Case from: Steve Muyskens M.D., Shelly Gossett BSRS RT(R)(MR)
Institute: Cook Children’s Heart Center, Fort Worth, TX, USA
Clinical history: A 17 year-old male with a history of simple d-transposition of the great arteries status post arterial switch operation at age 3 days presented for routine annual evaluation. Historically, he was an active teenager participating in football and basketball without symptoms. At his previous evaluation, his echocardiogram demonstrated normal global and regional ventricular function, patent coronary artery origins, and mild aortic insufficiency. His standard 12-lead electrocardiogram and treadmill exercise stress test were normal (Figure 1).
At presentation he reported increasing aerobic exercise intolerance characterized by shortness of breath and fatigue, particularly with running. He additionally complained of periodic chest discomfort and a chronic cough, but these were not temporally related to exercise. A standard 12-lead electrocardiogram (Figure 2) demonstrated a non-specific T-wave abnormality and subtle Q wave changes in leads I and aVL. The echocardiogram was unchanged from his previous visit, again demonstrating normal global and regional ventricular function (shortening fraction 31%) and patent coronary artery origins. He was referred to cardiac MRI for comprehensive evaluation of his pulmonary artery anatomy, coronary artery anatomy, and ventricular function and viability.
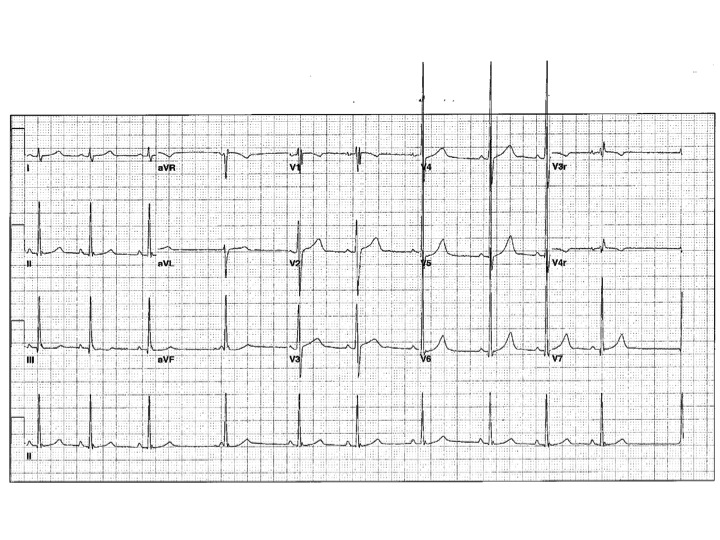
Figure 1 (Baseline ECG
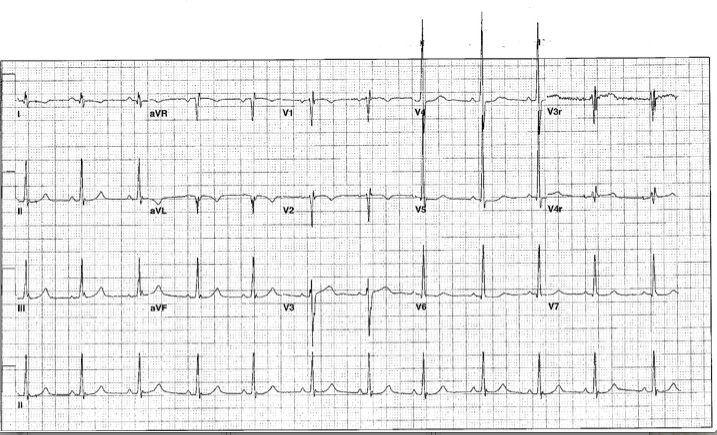
Figure 2 (ECG on presentation with excercise intolerance)
CMR Findings: Steady-state free precession cine images (Movies 1 through 5) demonstrated normal left ventricular size (104 ml/m2), no regional wall motion abnormalities, but borderline to mildly depressed global left ventricular systolic function (EF 49%) (1). His branch pulmonary artery anatomy was unremarkable.

