Case from: Aamisha Gupta, Yuyang Zhang, Jayanth Keshavamurthy, Kenneth Murdison.
Institute: Children’s Hospital of Georgia at Georgia Regents University, Division of Pediatric Cardiology and Department of Radiology, Augusta, GA.
Clinical history:
A 17 year old male with a history of autism presented to the emergency room with a three day history of subjective fever, otitis media and acute onset of chest pain for one day. He was treated
initially with NSAIDs and amoxicillin/clavulanate but without full resolution of the pain. His associated symptoms included left-sided shoulder pain, shortness of breath and rigors. He denied
palpitations, syncope, cyanosis, headache, back pain, abdominal pain or vomiting. He also denied smoking or use of illicit drugs. In the emergency room, his initial labs were significant
for a regular troponin I of 54 ng/ml, a BNP of 233 pg/ml and a negative viral panel and urine drug screen. His initial EKG and echocardiogram were abnormal:
EKG IMAGE:
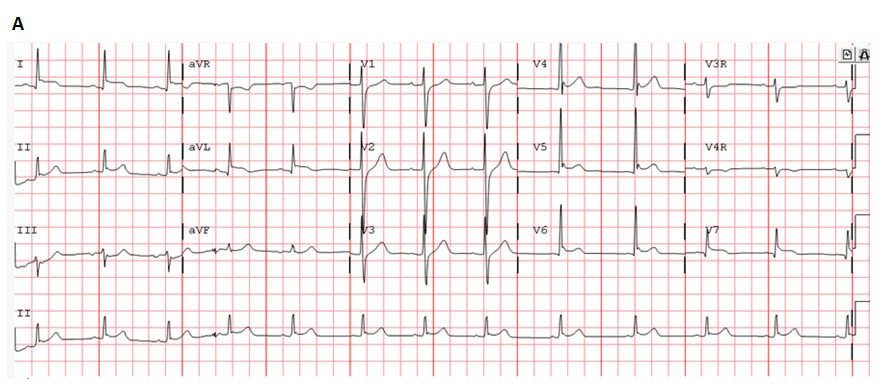
EKG A: His initial EKG demonstrated ST segment elevation in the lateral leads.
ECHO Findings: His initial echocardiogram demonstrated mildly diminished global systolic function (EF of 43%) with hypokinesia of the posterolateral wall. No pericardial effusion was
noted.Hospital Course:
