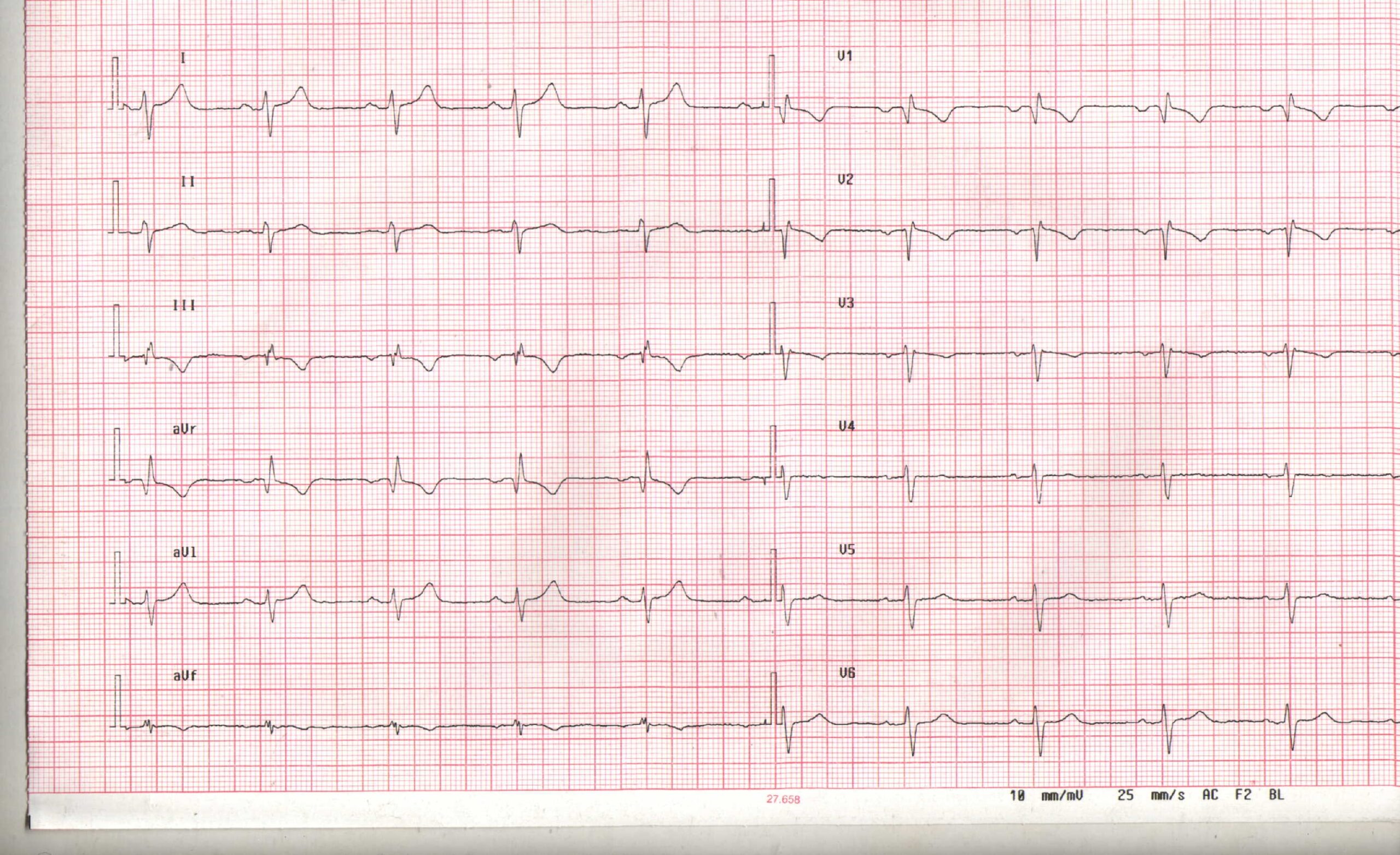
Figure 1: Electrocardiogram
The patient underwent Cardiac Magnetic Resonance (CMR) due to non diagnostic echocardiogram for inadequate acoustic window: the apical window was displaced more lateral than normal and echocardiographic findings were unusual due to deeper position and excessive systolic anterior movement of the heart. We presumed an absence of pericardium based on these results.
