Case from: Mirza Nubair Ahmad1, Fawad Khaliq1, Haroon Yousaf1, Daniel C. Bloomgarden2, Khawaja Afzal Ammar1
Institute: 1Aurora Cardiovascular Services, Aurora Sinai/Aurora St. Luke’s Medical Centers, Milwaukee, Wisconsin, USA; and 2Milwaukee Radiologists Ltd., Aurora St. Luke’s Medical Center, Milwaukee, Wisconsin, USA
Clinical history:
A 77-year-old man presented with a 2-week history of low-grade fever and dyspnea. Chest X-ray revealed large pleural effusions on the right side (Figure 1-A).
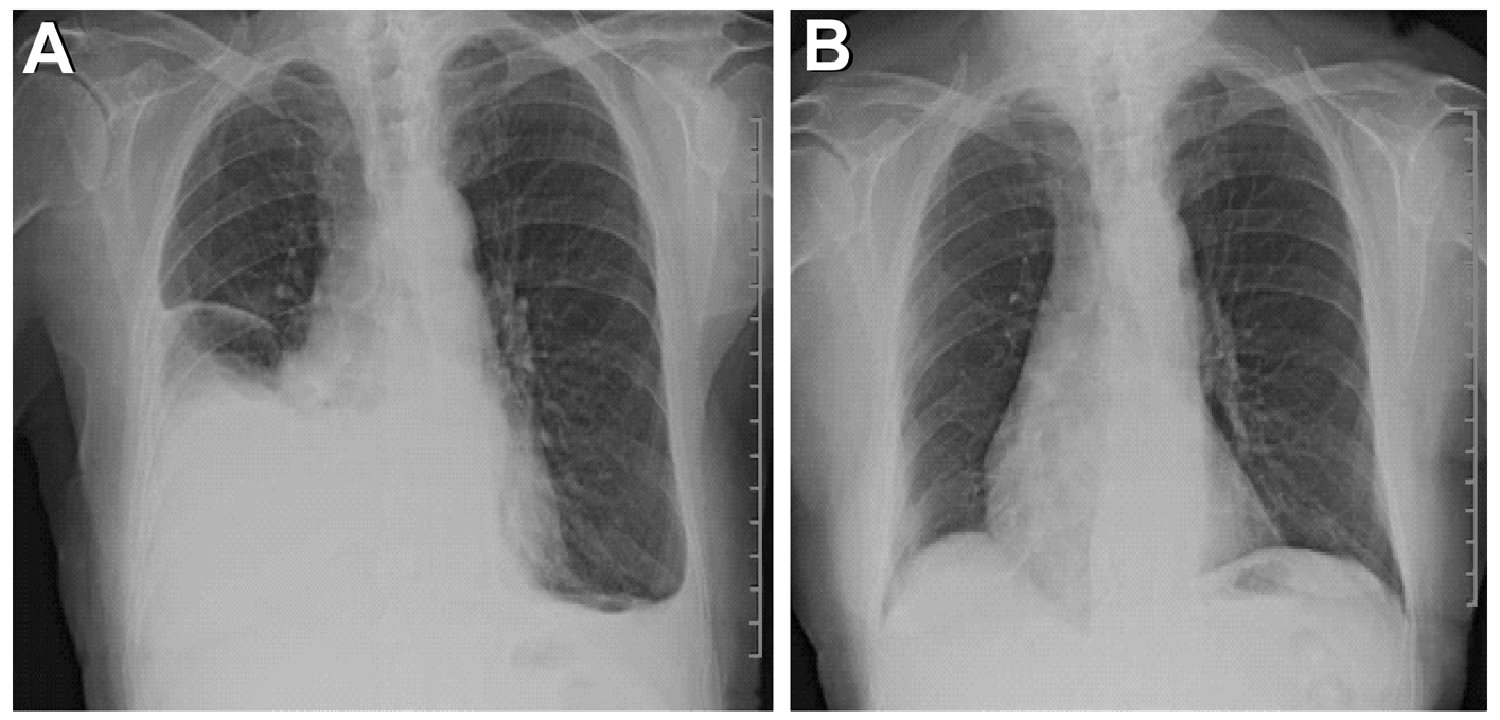
Figure 1: Chest X-ray before steroids (Panel A) and after steroids (Panel B).
Electrocardiogram did not show any signs of inflammation. Echocardiogram (Figure 2) revealed enlarged atria with normal ventricles, valves and pericardium.
