Case from: Aurelia Grosu1, Patrizia Pedrotti2, Giovanni Quarta1, Paolo Brambilla1, Alberto Roghi2, Antonello Gavazzi1, Michele Senni1
Institute: 1) AO Papa Giovanni XXIII, Bergamo, Italy; 2) AO Niguarda Ca’ Granda, Milano, Italy
Clinical history:
The first patient is a 67-years old woman admitted to the hospital with an inferior acute myocardial infarction, treated with PTCA and stenting to right coronary artery. After the procedure, there was inferior ST elevation persistence. After 5 months the patient was admitted with cardiogenic shock. Echocardiography showed a large infero-posterior aneurysm (70 X 55 mm) without evidence of thrombus within it (Movie 1-2) and significant mitral regurgitation (Movie 3).

Movie 1: Echocardiogram with large
inferoposterior aneurysm without thrombus
Movie 2: Additional view of aneurysm
Movie 3: Associated severe mitral regurgitation
She underwent a cardiac CT scan (Figure 1) and angiography (Movie 4), which confirmed an inferior aneurysm. To improve accuracy of anatomical assessment, she was referred for a cardiac MRI.
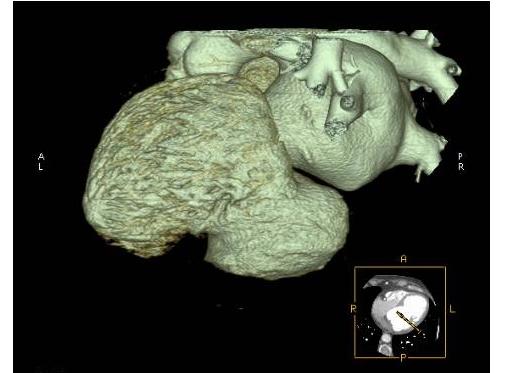
Figure 1: Cardiac CT demonstrating large ventricular aneurysm

Movie 4: Ventriculogram
The second patient is an asymptomatic 63-years old man with several cardiovascular risk factors, with signs of previous inferior myocardial infarction on ECG and on echocardiography (Movie 5) during a routine visit. Coronary angiogram showed chronic right coronary artery obstruction and severe left anterior descendent stenosis. LV angiogram (Movie 6) showed a large inferior aneurysm.
Movie 5: Echocardiogram of second patient
showing an inferior wall ventricular aneurysm Movie 6: LV angiogram
CMR Findings:
CMR from first patient confirmed a large infero-posterior aneurysm. The aneurysm started just below the mitral valve annulus and involved the posterior papillary muscle, resulting in systolic restriction of posterior MV leaflet and significant mitral regurgitation, with an eccentric, posterior jet (ischaemic MR) (Movie 7-9).
Movie 7: 4 chamber cine CMR with eccentric
mitral regurgitant jet