He was transferred to the pediatric intensive care unit in normal sinus rhythm. He was initially
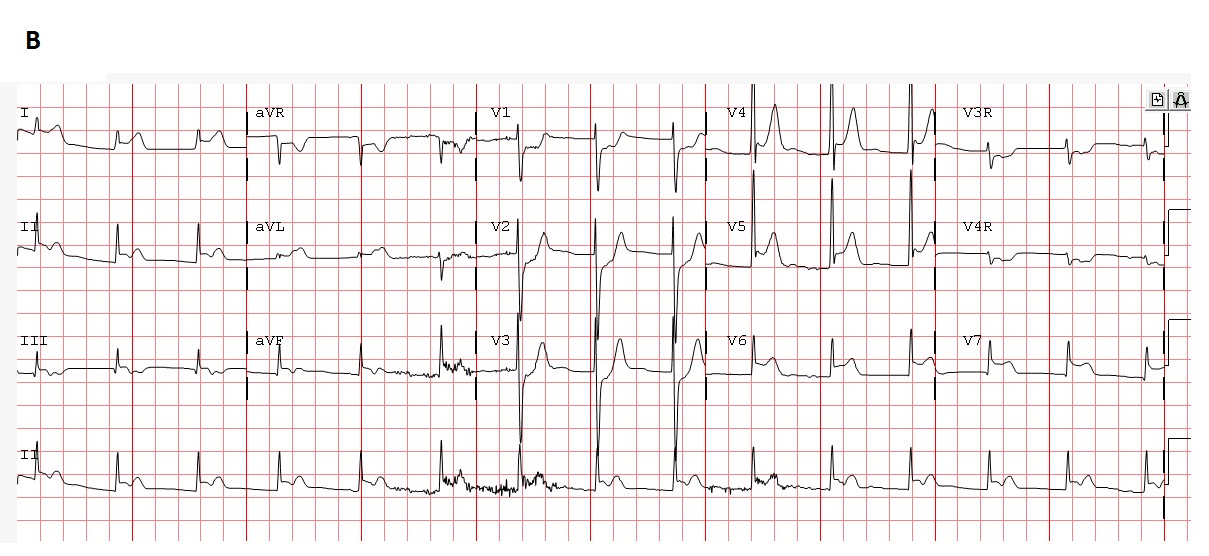
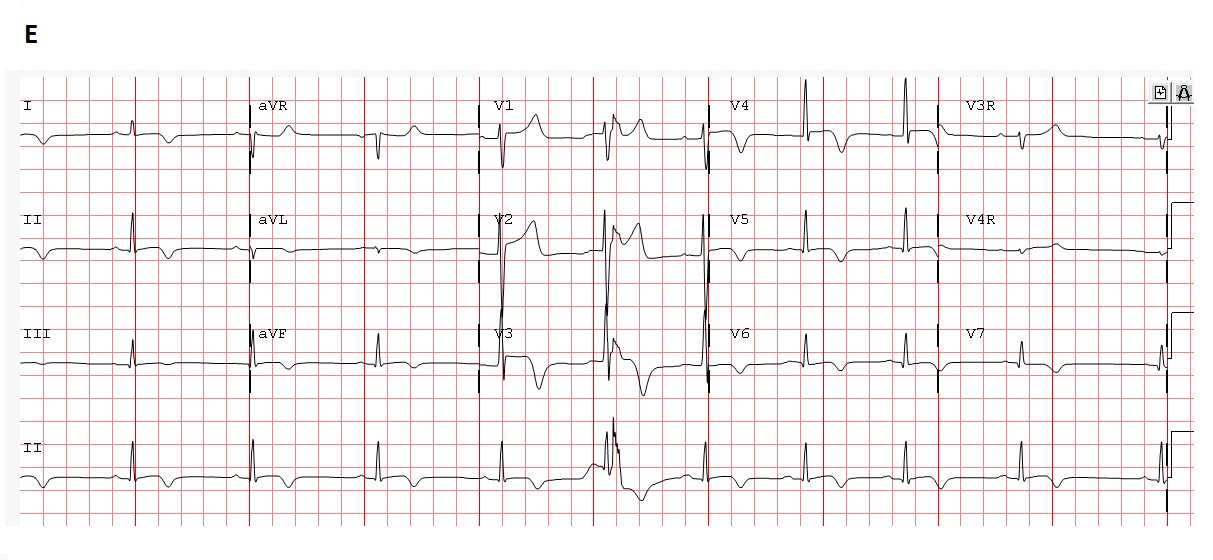
treated with scheduled NSAIDs for suspected pericarditis. After a decline to 32 ng/ml, repeat troponin I levels increased to 54 ng/ml, and serial EKGs demonstrated evolving ST changes (EKG images B and C).
EKG IMAGES:
He was started on anticoagulation therapy and underwent cardiac catheterization due to a suspected acute coronary event. Coronary angiography demonstrated normal vessel anatomy and patency, mildly diminished systolic function and an elevated left ventricular end-diastolic pressure of 17 mmHg. He was continued on NSAIDs and aspirin. A cardiac MRI (CMR) was performed on a Philips 3T magnet and included cine imaging, T2-weighted imaging for edema and T1-weighted post contrast images to detect late gadolinium enhancement (LGE).
CMR CINE IMAGING:
Video A: SSFP (cine) imaging in the “4-chamber” or ventricular long axis view demonstrated diminished LV function (ejection fraction of 40%), a small pericardial effusion and small bilateral pleural effusions.
EDEMA IMAGING:
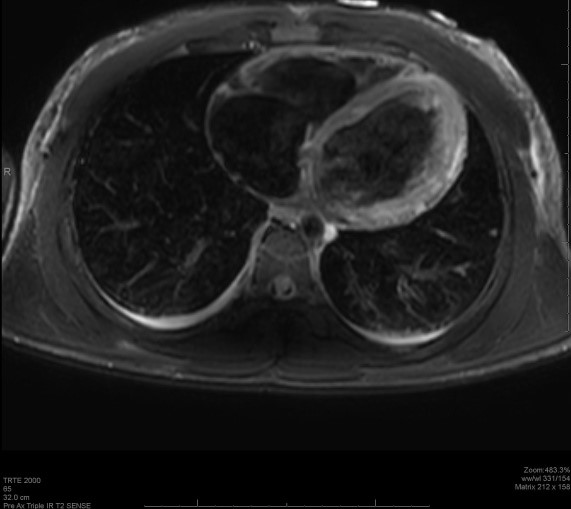
Image A. T2W-TSE image in the axial plane revealed high signal intensity of the left ventricular free wall.