MOVIE 1: SHORT AXIS – BASAL

MOVIE 2: SHORT AXIS – MID
MOVIE 3: SHORT AXIS APEX
MOVIE 4: 2-CHAMBER

MOVIE 5: 4-CHAMBER
3D IR-FLASH imaging with slow infusion (0.4mL/sec) of double dose contrast (0.4mL/kg gadopentetate) and respiratory navigation was performed to evaluate the origins and proximal courses of the coronary arteries. The proximal left main coronary artery was narrow, measuring approximately 2mm, with an acute angulation as well as an interarterial course concerning for a vice anomaly (Figure 3 and 4). The right coronary artery origin was widely patent (Figure 5)
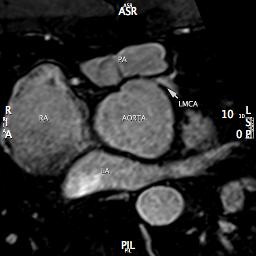
Figure 3 (Mulit Planar Reformat of LCA Origin)
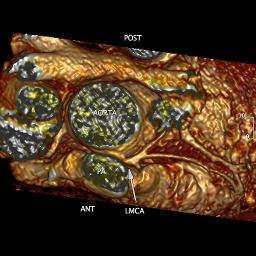
Figure 4 (3D Volume Rendering Showing LCA Origin From Above)
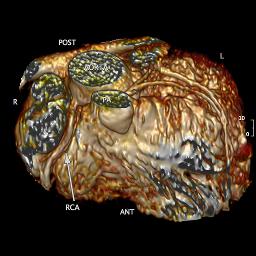
Figure 5 (3D Volume Rendering Showing Coronary Origins)
Late gadolinium enhancement (LGE) demonstrated multiple areas of subendocardial hyperenhancement restricted to the left anterior descending and left circumflex coronary artery distributions. There was sparing of the right coronary artery distribution (Figures 6 through 9).
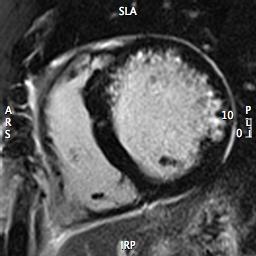
Figure 6 (Short Axis Base)
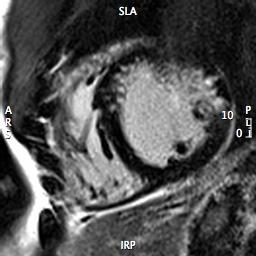
Figure 7 (LGE Short Axis Mid)
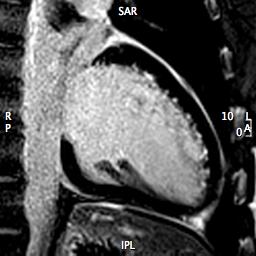
Figure 8 (LGE 2-Chamber)
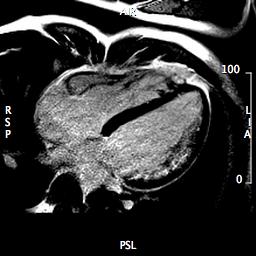
Figure 9 (LGE 4-Chamber)
Given the concerns regarding inducible ischemia, a nuclear medicine myocardial rest and stress SPECT exam was performed using Bruce 2-minute protocol and administration of technetium 99m-tetrofosmin. Resting heart rate was 83 bpm. Maximum heart rate during stress was 184 bpm, representing 90% of the maximal age predicted heart rate. Exercise stress test was stopped due to shortness of breath and significant ST segment depressions (Figure 10). Patient denied chest discomfort.
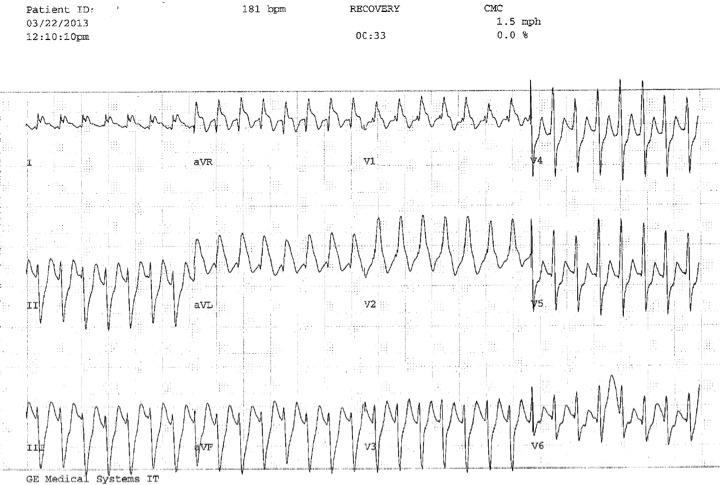
Figure 10 (Excercise Stress ECG)
The SPECT stress images demonstrated a large area of diminished perfusion involving the anteroseptal and anterior wall of the left ventricle (Figure 11). Inferior myocardium was better perfused. The rest images were normal with no visible perfusion defects. There was depressed global function at stress.