Movie 8: 2 chamber cine CMR with inferior
aneurysm

Movie 9: Short axis cine CMR with mitral annular
involvement
Early gad images confirmed the presence of thrombus (Figure 3). On late gadolinium images (suboptimal due to breathing artifacts) there was transmural LGE, which was in continuity with the pericardial layer; therefore it was suggested that this was a pseudo-aneurysm (Figure 4).
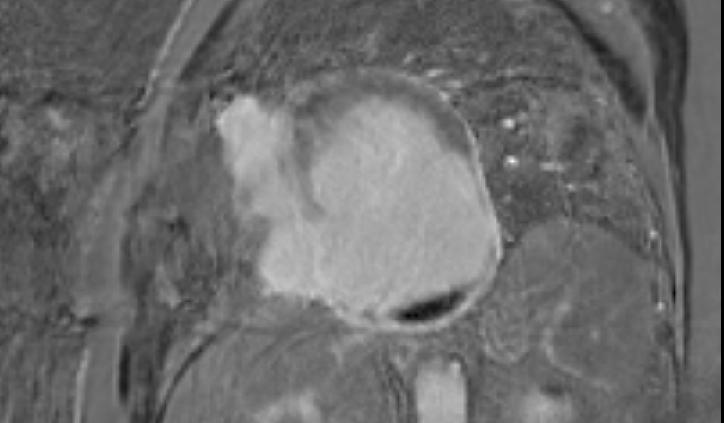
Figure 3: Early post gadolinium image
demonstrating thrombus within the aneurysm
(black crecent)
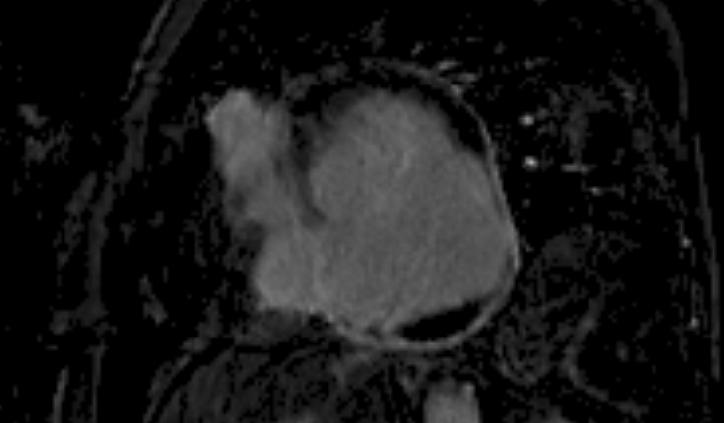
Figure 4: Late post gadolinium image
demonstrating transmural enhancement of the
aneurysm border continuous with the
pericardium
CMR from the second patient showed a large inferior aneurysm, starting 1 cm below the mitral valve annulus and stopping just medially to the posterior papillary muscle, without involving it; as a consequence, there was only trivial, posteriorly directed mitral regurgitation jet (Movie 10-13). There was no thrombus on early gad images. Late gadolinium enhancement showed transmural LGE, but a tiny epicardial layer was still visible (Figure 5-7). Therefore, it was suggested that this was a true aneurysm.
Movie 10: 4 chamber cine without suggestion of significant aneurysm
Movie 11: 2 chamber cine with large inferior aneurysm below the mitral valve
Movie 12: 3 chamber cine showing same aneurysm extending to the basal inferolateral segments

Movie 13: Basal short axis cine demonstrating region of aneurysm

Figure 5: Late gadolinium enhancement with
large infarcted area surrounded by very thin
strip of myocardial tissue