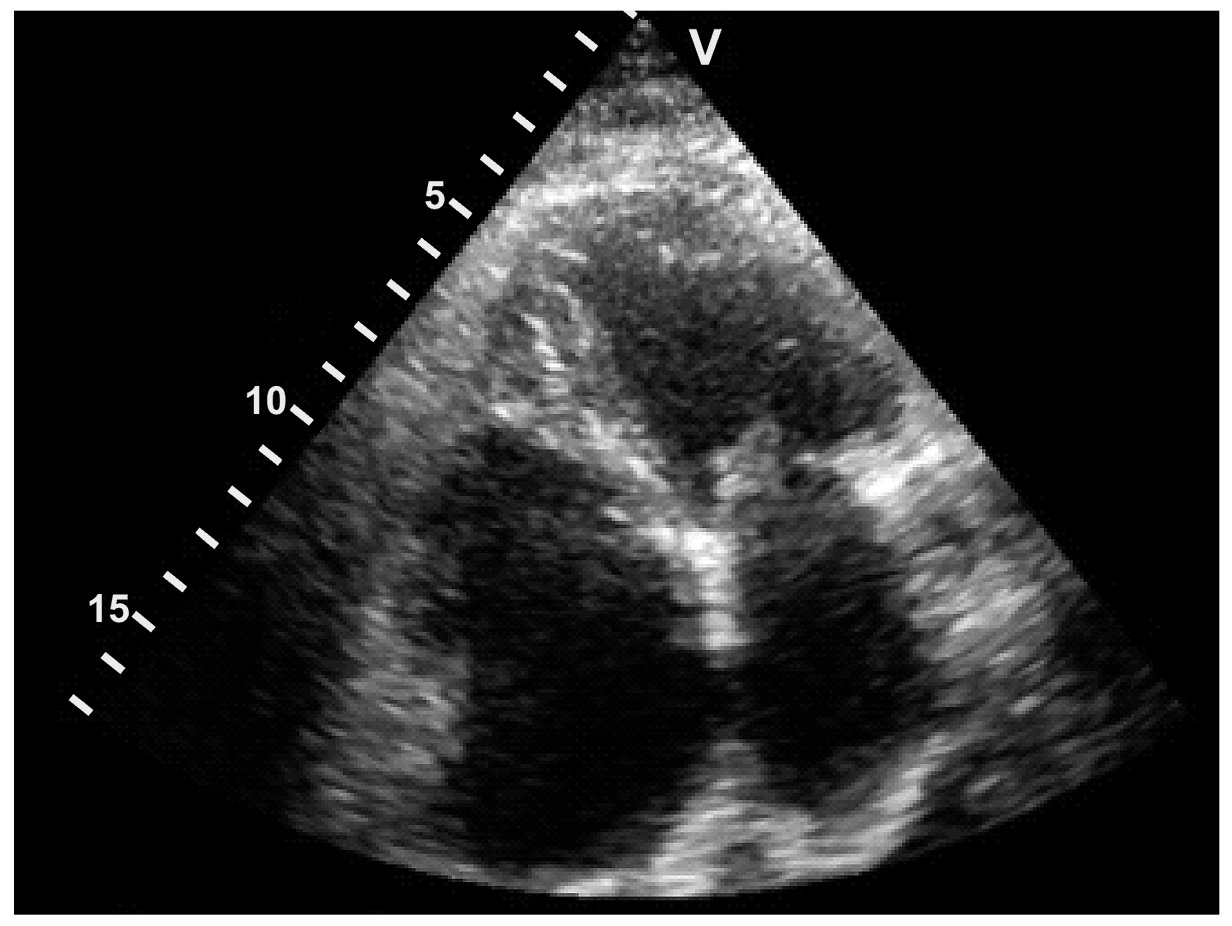
Figure 2: Echocardiogram did not show pericardial effusion.
Approximately 1.5 liters of nonmalignant, noninfectious inflammatory exudate was aspirated on thoracocentesis. However, the patient had multiple recurrences, with multiple thoracocenteses and similar outcomes. A pleural decortication surgery was planned. Prior to the surgery, he developed atrial fibrillation. Due to the pleuritic nature of pain and history of low-grade fever, late gadolinium-enhanced CMR imaging was ordered.
CMR Findings: Late gadolinium enhancement revealed marked enhancement of the pericardium with no enhancement of parietal or visceral pleura despite large pleural effusions (Figure 3-A), consistent with primary pericardial inflammation with secondary pleural effusions. Erythrocyte sedimentation rate was 100 mm/hr. The diagnosis of primary pericarditis with secondary reactive pleural effusion was made. Steroid therapy led to near-complete resolution of pericarditis (Figure 3-B) and pleural effusions (Figure 1-B) as well as normalization of erythrocyte sedimentation rate.
