Ahmed Kharabish 1,2 Manuel Gutierrez 2 Monika Arzanauskaite 2,3
1. Radiology Department, Cairo University Hospitals, Cairo, Egypt
2. Radiology Department, Liverpool Heart and Chest Hospital, Liverpool, United Kingdom.
3. Cardiovascular Research Center-ICCC, Hospital de la Santa Creu i Sant Pau, IIB-Sant Pau, Barcelona, Spain
Case Published in the Journal of Cardiovascular Magnetic Resonance: Click here for the link
Click here for PubMed Reference to Cite this Case
Clinical history:
We report a case of suspected hypertrophic cardiomyopathy (HCM) with a rare diagnosis that was uncovered using cardiac MRI. A 75-year-old man, with a family history positive for hypertrophic cardiomyopathy (HCM). His transthoracic echo revealed asymmetrical myocardial thickening (Figure 1) without outflow obstruction or papillary muscles hypertrophy, mild to moderate mitral regurgitation, and normal sized right and left ventricles. Cardiac MRI was requested for further assessment of HCM, hemodynamics and tissue characterisation.
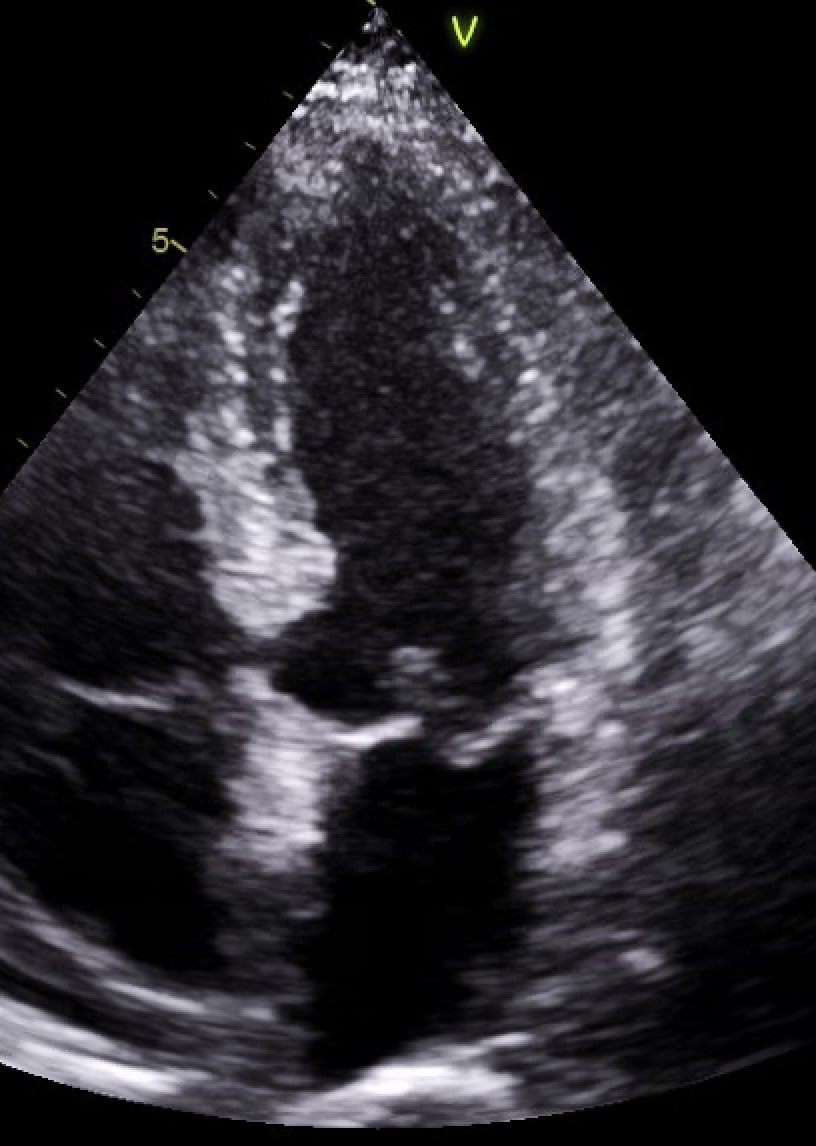
Figure 1
Cardiac MRI findings:
Cardiac MRI (Figures 2-4 and Videos 1-3) showed a normal sized left ventricle (LV) with mild hypertrophy of the basal septum (12mm). The remaining myocardial segments were of normal thickness (basal anterior and anterolateral walls: 7-8mm). There was hyperdynamic systolic function with hyperdynamic contraction of the LV basal posterolateral wall below the posterior mitral annulus. Papillary muscles were also normal. There was no obstruction in the LV outflow tract. Additionally there was bi-leaflet mitral valve prolapse (MVP) with thickened mitral leaflets, mitral annular disjunction (MAD) and mild to moderate mitral regurgitation. Importantly. on late gadolinium enhancement, MRI showed focal annular fibrosis in the posterior mitral annulus ( Figure 4).