Figure 6: Late gadolinium enhancement
of same patient demonstrating
thin segment of dark tissue surrounding infarct
consistent with intact myocardium
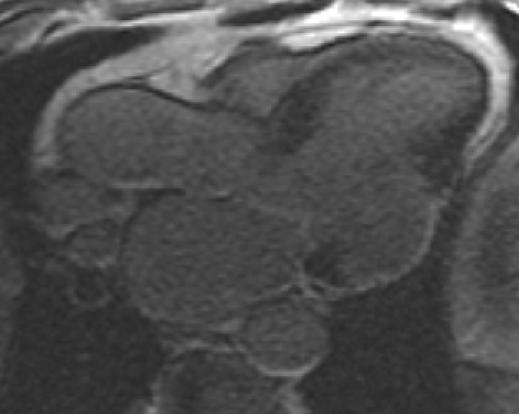
Figure 7: Late gadolinium enhancement
showing similar finding
Conclusion: Both patients underwent surgical treatment. Surgical exploration confirmed CMR diagnosis: pseudo-aneurysm with a thrombus for the first patient (figure 8), who underwent a successful CABG, aneurysmectomy and mitral valve replacement; true aneurysm without thrombus for the second patient (Figure 9), who underwent a successful CABG and aneurysmectomy; the detailed CMR description of the position of the aneurysm with respect to papillary muscles was fundamental for precise patch insertion, therefore damage or distortion of geometry of papillary muscles was avoided and patient did not need mitral valve repair/replacement.
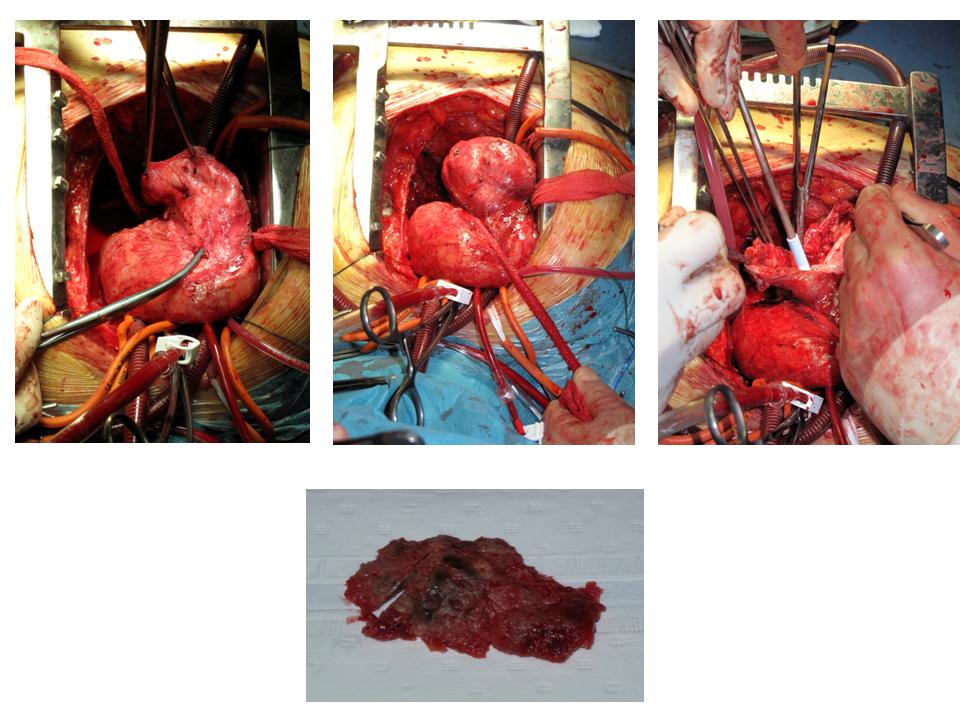
Figure 8: First patient with false aneurysm and associated thrombus undergoing resection
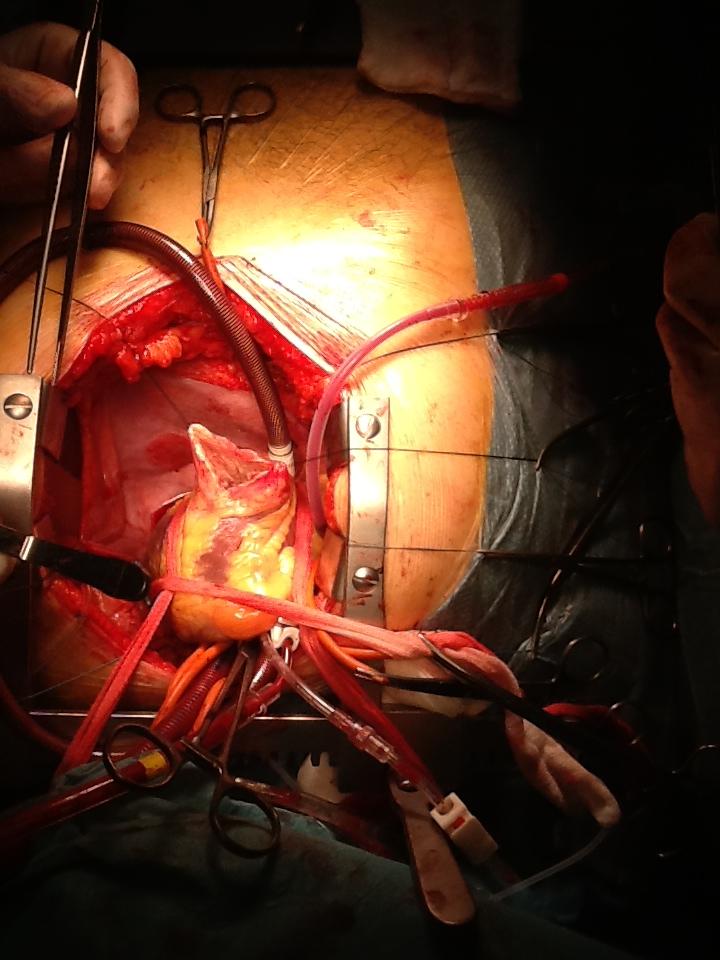
Figure 9: Second patient with true aneurysm without thrombus undergoing
resection
Perspective: Left ventricular free wall rupture is a rare, catastrophic complication of myocardial infarction, occurring in approximately 4% of patients (1). Overlying adherent pericardium may contain the defect, forming a false (pseudo) aneurysm. (2). Pseudoaneurysms are often detected incidentally by echocardiography or other imaging modalities. Lacking the structural support of myocardium, a LV pseudoaneurysm carries a significant risk of expansion and fatal rupture (3) and surgical treatment is often indicated. In contrast, true aneurysm consists of a thin, scarred ventricular wall which expands outwards during systole. Both true and false aneurysm may result in heart failure, thromboembolic events, ventricular arrhythmias. Distinguishing between true and false LV aneurysm is essential for appropriate treatment and prognosis. (4). The most important feature differentiating true and a false aneurysm is the presence of a continuous pericardial layer surrounding myocardial wall which is present only in the true aneurysm. In pseudo-aneurysm, thrombotic apposition may give the false impression of presence of a pericardial layer.
Contrast ventriculography, radionuclide ventirculography, transthoracic and transesophageal echocardiography, cardiac CT and cardiac MRI have been proposed to distinguish the two entities.