LATE GADOLINIUM ENHANCEMENT (LGE) IMAGING:

LGE image B-Long axis (“4-chamber”)
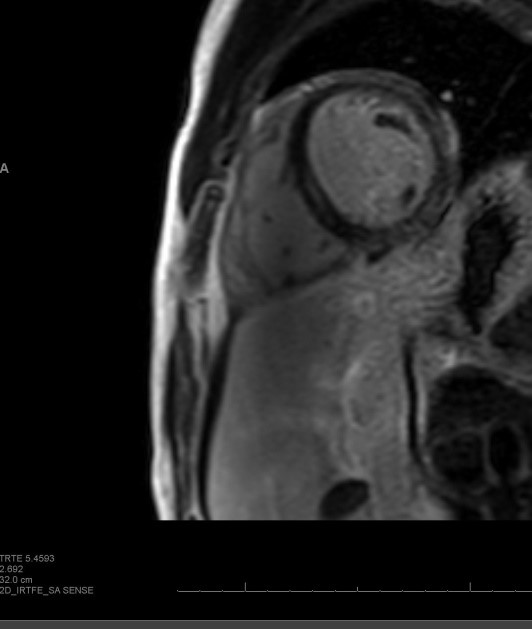
LGE image C-ventricular short axis
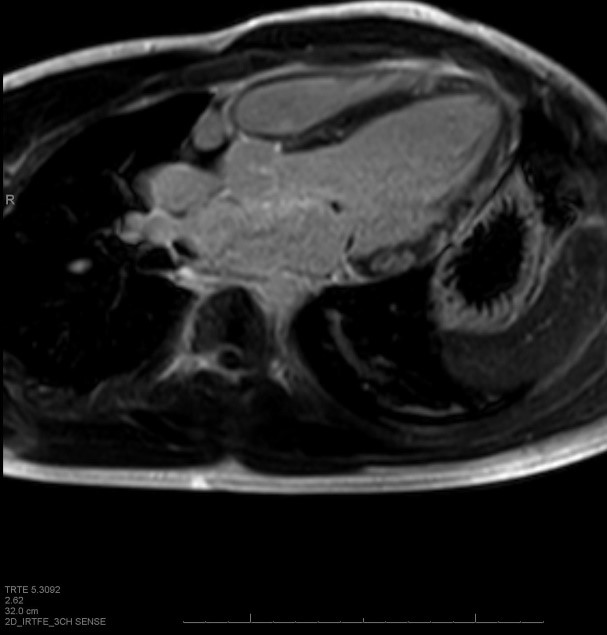
LGE image D- LV long axis (LVOT)
LGE Images B-D: T1W post contrast delayed inversion recovery sequences demonstrated multiple, patchy areas of enhancement of the subepicardial region of the myocardium with normal subendocardial layer. These areas were noted in the interventricular septum and free wall, in a non-coronary distribution, and were confirmed in multiple planes. A trivial pericardial effusion was also seen; all of which help support the diagnosis of myocarditis according to the Lake Louise consensus criteria[1].
Hospital Course, continued: Despite the EKG changes, CMR findings and the continued elevated troponin levels, the patient remained hemodynamically stable without arrhythmias throughout his hospital stay. He remained in the hospital for 1 week and was discharged once his troponin I levels normalized and EKG remained stable. He followed up for a repeat echocardiogram 10 days later that demonstrated no left ventricular segmental wall motion abnormalities or pericardial effusion. The left ventricular function remained mildly diminished (EF 55%).
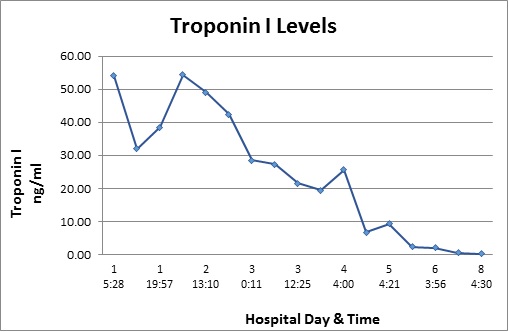
Table 1. The troponin I trend from admission to discharge.