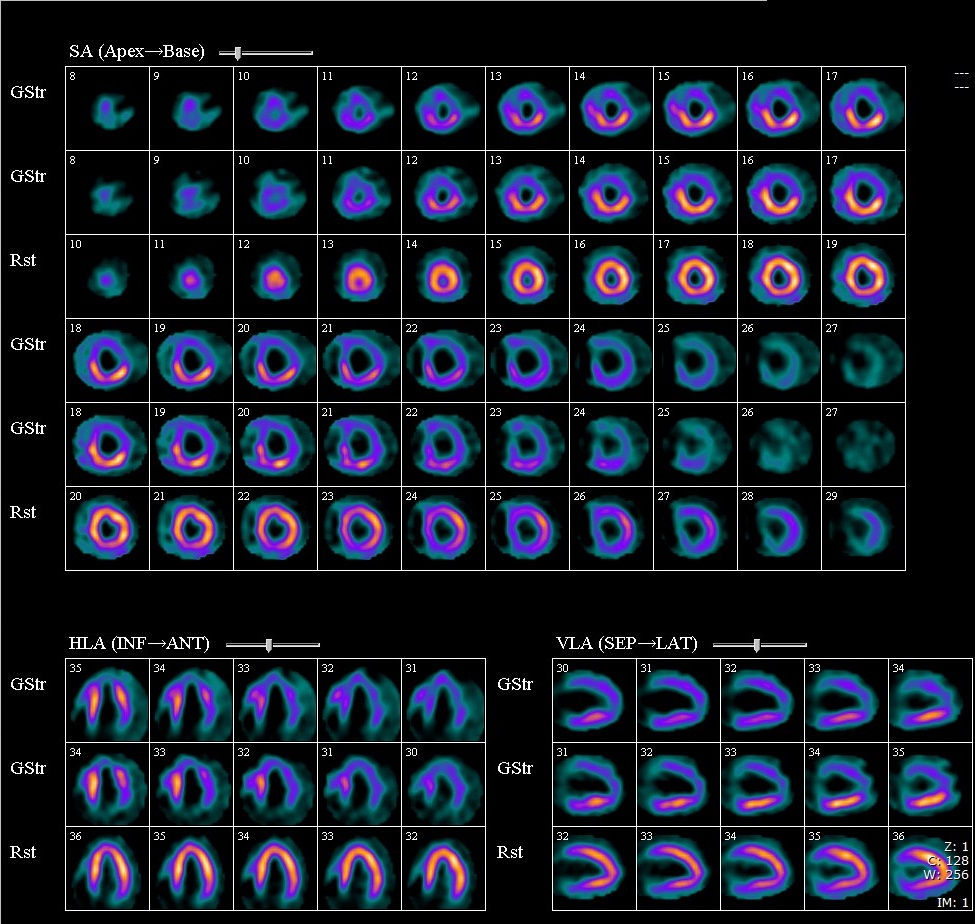
FIGURE 11 (SPECT MYOCARDIAL STRESS PERFUSION: Images are organised showing Stress Supine (the top stress line) and Stress Prone (the bottom stress line) followed by Rest images)
The patient was taken to the catheterization lab and selective angiography reaffirmed left coronary ostial stenosis and excluded distal coronary artery disease. The patient was referred for surgical correction. Inspection confirmed left coronary ostial stenosis with proximal interarterial course. He underwent successful coronary artery repair. His post-operative course was uncomplicated and a repeat nuclear medicine myocardial stress SPECT after surgical repair demonstrated normal perfusion and normalized estimated ejection fraction at stress and rest.