Echocardiography has the advantage of easy accessibility and widespread availability (6). Given its 3D properties and tissue characterization, CMR is ideal to study the location and the shape of aneurysms even when particularly deformed, and their relation with nearby structures, like papillary muscles (7). This, as shown in our cases, is particular important for surgical planning. In addition, MR study can further evaluate the pathological characteristics of the aneurysm and can help in differentiating false and pseudo aneurysm using late gadolinium enhancement technique. Thus, as shown in our cases, MR imaging could be considered a very powerful tool for detecting and characterizing ventricular aneurysms.
References:
- 1. Pollak H, Nobis H, Mlczoch J. Frequency of left ventricular free wall rupture complicating acute myocardial infarction since the advent of thrombolysis.Am J Cardiol. 1994 Jul 15;74(2):184-6.
- 2. Brown SL, Gropler RJ, Harris KM. Distinguishing left ventricular aneurysm from pseudoaneurysm. A review of the literature. Chest. 1997 May;111(5):1403-9.
- 3. Atik FA, Navia JL, Vega PR, Gonzalez-Stawinski GV, Alster JM, Gillinov AM, Svensson LG, Pettersson BG, Lytle BW, Blackstone Surgical treatment of postinfarction left ventricular pseudoaneurysm. EH. Ann Thorac Surg. 2007 Feb;83(2):526-31.
- 4. Gologorsky E, Gologorsky A, Barron ME, Hassan M, Ricci M, Salerno T. Echo rounds: transesophageal echocardiography images of an inferior wall pseudoaneurysm: a difficult differential diagnosis. Anesth Analg. 2010 Sep;111(3):613-5. doi: 10.1213/ANE.0b013e3181e9efd1. Epub 2010 Jul 2.
- 5. Gatewood RP Jr, Nanda NC. Differentiation of left ventricular pseudoaneurysm from true aneurysm with two dimensional echocardiography. Am J Cardiol. 1980 Nov;46(5):869-78.
- 6. Trindade ML, Tsutsui JM, Rodrigues AC, Caldas MA, Ramires JA, Mathias Junior W. Left ventricular free wall impeding rupture in post-myocardial infarction period diagnosed by myocardial contrast echocardiography: case report. Cardiovasc Ultrasound. 2006 Jan 26;4:7.
- 7. Konen E, Merchant N, Gutierrez C, Provost Y, Mickleborough L, Paul NS, Butany J. True versus false left ventricular aneurysm: differentiation with MR imaging-initial experience. Radiology. 2005 Jul;236(1):65-70. Epub 2005 Jun 13.
COTW handling editor: Kevin Steel, DO, FACC