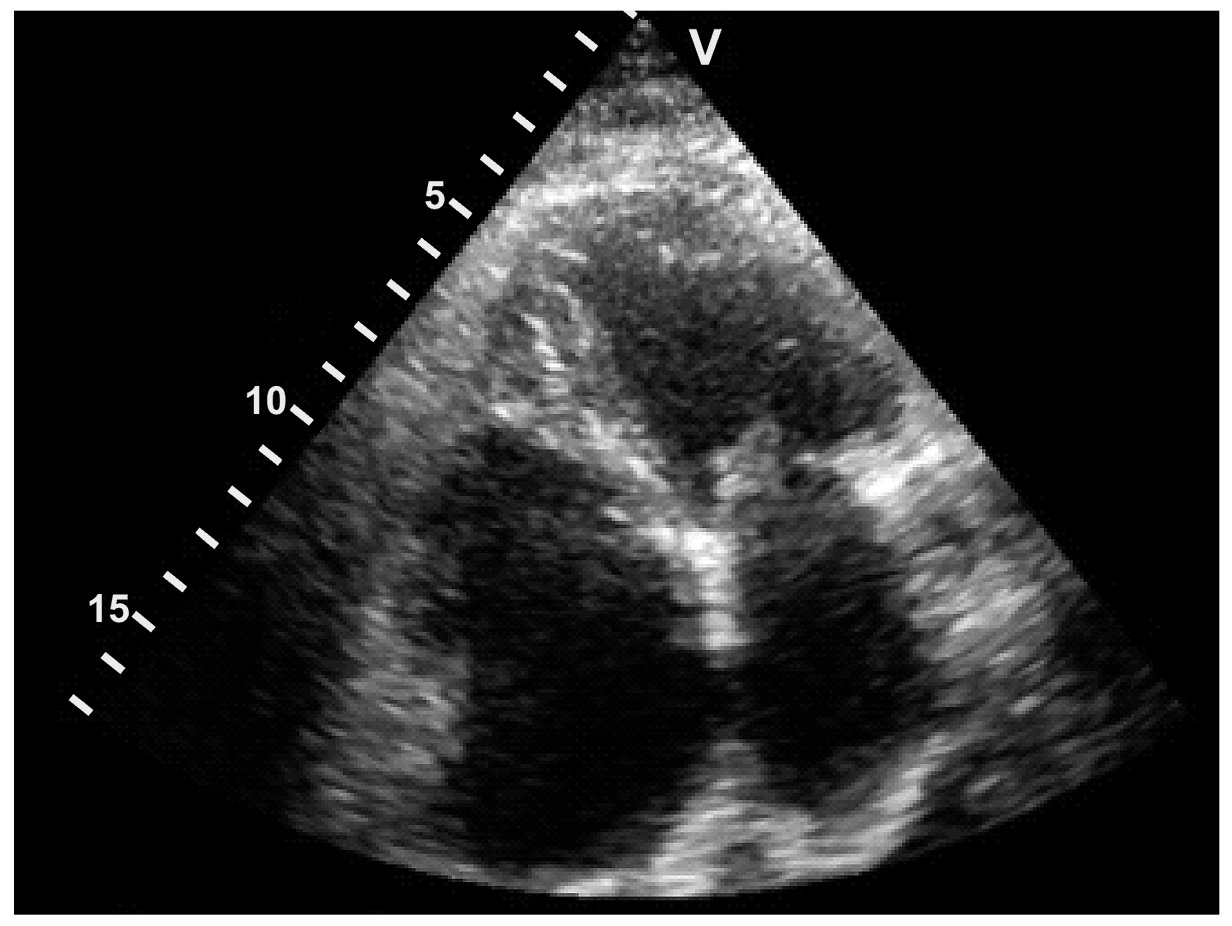
Figure 3: Late gadolinium-enhanced cardiac magnetic resonance image (Panel A) of inflamed pericardium (arrow) and noninflamed pleura, but reactive pleural effusion. Cardiac magnetic resonance image (Panel B) acquired after steroid therapy.
Conclusion: Our case describes using CMR to alter the clinical course; pleural decortication surgery, which would have been otherwise carried out for the treatment of recurrent idiopathic pleural effusions, was avoided. Should we always consider CMR in patients with recurrent idiopathic pleural effusions? While it will take more such cases to change clinical practice, this case suggests CMR should be considered in the management of idiopathic pleural effusions, especially prior to surgery, even if electrocardiogram and echocardiogram are normal. The ability of CMR to detect pericardial inflammation is clearly additive and complementary to our current clinical tools.
Perspective: Pleural effusion is a known but uncommon manifestation of pericarditis; sometimes it is the only presenting sign, making the diagnosis of pericarditis a difficult one in such patients. Traditionally the diagnosis of pericarditis is a clinical one, aided by the presence of inflammatory signs on electrocardiogram and confirmed by the presence of pericardial fluid on echocardiography. Using late gadolinium-enhanced cardiac magnetic resonance (CMR) imaging to diagnose pericarditis also has been reported by Feng et al.,1 but should it be considered in patients if electrocardiogram and echocardiogram are normal? This case demonstrate clinical utility of using CMR to diagnose pericarditis in suspected cases as well as in patients to rule out pericarditis as the primary etiology of recurrent idiopathic pleural effusions.
References:
- Feng D, Glockner J, Kim K, Martinez M, Syed IS, Araoz P, Breen J, Espinosa RE, Sundt T, Schaff HV, Oh JK. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after antiinflammatory medical therapy: a pilot study. Circulation. 2011,124:1830-7.
COTW handling editor: Sylvia Chen, MD
Have your say: What do you think? Latest posts on this topic from the forum