Figures 2 & 3. Cardiac MRI: Top row (2-chamber long axis figure 2, LVOT view figure 3) shows the mitral valve prolapse, the degree of mitral annular disjunction (MAD) as well as the jet of mitral regurgitation (MR).

Video 1. Cardiac MRI 4-Chamber View
Video 2. Cardiac MRI 3-Chamber View
Video 3. Cardiac MRI 2-Chamber View
Video 1-3. Cardiac MRI 4ch, 3ch and 2ch views respectively show the mitral valve prolapse, the mitral annular disjunction as well as the jet of mitral regurgitation.
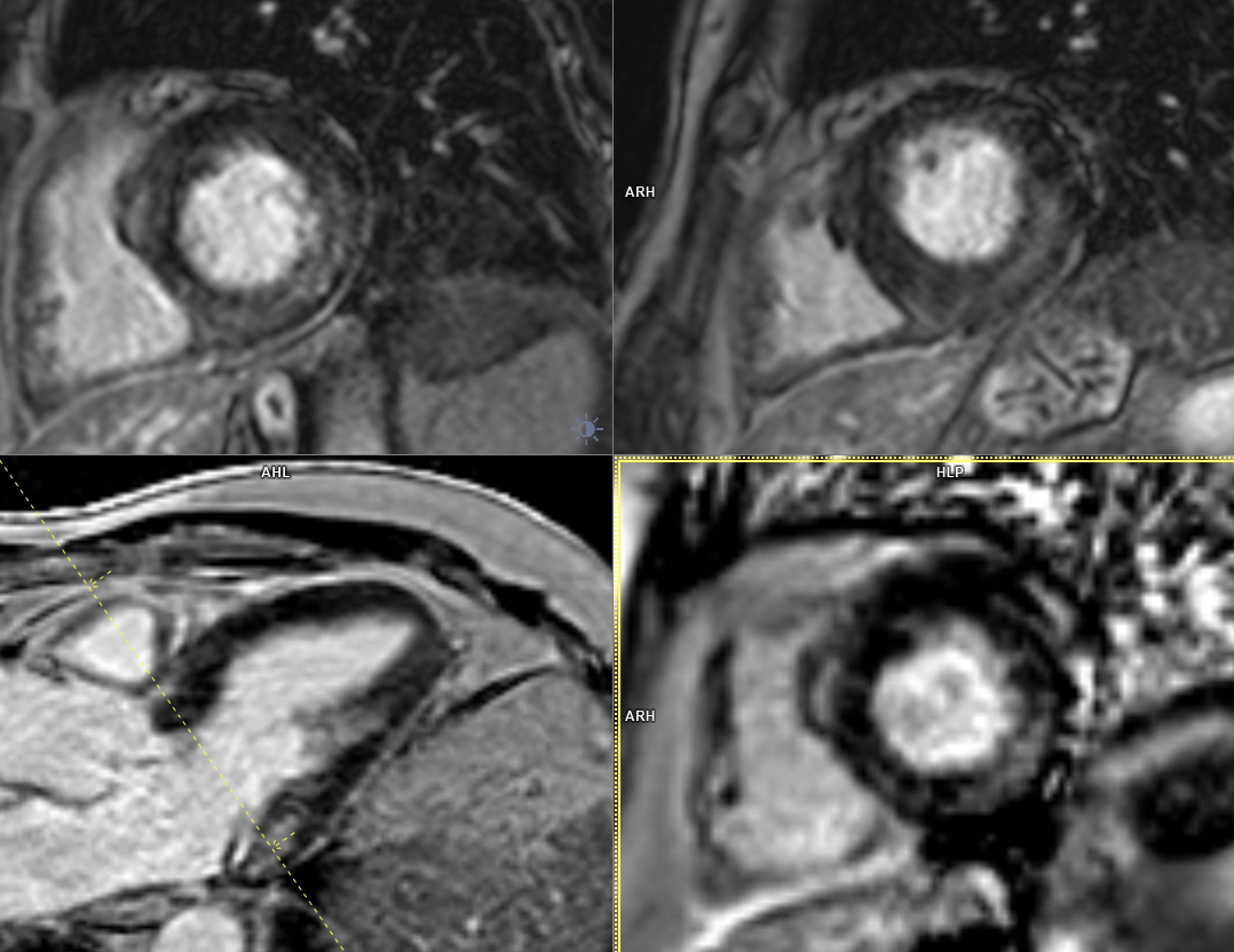
Figure 4. Cardiac MRI: late enhancement sequence in short axis and LVOT views shows the fibrosis area in the lateral wall basal segment.