Discussion:
Chest pain is a common complaint in children and adolescents presenting to the emergency room. However, a cardiac etiology for their chest pain is defined in only 0.6% out of all cases [3, 4]. Troponin I is the most cardiac-specific among the three subunits of the troponin complex and has high sensitivity for acute myocardial injury [2]. It has been established as a useful screening tool for the evaluation of acute coronary ischemic disease in adults, but not in acute perimyocarditis in the pediatric population [2, 4]. In children, reports of elevations of Troponin I are rare. According to a study of elevated troponins in adolescents with chest pain, the median peak troponin I level was 17.8 ng/ml [5]. Our case is interesting given the age of the patient as well as the extreme elevation of Troponin I to 54 ng/ml and his relative clinical stability.
Traditionally, endomyocardial biopsy was considered the gold standard for the diagnosis of myocarditis based on histopathology, immunohistology and molecular techniques [2]. CMR is becoming the standard imaging modality for the diagnosis of myocarditis both in adults and children[1,7]. The goals of a comprehensive CMR evaluation of active myocarditis should include evaluation of tissue injury which involves intracellular and interstitial edema, cellular necrosis, and fibrosis. The classic CMR findings of myocarditis include high signal on T2-weighted images and both early and delayed enhancement on post gadolinium T1-weighted images. This pattern of early and late gadolinium enhancement (LGE) may be focal, multi-focal or diffuse, and typically involves the supepicardial region or can extend into the mid-myocardial region. The subendocardium is spared which distinguishes myocarditis from an ischemic process [1]. If all the sequences are performed, the diagnostic accuracy of myocardial inflammation can be as high as 78% [1].
In adults, the presence of LGE on a patient’s initial CMR for myocarditis has been shown to be an independent predictor of all-cause mortality and cardiac mortality. In one study, no patients without LGE experienced sudden cardiac death[6]. Conversely, in a recent multicenter paper describing the CMR findings in a cohort of pediatric patients, the parameters found to be associated with persistent left ventricular dysfunction were larger LV dimensions and lower LVEF and RVEF, but not the presence of LGE. There was wide practice variation in the imaging protocols used and the authors recommended that further investigation needed to be performed in the pediatric population[7]. In regards to the importance of LGE on longer follow-up CMR, in a small adult study they found that if there was the presence of LGE four weeks after the initial CMR, this indicated a worse prognosis after a three year follow-up[8].
This case may provide useful to many clinicians because of the unusual clinical presentation with extreme troponin I elevation and progressive ST segment abnormalities, yet associated with a negative coronary catheterization. Perhaps as more cases like ours become known, future patients with similar presentations could avoid a cardiac catheterization. The classic CMR findings for myocarditis were crucial in establishing the diagnosis in this case.
References:
1. Friedrich M, Sechtem U, et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. Journal of the American College of Cardiology. 2009; 53: 1475-1487
2. Kern J, Modi R, Atalay M, Kochilas L. Clinical Myocarditis Masquerading as Acute Coronary Syndrome. Journal of Pediatrics. 2009; 154: 612-15
3. May J, Patton D, Fruitman D. The evolving approach to pediatric myocarditis: a review of current literature. Cardiology in the Young. 2011; 21: 241-251
4. Sharma J, Fernandes N, Alavarez D, Khanna S. Acute Myopericarditis in Adolescent Mimicking Acute Myocardial Infarction. Pediatric Emergency Care. 2015; 31(6): 427-30
5. Schwartz, MC. Wellen S, et al. Chest Pain with elevated troponin assay in adolescents. Cardiology in the Young. 2013. 23 (3): 353-360.
6. Grun S et al. Long-Term Follow-up of Biopsy-Proven Viral Myocarditis: Predictors of Mortality and Incomplete Recovery. Journal of the American College of Cardiology. 2012; 59 (19): 1604-15.
7. Banka P, Robinson J, Powell A, et al. Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. Journal of Cardiovascular Magnetic Resonance. 2015; 17: 96.
8. Wagner A., Schulz-Menger J., Dietz R., Friedrich M.G.; Longterm follow-up of patients with acute myocarditis by magnetic resonance imaging. MAGMA. 2003; 16: 17-20