CMR Findings: The study was performed on a General Electric 1.5T scanner. CMR demonstrated leftward displacement of the heart into the left hemithorax with the left ventricular apex pointing posteriorly and with excessive mobility during cardiac cycle; biventricular volumes were mildly increased (LVEDVI/LVESVI = 93/36 ml/m2; RVEVI/RVESVI = 82/34 ml/m2), normal biventricular function (LVEF = 61%; RVEF = 66%), mild atrio-ventricular valve regurgitations and mild bi-atrial dilatations (area left atrium = 24 cm2; area right atrium = 26 cm2) were present; no other malformations of the heart were found (Movie 1).
Movie 1: Cardiac MRI, balanced steady-state free procession technique (b-SSFP) four, two and three chambers and short axis CINE stack
The pericardium is delineated only along the left atrial posterior wall and basal segment of right ventricle (Figure 2, arrowed, a-b).
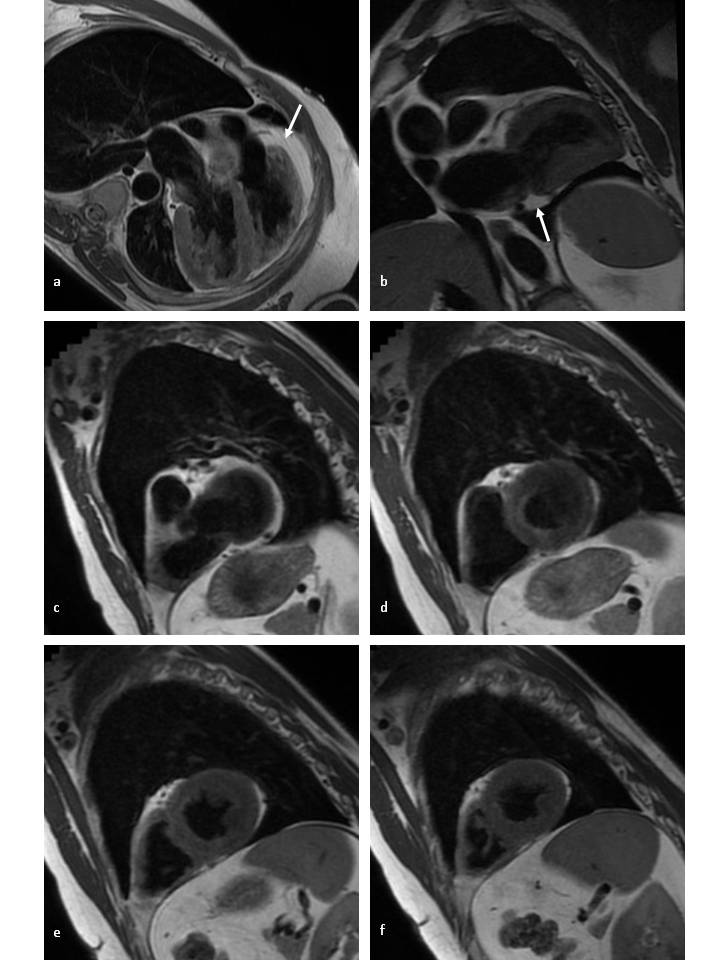
Figure 2: T1-weighted fast spin-echo CMR in axial view. a-b) long-axis and c-d-e-f) short axis at four different levels. The pericardium is noted by the white arrow.
No evidence of pericardial recesses were found in the transverse plane at three different levels throught the origin of the great vessels (Figure 3).

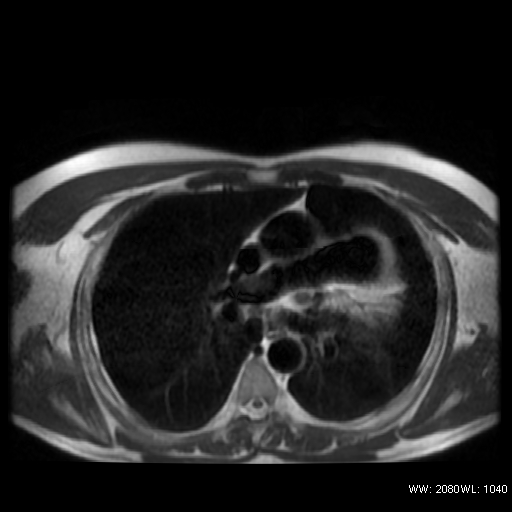

Figure 3: T1weighted FSE in the transverse plane, three different levels, through the origin of the great vessel
Conclusion: Taking all the imaging results into consideration, the patient was presumed to have partial absence of the pericardium. The patient is currently asymptomatic, we scheduled a clinical follow-up to evaluate potential complications.