Conclusion: Coronary ostial stenosis is a well-described complication of the arterial switch operation (2). This case demonstrates an atypical presentation of exercise induced ischemia with subendocardial scar formation in the absence of exercise induced chest pain. Transection of the aortic root during the arterial switch procedure can lead to denervation and subsequent lack of ischaemic chest pain. Cardiac MR has been shown to be an accurate non-invasive method of evaluating coronary artery anatomy and function (2). Currently, two techniques are primarily used to assess coronary anatomy. 3D SSFP with respiratory navigation does not require contrast and allows high quality images (3). This is the imaging modality of choice at most centers performing scans at 1.5 Tesla. At 3 Tesla, 3D SSFP with a T2 prep pulse is often not commercially available secondary to issues with violating acceptable SAR limits. Additionally, the increased off-resonance artifact with SSFP at 3 Tesla raises concerns regarding image quality. Therefore, a contrast enhanced 3D IR-FLASH with respiratory navigator is commonly performed (4). IR-FLASH is likely less prone to artifact and provides more robust contrast-to-noise ratio (5). Disadvantages of the protocol used include a single attempt at image acquisition and the use of double dose contrast for coronary imaging precludes adding rest and stress perfusion into the same imaging protocol. However, alternative protocols using single dose contrast at slow infusion for coronary imaging and half dose for rest and stress imaging could give all the information in a single exam. Another alternative would be to use dobutamine stress imaging in combination with our protocol or to use gadobenate dimeglumine, which is partially bound to Albumin, allowing a longer period for the IR-FLASH imaging. Future development of a modified T2 prep pulse profile, improved shimming of B0 field inhomogeneity, advanced respiratory motion compensation, and the use of intravascular contrast agents may offer different options for scanning these patients (5,6).
Perspective: Cardiac MRI is an important tool in the assessment of patients with congenital heart disease and coronary artery translocations. Presenting symptoms and etiologies can be diverse and atypical in this patient population. Cardiac MRI is ideal in evaluating these patients due to its ability to evaluate vascular anatomy, ventricular function, myocardial perfusion, and viability in a single exam. In our case, cardiac MRI allowed a refined evaluation despite the patient’s atypical presentation, was validated by multiple modalities, and resulted in a timely and successful surgical repair.
Scanner/Coil/Processing:
Siemens 3T Verio / 32 Channel Cardiac Coil/CMR42.
References:
1. Sarikouch S, Peters B, Gutberlet M, Leismann B, Kelter-Kloepping A, Koerperich H, Kuehne T, Beerbaum P. Sex-Specific Pediatric Percentiles for Ventricular Size and Mass as Reference Values for Cardiac MRI: Assessment by Steady-State Free-Precession and Phase-Contrast MRI Flow. Circ Cardiovasc Imaging. 2010;3:65-76.
2. Tanel RE, Wernovsky G, Landzberg MJ, Perry SB, Burke RP. Coronary artery abnormalities detected by cardiac catheterization following the arterial switch operation for transposition of the great arteries. Am J Cardiol. 1995;76:153-157.
3. Weber OM, Martin AJ, Higgins CB. Whole-heart steady-state free precession coronary artery magnetic resonance angiography. Magn Reson Med. 2003;50(6):1223-8.
4. Yang Q, Li K, Liu X, Bi X, Liu Z, An J, Zhang A, Jerecic R, Li D. Contrast-enhanced whole-heart coronary magnetic resonance angiography at 3.0-T: a comparative study with X-ray angiography in a single center. J Am Coll Cardiol. 2009;54(1):69-76.
5. Prompona M, Cyran C, Nikolaou K, Bauner K, Reiser M, Huber A. Contrast-enhanced whole-heart MR coronary angiography at 3.0 T using the intravascular contrast agent gadofosveset. Invest Radiol. 2009;44(7):369-74.
6. Henningsson M, Botnar R. Advanced respiratory motion compensation for coronary MR angiography. Sensors (Basel). 2013;13(6):6882-6889.
COTW handling editor: Tarique Hussain, MD