Conclusion:
In conclusion,the pattern of ventricular hypertrophy was not typical for HCM. MRI diagnosis was MVP, MAD and focal annular myocardial fibrosis. ECG monitoring was recommended after cardiac MRI.
Perspective:
The mitral annulus is a fibro-cartilagenous structure. MVP is bowing with a displacement of > 2 mm of mitral leaflets into the left atrium, beyond annular plane. The pathology of mitral degeneration includes chronic activation of the valvular interstitial cells as well as the degradation of the collagen and elastin of the mitral valve by proteolytic enzymes.Histopathological types of mitral degeneration include Barlow’s disease; which is the classic type, and the Fibroelastic type which leads to mitral annulus disjunction (MAD). MAD is the separation of the atrio-mitral valve (MV) junction from the left ventricular attachment allowing for increased mobility of the MV apparatus (1).MAD by itself is considered arrhythmiogenic (2). Echocardiography can usually detect MVP and any associated mitral regurgitation.MRI clearly demonstrates the degree of MVP (3,4) and MAD as well as the hyperdynamic basal lateral wall the basal segments’ mild focal hypertrophy. This ASH on echocardiography may simulate a pattern of HCM. Moreover, MRI is capable of depicting further important surrogates for instance fibrosis. The combination of MVP, MAD and focal fibrosis increases the risk of fatal heart rhythm in those patients.
The triad of MAD, MVP and focal fibrosis is arrhythmiogenic, and could represent a fatal triad. It is therefore paramount to early recognise it especially in young patients using the different imaging modalities (5). Further studies are recommended to determine whether monitoring younger patients using CMR would be essential.
Click here to view the case on CloudCMR.
References:
1. Dejgaard LA, Skjølsvik ET, Lie ØH, Ribe M, Stokke MK, Hegbom F, Scheirlynck ES, Gjertsen E, Andresen K, Helle-Valle TM, Hopp E, Edvardsen T, Haugaa KH. The Mitral Annulus Disjunction Arrhythmic Syndrome. J Am Coll Cardiol. 2018 Oct 2;72(14):1600-1609, https://www.onlinejacc.org/content/72/14/1600.
2. Perazzolo Marra M, Basso C, De Lazzari M, Rizzo S, Cipriani A, Giorgi B, Lacognata C, Rigato I, Migliore F, Pilichou K, Cacciavillani L, Bertaglia E, Frigo AC, Bauce B, Corrado D, Thiene G, Iliceto S.Perazzolo Marra M, et al. Morphofunctional Abnormalities of Mitral Annulus and Arrhythmic Mitral Valve Prolapse. Circ Cardiovasc Imaging. 2016;9(8):e005030. https://www.ahajournals.org/doi/full/10.1161/circimaging.116.005030
3. Han Y, Peters DC, Salton CJ, Bzymek D, Nezafat R, Goddu B, Kissinger KV, Zimetbaum PJ, Manning WJ, Yeon SB.Han Y, et al. JACC Cardiovasc Imaging. Cardiovascular magnetic resonance characterization of mitral valve prolapse. JACC Cardiovasc Imaging. 2008. PMID: 19356441.https://imaging.onlinejacc.org/content/jimg/1/3/294.full.pdf
4. Pradella S, Grazzini G, Brandani M, Calistri L, Nardi C, Mori F, Miele V, Colagrande S, et al. Cardiac magnetic resonance in patients with mitral valve prolapse: Focus on late gadolinium enhancement and T1 mapping. Eur Radiol. 2019 Mar;29(3):1546-1554.https://pubmed.ncbi.nlm.nih.gov/30088066/
5. Marc A Miller, Srinivas R Dukkipati, Mohit Turagam , Steve L Liao, David H Adams 5 , Vivek Y Reddy. Arrhythmic Mitral Valve Prolapse: JACC. 2018 ; 11;72(23 Pt A):2904-2914.www.onlinejacc.org/content/72/23_Part_A/2904
Case prepared by:
Ahmed Kharabish, MD
Associate Editor, SCMR Case of the Week
Radiology Department, Cairo University Hospitals, Cairo, Egypt
Madhusudan Ganigara, MD
Associate Editor, SCMR Case of the Week
Cohen Children’s Medical Center of New York – Hofstra Northwell School of Medicine, New York.