Perspective: Congenital absence of the pericardium is a rare malformation and it always results from an abnormal embryonic development (originates from premature atrophy of the common cardinal vein, which impedes its normal closure). The agenesis is more common on the left side (70%) than on the right side (4%) or the inferior side (17%)1. It is more often partial than total (9%) and may be associated with other malformations, particularly malformations of the heart (bicuspid aortic valve, mitral stenosis, ductus arteriosus, atrial septal defect, bronchogenic cyst, hiatus hernia, diaphragmatic hernia and pectus excavatum)2.
The clinical presentation is variable. Patients with complete absence of the pericardium are generally asymptomatic; patients with partial absence of the pericardium, on the other end, are at risk from possible symptomatic herniation.
Although transthoracic and transesophageal echocardiography are not the techniques of choice for the direct visualization of the pericardium, they can detect nonspecific signs such as anomalous position and motion of the heart, paradoxic septal motion, hypermobility of the posterior wall and anterior displacement of the left ventricle in systole. MRI is the technique of choice due to its high spatial resolution and tissue chracterization and to the ability related to tomographic imaging. It enables the pericardium to be seen as a fine structure 1-2 mm thick situated between the epicardial and the mediastinal fat; MRI can also reveal situations involving potential risk, such as chamber herniation through partial defect or annular constriction of the ventricular myocardium, which is the most dangerous of these situations.
The diagnosis of a pericardial defect is not always straightforward also on CMR, since in normal conditions the pericardium over the lateral side of the left ventricle, corresponding to the most frequent location of pericardial defects, is usually not well depicted because of a paucity of surrounding fat3.
The preaortic and retroartic recesses of the pericardium can be identified in 67-100% of the cases, these differences of percentage are due to variability of the amount of serous fluid among individuals and may explain, at least in part, why in some patients, sinuses or recesses may or may not be seen. The sensitivity of SE-MRI for visualising the pericardium varies from only 61% for the pericardium over the freewall of the LV to 100% over the region of the RV(4).
The diagnosis of pericardial agenesis usually relies on other signs such as an abnormal location of cardiac structures with excessive levo-rotation or cardiac indentation at the location of the defect (5-6), but is not always easy to differentiate partial versus total agenesis of pericardium. MRI can not always delineate the entire pericardium, and so the full extent of defect could not be confirmed without performing a thoracotomy.
Complete or unilateral agenesis does not require prophylactic intervention because these conditions do not involve any risks. Both symptomatic and asymptomatic partial agenesis that appears to involve the risk of ventricular strangulation on imaging techniques requires more careful follow up than complete absence of the pericardium, although there is no clear evidence of benefit of prophylactic surgery of these patients.
References:
- Amplatz K, Moller JH (1993) radiology of congenital heart disease. Mosby Year Book, St Louis, Mo, USA
- Lorell BH, Braunwald E (1988) Pericardial disease. In: Braunwald E (ed) Heart disease, a textbook of cardiovascular medicine. Saunders, Philadelphia, pp 1484-1485
- Gutierrez FR, Shackelford GD, McKnight RC, Levitt RG, Hartmann A. Diagnosis of congenital absence of left pericardium by MR imaging. J Comput Assist Tomogr 1985;9:551-553
- Sechtem U, Tscholakoff D, Higgins CB. MRI of the abnormal pericardium. Am J Roentgenol 147:239-244
- Abbas AE, Appleton CP, Liu PT, Sweeney JP. Congenital absence of the pericardium: case presentation and review of literature. Int J Cardiol. 2005 Jan;98(1):21-5
- Scheuermann-Freestone M, Orchard E, Francis J, Petersen M, Friedrich M, Rashid A, Shore D, Myerson S, Neubauer S. Images in cardiovascular medicine. Partial congenital absence of the pericardium. Circulation. 2007 Aug 7;116(6):e126-9
COTW handling editor: Sylvia Chen
Have your say: What do you think? Latest posts on this topic from the forum







