Case from: Wilson T. King, MD; Andrew J. Powell, MD.
Institute: Children’s Hospital Boston; Boston, Massachusetts, USA.
Clinical history: A previously healthy 18-year-old woman presented to an outside medical facility with fever and left scapular pain and was found to have an elevated D-dimer. She underwent a CT angiogram for a suspected pulmonary embolus. The CT was negative for an embolus and she was ultimately diagnosed with an epidural abscess. However, the CT identified that all of the right pulmonary veins drained into the inferior vena cava (IVC)(Figure 1).

Figure 1: CT angiogram reformatted in an oblique coronal plane
CMR Findings: A CMR examination was ordered primarily to evaluate whether the left to right shunt was significant enough to warrant surgical repair. SSFP cine and 3D contrast MR angiography showed that right pulmonary veins drained not only to the IVC, but also to the superior vena cava (SVC)(Figure 2, Movie 1, 2 and 3). This represented an unusual variant of partially anomalous pulmonary venous connection (PAPVC) in which the right pulmonary veins drained to both the IVC and SVC, and not to the left atrium.

Movie 1: 3D contrast MR angiogram reformatted to an axial plane. Note that there is also a left aortic arch with an aberrant origin of the right subclavian artery.
Movie 2: 3D contrast MR angiogram reformatted to a coronal plane.
Movie 3: Volume rendering of the 3D contrast MR angiogram.

Figure 2: Volume rendering of the 3D contrast MR angiogram viewed posteriorly. Abbreviations: IVC=inferior vena cava, LLPV=left lower pulmonary vein, LUPV=left upper pulmonary vein, RLPV=right lower pulmonary vein, RPV=right pulmonary vein, RUPV=right upper pulmonary vein, SVC=superior vena cava.
Phase contrast flow measurements yielded: 1) a Qp:Qs of 2.0 (main pulmonary artery flow/ascending aorta flow), 2) equal branch pulmonary artery flow, and 3) 75% of right pulmonary venous flow drained to the SVC and 25% to the IVC. Phase contrast MRI with in-plane velocity encoding provided additional confirmation of the dual drainage (Movie 4).
Movie 4: Phase contrast MRI in an oblique coronal plane with in-plane flow encoding in the superioinferior direction. The velocity data is displayed using a color scale and overlaid on the magnitude images. Superior flow is red and inferior flow is blue.
SSFP cine ventriculography was notable for severe right ventricular dilation (end-diastolic volume 170ml/m2) and normal systolic function (ejection fraction 58%).
Follow-up: The CMR data supported surgical intervention by identifying a significant left-to-right shunt, severe right ventricular dilation, and equal branch pulmonary blood flow. The discovery on CMR that the right pulmonary veins drained to the SVC as well as the IVC led to an important modification of the surgical plan. The right pulmonary vein to SVC connection was addressed by constructing a baffle within the SVC and right atrium that directed pulmonary venous blood flow across the atrial septum into the left atrium. The right pulmonary vein to IVC connection was treated with banding rather than ligation in order to provide an alternative drainage route in the event the SVC-to-left atrial baffle pathway became obstructed.
A CMR study was performed on post-operative day 6 to assess the surgical repair. The SVC-to-left atrial pulmonary venous baffle pathway was unobstructed (Figure 3). The Qp:Qs normalized to 1.0, the RV end-diastolic volume decreased to 125ml/m2, and the RV ejection fraction decreased to 49%. Now, 94% of the right pulmonary venous flow drained via the SVC-left atrial baffle, and 6% via the IVC.

Figure 3: SSFP cine image in an oblique coronal plane after repair. Abbreviations: LA=left atrium, RA=right atrium, RPV=right pulmonary vein.
Perspective: This case presents an unusual variant of PAPVC in which there was right pulmonary venous drainage to both the IVC and SVC, and none to the left atrium. CMR provided a complete anatomical and functional evaluation both pre- and post-operatively. In retrospect, the right pulmonary venous drainage to the SVC was inconspicuous by CT angiography because the dense contrast in the SVC gave the appearance of a boundary between it and the less densely opacified adjacent right pulmonary vein (Figure 4).
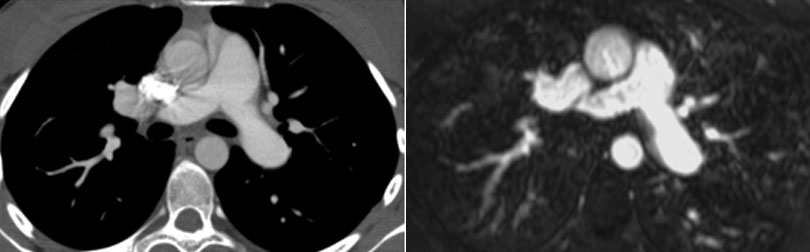
Figure 4: Corresponding axial reformatted images for the CT (left) and MR angiograms (right).
PAPVC is a congenital cardiac anomaly in which some but not all of the pulmonary veins connect to the systemic veins. (1,2) The most common variants include the left upper pulmonary vein to innominate vein, right upper pulmonary vein to the superior vena cava, and right pulmonary veins to the inferior vena cava. (3) Nonetheless, numerous variations of PAPVC have been described. (4) Furthermore, PAPVC is associated with congenital conditions such as atrial septal defects, tetralogy of Fallot, pulmonary hypoplasia and pulmonary sequestration in the setting of scimitar syndrome, Noonan’s syndrome and Turner’s syndrome.
References:
1. Healy JE Jr. An anatomic survey of anomalous pulmonary veins: their clinical significance, Journal of Thoracic Cardiovascular Surgery. 1952; 23:433-444.
2. Hughes C, Rumore P. Anomalous pulmonary veins, Archives of Pathology. 1944; 37:364-366.
3. Geva T, Van Praagh S. Abnormal pulmonary venous connections. In Allen H, Driscoll D, Shaddy R, Feltes T et al.,eds. Heart Disease in Infants, Children and Adolescents. Baltimore: Wilkins & Wilkins, 1995. -7th:pp 761-792.
4. Geggel RL. Scimitar syndrome associated with partial anomalous pulmonary venous connection at the supracardiac, cardiac and infracardiac levels. Pediatric Cardiology. 1993; 14(4):234-237.
COTW handling editor: M. Jay Campbell, MD
Have your say: What do you think? Latest posts on this topic from the forum





